Topical carbonic anhydrase inhibitors (CAIs) such as brinzolamide 1% (Azopt; Alcon Laboratories, Fort Worth, TX, USA) attenuate bicarbonate efflux, and this may lead to corneal oedema.
To our knowledge, this is the first report of complete resolution of corneal oedema after cessation of topical brinzolamide 1%.
CASE REPORTS
A 57 year old African-American man with primary open angle glaucoma (POAG) presented with painless blurry vision left eye 1 hour after instilling brinzolamide 1% in both eyes. He had been on brinzolamide 1% both eyes twice daily, brimonidine tartrate 0.2% (Alphagan) in both eyes twice daily, and latanoprost 0.005% (Xalatan) in both eyes once at night for 2 years. On presentation, best corrected visual acuity (BCVA) was 20/25 right eye and 20/50 left eye. The left eye had mild corneal oedema, Descemet’s folds, and whitish fleck-like debris on the corneal endothelium (fig 1A). Intraocular pressures (IOPs) were 15 mm Hg and 16 mm Hg. The brinzolamide 1% in both eyes was discontinued. Timolol maleate 0.5% (Timoptic) in both eyes twice daily and topical prednisolone acetate 1% (Pred Forte) left eye four times daily were started. By 1 week follow up, the cornea was clear (fig 1B). Specular microscopy revealed endothelial cell counts (ECC) of 1355 cells/mm2 right eye and 648 cells/mm2 left eye with enlarged pleomorphic endothelial cells left eye (fig 2). Central corneal thickness (CCT) was measured as 512 μm right eye and 505 μm left eye.
Figure 1.
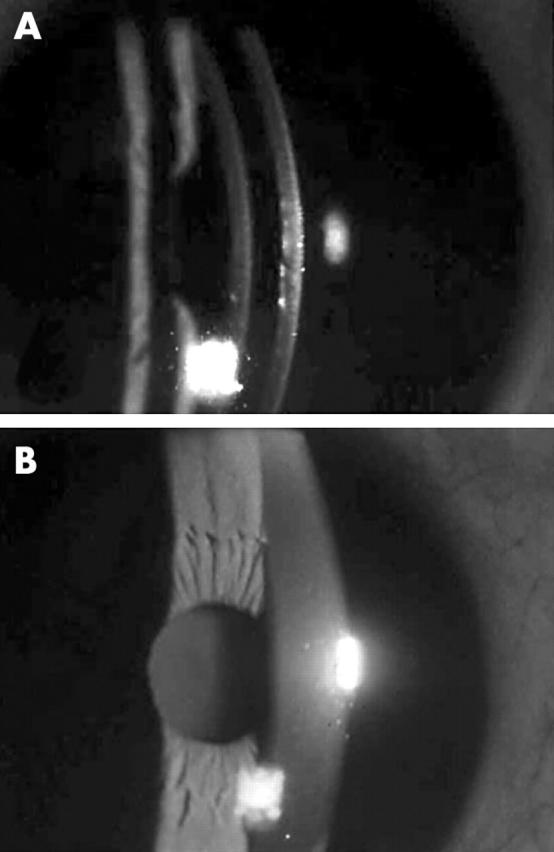
Case 1. (A) Corneal oedema left eye with Descemet’s folds 10 hours after the last dose of topical brinzolamide 1%. (B) Corneal oedema completely resolved 7 days after discontinuing brinzolamide 1% with minimal guttata noted.
Figure 2.
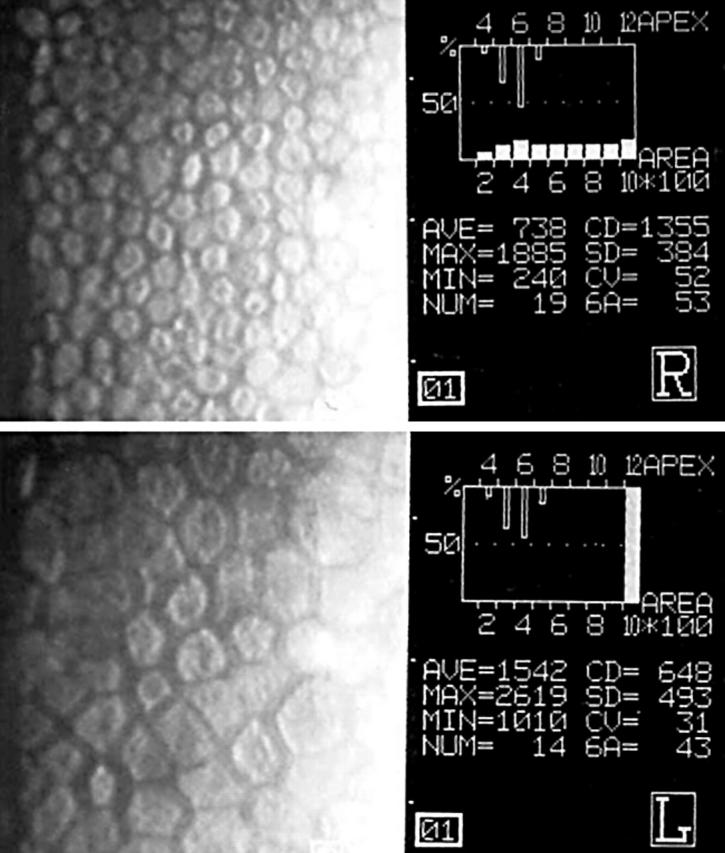
Case 1. Specular microscopy showing an ECC of 1355 cells/mm2 right eye and 648 cells/mm2 with pleomorphic cells left eye.
A 77 year old white man, who had had cataract extraction 46 years earlier and subsequent aphakia right eye, had been followed for open angle glaucoma in both eyes for 25 years. He was on timolol maleate 0.5% in both eyes twice daily, latanoprost 0.005% in both eyes once at night, and pilocarpine hydrochloride 4% gel (Pilopine Gel HS) in both eyes once at night. His visual acuities were hand movement right eye and counting fingers at 1 foot left eye. An IOP of 19 mm Hg right eye and 10 mm Hg left eye necessitated the addition of brinzolamide 1% twice daily right eye. Both corneas were clear at that time. Fifteen months after starting brinzolamide 1%, there was moderate corneal oedema right eye. Brinzolamide 1% was discontinued. Over 3 months, the corneal oedema in the right eye gradually resolved. The patient later needed trabeculectomy with mitomycin C right eye because of medically uncontrolled IOP.
COMMENT
The Merck Worldwide Adverse Experience System database for dorzolamide 2% includes 25 reports of corneal oedema. Nearly all of these cases had a history of multiple ocular surgeries and compromised corneas.1
Dorzolamide is a reversible inhibitor of carbonic anhydrase II and does not accumulate in the cornea with repeat dosing,2 so any corneal effect from a similar medication should indeed be potentially reversible.1 Dorzolamide’s peak concentration in rabbit corneas is also reached 1 hour after dosing, and the half life in the cornea is approximately 2 hours.3 This is consistent with case 1 having blurry vision 1 hour after instilling brinzolamide 1%.
Patients with primary open angle glaucoma or ocular hypertension and a baseline ECC of greater than 1500 cells/mm2 have an average 3.6% decrease in ECC after a year of dorzolamide 2% three times daily.4 This endothelial loss is much higher than the 0.6% annual rate seen in normal subjects.5
Topical CAIs can cause corneal oedema in compromised corneas—for example, those with cornea guttata,6 but the oedema is reversible if identified early. Before initiating brinzolamide 1%, an ECC may be needed for high risk patients (that is, monocular, previous ocular surgery, corneal disease, etc). Because of the potentially irreversible nature of the corneal decompensation,7 topical CAIs may be relatively contraindicated in patients with significant corneal disease.
Although dorzolamide and brinzolamide are both topical CAIs, their chemical formulas are different, and a side effect that is associated with dorzolamide may not necessarily be assumed to be associated with brinzolamide. It is important to be aware that brinzolamide can also potentially cause corneal oedema.
REFERENCES
- 1.Adamsons I. Irreversible corneal decompensation in patients treated with topical dorzolamide. Am J Ophthalmol 1999;128:774–6. [DOI] [PubMed] [Google Scholar]
- 2.Sugrue MF, Johns B. Concentrations of dorzolamide in the pigmented rabbit eye after repeated dosing with Trusopt. Invest Ophthalmol Vis Sci 1999;40 (Suppl) :S171. [Google Scholar]
- 3.Sugrue MF, Harris A, Adamsons I. Dorzolamide hydrochloride: a topically active, carbonic anhydrase inhibitor for the treatment of glaucoma. Drug of Today 1997;33:283–98. [Google Scholar]
- 4.Lass JH, Khosrof SA, Laurence JK, et al. A double-masked randomized, 1-year study comparing the corneal effects of dorzolamide, timolol, and betaxolol. Arch Ophthalmol 1998;116:1003–10. [DOI] [PubMed] [Google Scholar]
- 5.Bourne WN, Nelson LR, Hodge DO. Central corneal endothelial cell changes over ten-year period. Invest Ophthalmol Vis Sci 1997;38:779–82. [PubMed] [Google Scholar]
- 6.Wirtitsch MG, Findl O, Kiss B, et al. Short-term effect of dorzolamide hydrochloride on central corneal thickness in humans with cornea guttata. Arch Ophthalmol 2003;121:621–5. [DOI] [PubMed] [Google Scholar]
- 7.Konowal A, Morrison JC, Brown SV, et al. Irreversible corneal decompensation in patients treated with topical dorzolamide. Am J Ophthalmol 1999;127:403–6. [DOI] [PubMed] [Google Scholar]


