Abstract
Aim: To evaluate the properties of devices for measuring stray light and glare: the Nyktotest, Mesotest, “conventional” stray light meter and a new, computer implemented version of the stray light meter.
Methods: 112 subjects, divided in three groups: (1) young subjects without any eye disease; (2) elderly subjects without any eye disease, and (3) subjects with (early) cataract in at least one eye. All subjects underwent a battery of glare and stray light tests, measurement of visual acuity, contrast sensitivity, refraction, and LOCS III cataract classification. Subjects answered a questionnaire on perceived disability during driving.
Results: Repeatability values were similar for all glare/stray light tests. Validity (correlation with LOCS III and questionnaire scores), discriminative ability (ability to discriminate between the three groups), and added value (to measurement of visual acuity and contrast sensitivity) were all superior for both stray light meters. Results of successive measurements are interrelated for the conventional but not the new stray light meter. This indicates a better resistance to fraud for the latter device.
Conclusions: The new computer implemented stray light meter is the most promising device for future stray light measurements.
Keywords: vision tests, glare, driving, cataract
Disability glare is the reduction in visual performance, caused by veiling luminance on the retina. It is an effect of intraocular stray light. Measurements of glare and stray light are particularly important for drivers,1–3 cataract,4–6 and refractive surgery.7–14 Glare testing in the elderly may be important in view of the high accident rates in this age group,15 especially at night.16 Moreover, glare measurements may predict future decrease of visual acuity.17
Over the years, many glare testers have been developed. Most of these measure either visual acuity or contrast sensitivity in the presence of a glare source. None of these has evolved into a universally accepted standard.18–20 The stray light meter21–23 provides a direct measure of intraocular stray light, instead of measuring the effect on perception. It is therefore considered the current “gold standard,” but it is, as yet, suited for laboratory use only.24 The design of the equipment does not allow implementation in a setting in which fraud resistance is essential.
Glare measurements for drivers are advocated by the German Ophthalmological Society.2 The guidelines are based on the classic study of Aulhorn and Harms.25 This led to the development of the Nyktometer and the Mesotest. Although widely used,25–30 the properties of these devices (reproducibility, validity, and discriminative ability) have been scarcely investigated.31–33
In the current study, we compared the properties of several stray light and glare test devices. Apart from the stray light meter, the Nyktotest, and Mesotest, a new, computer implemented version of the stray light meter was included that, intentionally, does not have several of the drawbacks of the original device.
METHODS
Subjects
A cross sectional cohort of 112 subjects was drawn from the patients and visitors of the three participating clinics. Subjects belonged to one of the following groups:
The young group: between 20 and 40 years of age, no ocular disease, corrected visual acuity (VA) equal to or better than 0.1 logMAR (Snellen acuity 20/25) in both eyes (n = 40);
The elderly group: 50 years of age and over, corrected VA in both eyes equal to or better than 0.1 logMAR, minimal cataract at most, no other ocular disease (n = 37);
The cataract group: binocular VA equal to or better than 0.2 (Snellen acuity 20/32), clinically relevant cataract in at least one eye, no other eye disease (n = 35). Subjects had no more than 6 dioptres of myopia, 5 dioptres of hyperopia, and/or 1.5 dioptres of astigmatism. In half of the subjects, glare and stray light measurements were repeated on a different day, to allow repeatability calculations.
Questionnaire
Before testing, subjects were asked to answer a questionnaire, containing questions about visual disability experienced during driving.34
Measurement of visual function
Visual acuity (VA) was measured with the ETDRS chart on a logMAR scale,35,36 using best corrected visual acuity (BCVA), according to the modified ETDRS protocol from the AREDS study37; contrast sensitivity (CS) was determined using the Pelli-Robson chart,38–40 with BCVA and, for subjects of 40 years and over, a near addition of +0.75 and expressed as log(contrast sensitivity). Stray light was measured, using the conventional stray light meter (CSLM).21–23 The right and left eyes were measured, using trial glasses as instructed by the designer (may be obtained from the authors), to correct for refraction errors. In addition, stray light was measured using the new (computer implemented) stray light meter (NSLM). This device differs from the CSLM in that the turning knob does not have an end stop and the luminance of the central detection field is kept constant. These modifications aimed at enhancing fraud resistance by eliminating cues, other than detection of flicker in the measurement fields. In addition, the NSLM may be used binocularly, because the subject looks at a computer screen rather than in a (monocular) test tube. Subjects wore trial glasses with their BCVA, with near addition according to age. Measurements were performed for right and left eyes and binocularly. Stray light measurements consisted of the average of three knob settings and were expressed as log(stray light parameter). CSLM and NSLM were performed with “normal” pupils at room light as well as with pharmacologically “dilated” pupils (one drop of tropicamide 0.5%). Mesopic contrast sensitivity and glare sensitivity were measured using the Mesotest II25 (Oculus, GmbH, Wetzlar, Germany) and the Nyktotest 30030 (with both 501 and 502 test discs, Rodenstock, GmbH, Ottobrunn, Germany) and expressed as level, corresponding to log(percentage contrast). The Nyktotest 300 has a brighter illumination of the background than the Mesotest. According to the instructions of the manufacturer, Mesotest measurements were the average of five subsequent readings. The Nyktotest has only one reading per level, therefore each measurement consisted of one reading only. For the Nyktotest, levels 1–8 correspond to log(percentage contrast) of, respectively, 0.02, 0.1, 0.2, 0.3, 0.4, 0.5, 0.7, and 0.92. For the Mesotest, levels 1–4 correspond to log(percentage contrast) of, respectively, 0.02, 0.1, 0.2, and 0.3.
Definition of impaired
Visual acuity was considered impaired when higher than 0.3 logMAR (Snellen acuity lower than 20/40); stray light when the log(s) parameter was higher than 1.4; contrast sensitivity when the log(contrast sensitivity) was less than 1.25,41 Nyktotest and Nyktotest with glare when more than 40% contrast was needed, corresponding to level 5,30 and Mesotest and Mesotest with glare when more than 20% contrast was needed, corresponding to level 2 (DOG recommendations for class 1 drivers2).
Quantification of cataract
Cataract was quantified using the LOCS III lens classification.42
Statistical analysis
The statistical analysis was performed using SPSS for Windows PC, release 9.0.0.
RESULTS
Repeatability
The level of agreement between repeated measurements can be expressed as repeatability coefficient RC = 2 × SD of differences between repeated measurements.43 The Nyktotests and Mesotests have a minimum and a maximum score that is being achieved by many subjects. For example, for the right eyes, minimum or maximum scores were reached in 29 and six subjects for the Nyktotests and Mesotests without glare and in 28 and 26 subjects for the Nyktotests and Mesotest with glare, respectively (see also fig 1). Therefore, many scores are “arbitrarily” fixed on the minimum and maximum values. This truncation of scores artificially improves the repeatability.44 To correct for this effect, in the analysis we removed the maximum and minimum scores on the Nyktotest and Mesotest, both with and without glare. (see table 1: “RC, correction for truncations”).
Figure 1.
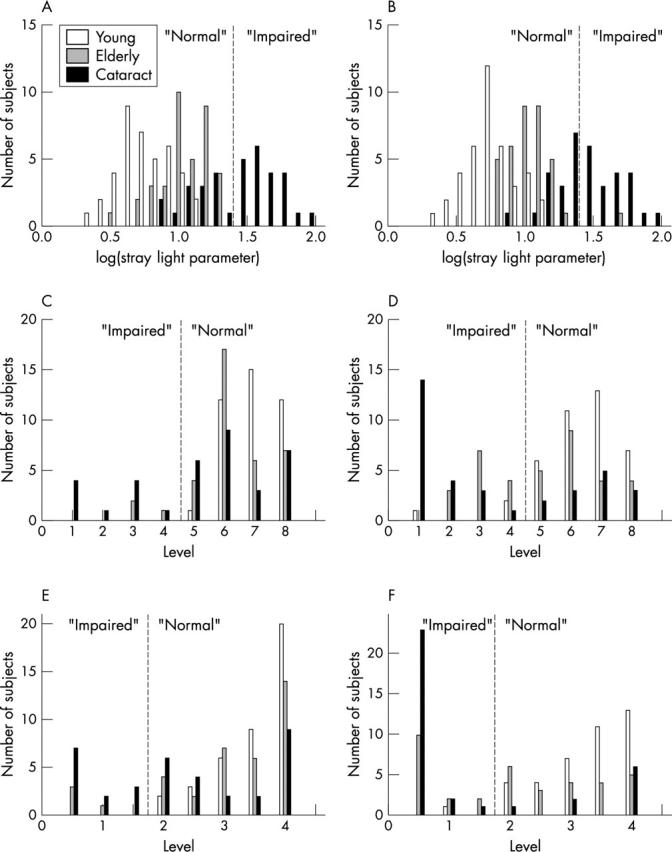
Distribution of data for each of the tests. (A) Conventional stray light meter. (B) New stray light meter. (C) Nyktotest without glare. (D) Nyktotest with glare. (E) Mesotest without glare. (F) Mesotest with glare. Note that the vertical scaling differs between panels. For the CSLM and NSLM, there are hardly any “normal” young or elderly subjects who display “impaired” test results (low false positives). Some elderly (and young) subjects display “impaired” results on the Nyktotest and Mesotest without glare, and even more so on the Nyktotest and Mesotest with glare (higher false positives). Results are shown for right eyes only. Results for left eyes and binocular tests are similar.
Table 1.
Repeatability coefficients (RC) and related parameters (n = 49–55)
| Test | RC | RC′ corrected for truncations | Range (RNG) | Ratio RC′/RNG |
| Right eye | ||||
| Conventional stray light meter | 0.34 | id‡ | 1.29 | 0.26 |
| New stray light meter | 0.27 | id | 1.30 | 0.21 |
| Nyktotest | 1.72 | 1.905 | 7 | 0.27 |
| Mesotest | 1.05 | 1.174 | 4 | 0.29 |
| Nyktotest with glare | 2.37 | 2.809 | 8 | 0.35 |
| Mesotest with glare | 0.96 | 1.170 | 4 | 0.29 |
| Visual acuity | 0.2u* | id | 0.7U | 0.29 |
| Contrast sensitivity | 0.15u† | id | 1.2 | 0.13 |
| Left eye | ||||
| Conventional stray light meter | 0.36 | id | 1.35 | 0.27 |
| New stray light meter | 0.31 | id | 1.50 | 0.21 |
| Nyktotest | 1.58 | 1.711 | 7 | 0.24 |
| Mesotest | 0.99 | 1.125 | 4 | 0.31 |
| Nyktotest with glare | 2.11 | 2.406 | 8 | 0.30 |
| Mesotest with glare | 0.97 | 1.184 | 4 | 0.46 |
| Visual acuity | 0.2u* | id | 0.7U | 0.29 |
| Contrast sensitivity | 0.15u† | id | 1.15 | 0.13 |
| Both eyes | ||||
| New stray light meter | 0.29 | id | 1.17 | 0.25 |
| Nyktotest | 1.47 | 1.728 | 6 | 0.29 |
| Mesotest | 0.55 | 0.655 | 4 | 0.16 |
| Nyktotest with glare | 1.52 | 1.641 | 8 | 0.20 |
| Mesotest with glare | 1.41 | 1.673 | 4 | 0.41 |
| Visual acuity | 0.2u* | id | 0.5U | 0.4 |
| Contrast sensitivity | 0.15† | id | 0.9 | 0.17 |
The repeatability, expressed as RC/RNG, is similar for all tests, although monocular values for the NSLM tend to be lower than those of the remaining glare/stray light tests. Values for contrast sensitivity are lower than those for glare and stray light tests
*From Elliott and Sheridan45; †From Elliott et al40; ‡id, no correction for truncations (RC′ identical to RC). Note that all values are on a log scale, including the ones for visual acuity. For visual acuity, 0.1 log unit corresponds to one line on the visual acuity chart.
To allow for comparison of values between tests that use different measurement units, we calculated the ratio between RC′ and the range of measurement values that was obtained. The ratio RC′/RNG hardly differs between the tests (table 1). Ratios are lower only for contrast sensitivity, caused by the wide range of scores obtained with the Pelli-Robson chart.
For none of the tests was there a significant relation between repeatability and test score (regression analysis, all p values larger than 0.24). There was no dependency of repeatability coefficients on the subject group (analysis of variance; all p values ranging from 0.20 to 0.84).
Validity
The validity of a test indicates the extent to which the test outcome is related to a reference variable in our study: the LOCS III lens classification and the questionnaire. We found the highest correlations for the CSLM and, to a lesser extent, the NSLM (table 2). We studied the correlation between test outcomes and single parameters of both LOCSIII (NO, NC, C, and P) and the questionnaire (single questions); these were similar to those of the overall scores. Therefore, only the overall scores are being reported. Since the CLSM in the literature is considered the gold standard, we also investigated the relation of test outcomes to the CLSM. These correlations were highest for the NSLM.
Table 2.
Validity: Pearson’s correlation coefficients between tests and reference variables: CSLM, LOCSIII, and the questionnaire (n = 112)
| Test | Reference variable | |||
| Conventional stray light meter | LOCS III lens classification | Questionnaire (average score) | ||
| Right eye | ||||
| Conventional stray light meter | Undilated pupils | – | 0.763 | 0.454 |
| Dilated pupils | – | 0.702 | 0.474 | |
| New stray light meter | Undilated pupils | 0.635 | 0.650 | 0.313 |
| Dilated pupils | 0.711 | 0.609 | 0.346 | |
| Nyktotest | −0.471 | −0.479 | −0.244 | |
| Nyktotest with glare | −0.436 | −0.397 | −0.249 | |
| Mesotest | −0.449 | −0.495 | −0.205 | |
| Mesotest with glare | −0.465 | −0.486 | −0.247 | |
| Left eye | ||||
| Conventional stray light meter | Undilated pupils | – | 0.751 | 0.483 |
| Dilated pupils | – | 0.689 | 0.456 | |
| New stray light meter | Undilated pupils | 0.705 | 0.658 | 0.355 |
| Dilated pupils | 0.709 | 0.538 | 0.420 | |
| Nyktotest | −0.561 | −0.536 | −0.298 | |
| Nyktotest with glare | −0.516 | −0.505 | −0.318 | |
| Mesotest | −0.548 | −0.513 | −0.293 | |
| Mesotest with glare | −0.508 | −0.534 | −0.293 | |
| Both eyes | ||||
| New stray light meter | – | – | 0.415 | |
| Nyktotest | – | – | −0.312 | |
| Nyktotest with glare | – | – | −0.334 | |
| Mesotest | – | – | −0.266 | |
| Mesotest with glare | – | – | −0.319 | |
The LOCS III score was the average of all four LOCS III parameters. The questionnaire score was the average score of all five questions. The scores on the CSLM and, to a lesser extent, the NSLM, are closest related to the results of the LOCS III classification and the questionnaire. The correlations between CSLM/NSLM and LOCSIII for dilated pupils are no better than those for undilated pupils. All correlation coefficients were statistically significant (p<0.05).
Dilated pupils
The LOCS III lens classification evaluates the properties of the entire lens, the effects of glare and stray light are clustered around the optical axis. This difference may have affected the relation between the two. Therefore, we measured stray light with dilated pupils. We found that the correlations between the CSLM/NSLM, as measured with dilated pupils, and the LOCS III lens classification are no better than those for undilated pupils (table 2).
Discriminative ability
We investigated to what extent the devices could discriminate between our groups. For the CLSM and NSLM, there are no young subjects who display impaired test results (fig 1A, B). There is only one elderly subject with an impaired NSLM result. For Nyktotests and Mesotests (fig 1C–F), several normal elderly subjects display impaired test results, for the with glare condition (fig 1E, F), even some young subjects display impaired results (false positives). For all tests, several subjects from the cataract group display non-impaired results These may not be considered false negatives because cataract can, but not necessarily does, lead to increased stray light/glare values.
Receiver operating characteristics
Table 3 shows the area under the curve of the receiver operating characteristics (ROCs) for comparisons between groups. For all comparisons (cataract versus no cataract; cataract versus elderly; young versus elderly), the results were best for the NSLM. Values for the stray light meters were similar to those for visual acuity and contrast sensitivity. Note that values for VA may be artificially high, because this was a selection criterion of the study. The high values for the LOCS III classification may be caused by the fact that lens opacification, as observed at the slit lamp, was one of the criteria for group assignment.
Table 3.
Values* of “area under the curve” of the receiver operating characteristics (n = 112)
| Test | Groups for comparison | ||
| Cataract versus no cataract (young and elderly) | Cataract versus elderly without cataract | Elderly versus young | |
| Right eye | |||
| Conventional stray light meter | 0.881 | 0.836 | 0.774 |
| New stray light meter | 0.916 | 0.871 | 0.771 |
| Nyktotest | 0.682 | 0.632 | 0.659 |
| Mesotest | 0.697 | 0.658 | 0.613 |
| Nyktotest with glare | 0.736 | 0.695 | 0.680 |
| Mesotest with glare | 0.764 | 0.716 | 0.756 |
| Visual acuity | 0.784 | 0.748 | 0.533 |
| Contrast sensitivity | 0.810 | 0.767 | 0.547 |
| LOCS III lens classification | 0.929 | 0.887 | 0.851 |
| Left eye | |||
| Conventional stray light meter | 0.897 | 0.847 | 0.725 |
| New stray light meter | 0.881 | 0.825 | 0.792 |
| Nyktotest | 0.693 | 0.640 | 0.629 |
| Mesotest | 0.719 | 0.703 | 0.525 |
| Nyktotest with glare | 0.750 | 0.704 | 0.683 |
| Mesotest with glare | 0.772 | 0.713 | 0.756 |
| Visual acuity | 0.846 | 0.822 | 0.526 |
| Contrast sensitivity | 0.897 | 0.864 | 0.594 |
| LOCS III lens classification | 0.957 | 0.928 | 0.846 |
| Both eyes | |||
| New stray light meter | 0.895 | 0.848 | 0.832 |
| Nyktotest | 0.737 | 0.676 | 0.638 |
| Mesotest | 0.693 | 0.666 | 0.584 |
| Nyktotest with glare | 0.794 | 0.745 | 0.674 |
| Mesotest with glare | 0.813 | 0.763 | 0.762 |
| Visual acuity | 0.839 | 0.809 | 0.567 |
| Contrast sensitivity | 0.915 | 0.871 | 0.547 |
| Questionnaire | 0.867 | 0.832 | 0.576 |
*A value of 0.5 indicates a random test; the closer to 1, the better the discriminative ability of the test
Resistance to fraud: the CSLM and NSLM
For the CSLM, within measurement variability was lower than between measurement variability, indicating that successive measurements are related. This makes the device prone to fraud. This difference is not present for the NSLM (table 4).
Table 4.
Within and between measurement repeatability for the CSLM and the NSLM (n = 49–55)
| Test | Repeatability coefficient | |
| Within measurements | Between measurements | |
| Conventional stray light meter | 0.282 | 0.430 |
| New stray light meter | 0.489 | 0.394 |
For the CSLM, “within” values are better than “between” values, indicating that successive measurements are related. For the NSLM, “within” values are not better than between values, suggesting that successive measurements are independent. Values are higher than values in table 1, because values in this table reflect the repeatability of single knob settings and values in table 1 reflect repeatability of measurements, consisting of three knob settings
Added value of a test
We investigated to what extent each of the glare tests provide information, additional to that acquired from visual acuity and contrast sensitivity. Furthermore, we studied to what extent visual acuity and contrast sensitivity provide information that is not being provided by the glare tests. We assumed our a priori group assignment as reference.
In the absence of any covariants, all tests provide information about differences between groups (table 5A, B). If VA and CS are covariants, only the CSLM, NSLM, and Nyktotest and Mesotest with glare provide information about differences between groups (table 5C). In all comparisons, F values for the CSLM and NSLM are highest.
Table 5.
ANOVA statistics for the discrimination between the three groups: young/elderly/cataract (n = 112)
| Dependent | Covariants | Right eye | Left eye | Both eyes | |||
| F | P | F | P | F | P | ||
| (A) Visual acuity and contrast sensitivity | |||||||
| Visual acuity | None | 19.48 | <0.001 | 27.91 | <0.001 | 27.17 | <0.001 |
| Contrast sensitivity | None | 24.32 | <0.001 | 46.63 | <0.001 | 32.87 | <0.001 |
| (B) Glare/stray light | |||||||
| Conventional stray light meter | None | 53.41 | <0.001 | 49.88 | <0.001 | NA | NA |
| New stray light meter | None | 69.51 | <0.001 | 63.80 | <0.001 | 63.78 | <0.001 |
| Nyktotest | None | 11.66 | <0.001 | 14.31 | <0.001 | 16.31 | <0.001 |
| Mesotest | None | 13.04 | <0.001 | 12.57 | <0.001 | 12.61 | <0.001 |
| Nyktotest with glare | None | 20.31 | <0.001 | 22.34 | <0.001 | 28.50 | <0.001 |
| Mesotest with glare | None | 25.77 | <0.001 | 26.28 | <0.001 | 35.50 | <0.001 |
| (C) Glare/stray light with co-variants | |||||||
| Conventional stray light meter | Visual acuity, contrast sensitivity | 15.88 | <0.001 | 8.11 | 0.001 | NA | NA |
| New stray light meter | Visual acuity, contrast sensitivity | 31.36 | <0.001 | 23.39 | <0.001 | 29.69 | <0.001 |
| Nyktotest | Visual acuity, contrast sensitivity | 2.07 | 0.131 | 0.62 | 0.539 | 4.47 | 0.014 |
| Mesotest | Visual acuity, contrast sensitivity | 3.10 | 0.049 | 0.73 | 0.486 | 2.28 | 0.107 |
| Nyktotest with glare | Visual acuity, contrast sensitivity | 8.49 | <0.001 | 5.04 | 0.008 | 14.18 | <0.001 |
| Mesotest with glare | Visual acuity, contrast sensitivity | 11.64 | <0.001 | 9.92 | <0.001 | 17.09 | <0.001 |
In absence of any covariant (A and B), all tests discriminate between the groups. If visual acuity and contrast sensitivity are covariant (C), only the stray light meters and the Nyktotests and Mesotests with glare discriminate between the groups. In all comparisons, F values are highest for the CSLM and NSLM
DISCUSSION
Many authors have favoured the measurement of glare sensitivity for assessing the visual capacity of drivers and for evaluating cataract, but currently it is not included in the directive of the European Union.46 A possible inclusion of a glare or stray light test is hampered by the absence of a universally accepted, fraud resistant measurement technique. In this study we systematically investigated various aspects of several glare and stray light tests. Knowledge about these aspects is crucial before a widespread introduction of one or more of these tests may be taken into consideration.
We found that various aspects such as validity, discriminative ability, and added value are superior for the stray light meters. It may be noted that this device provides a measure of intraocular stray light, which is the cause of glare. Other devices, such as Nyktotests and Mesotests, but also other commercially available glare testers, measure the effect of glare on perception (contrast sensitivity). This effect is largely dependent on the specific measurement conditions. It may be that these conditions do not represent the conditions in daily life when glare is perceived. Apparently, this counts even for devices such as Nyktotests and Mesotests, in which traffic conditions are simulated. Notably, our questionnaire contained questions specifically directed at night time driving. Even the results of our questionnaire were better correlated with the stray light meters than with the Nyktotests and Mesotests. The fact that the stray light meters performed best in our experiments also indicates that intraocular stray light is well correlated with the detrimental effects of glare on perception.
Repeatability
We found that repeatability values, in relation to the range of measurement values, were about similar for all tests. Repeatability coefficients in relation to range of values for contrast sensitivity were much lower, owing to the wide range of measurement values that was obtained with this test. Because this wide range is mainly caused by outliers, this does not necessarily increase the reliability of this test. For the stray light meters, repeatability can probably be improved by changing the measurement strategy into a forced choice method. This is a topic of future study.
The Nyktometer is similar in design to the Nyktotest and similar in test conditions to the Mesotest. Hartmann and Wehmeyer26 investigated the repeatability of the Nyktometer in a study that involved nine subjects, who performed 18 measurements each. The authors found that the SD of the mean of these measurements was at the 0.75 level. Rassow,30 evaluating the Nyktotest, found an accuracy at a plus or minus 1 level. These results agree well with our results: we found an SD of 0.67 for the Nyktotest without glare and 0.70 with glare.
We note that for the Nyktotests and Mesotests, there is only a small distance between the average normal score and the recommended cut-off values. This counts for the young, but especially for the elderly group. (Expressed in units RC, distances were generally less than 1, compared to values of about 2 for visual acuity, contrast sensitivity and stray light meters.) With such small distances, misclassification of subjects (normal subjects being classified as impaired and vice versa) could easily occur. Hartmann and Wehmeyer concluded that this repeatability is “good.” Although we agree with the magnitude of the repeatability value, in view of the small difference between “normal” and “impaired” values, we consider this value low.
Discriminative ability
For the assessment of discriminative ability, we assumed our clinical group assignment as the reference variable. This group assignment was based on a constellation of signs and symptoms: the history of the subject, the clinical assessment of cataract by the ophthalmologist, and the visual acuity. Hence, this group assignment provides a clinical aggregation of the cataract assessment and perceived disability, similar to the LOCS III classification and questionnaire. The information of group assignment, LOCS III, and questionnaire therefore displays some overlap. Since group assignment is a discrete variable, it is particularly suited for discrimination studies. The low discriminative ability of the Nyktotests and Mesotests, particularly in the presence of glare, agrees with the literature: the high rate of false positives constitutes a major problem of these tests.32,34,47
Selection bias and misclassification
The subjects/participants in these experiments formed a non-random selection of the visitors to the outpatient departments of the involved clinics. Group assignment was made on the basis of clinical judgment. The primary intention of this study was to provide an analysis of the measurement devices that are currently available. Any selection bias only affects the concept of glare measurements, not the relation between the various measurement devices. The same counts for possible misclassification errors: elderly normal subjects who erroneously have been assigned to the cataract group and vice versa. These would have weakened the relation between test outcomes and reference variables, but not the relations between the various test devices. The inclusion criterion for the cataract group was a binocular visual acuity of at least 0.6. Although unlikely, it may be that relations between test outcomes and reference variables are different in subjects with lower visual acuities. We note that in such subjects, visual acuity itself is the most important parameter of visual function. Stray light and glare measurements are particularly important in subjects with early cataracts and only slightly decreased visual acuities. Our study demonstrates that in these subjects, measurement of stray light/glare does provide additional information and the stray light meter does discriminate between presence and absence of early cataract.
Glare and driving
Many investigators have promoted the use of glare measurement devices for assessing fitness for driving. Our research demonstrates that the stray light meter may be the device of choice for such assessment. However, before introducing any glare or stray light measurement, there should be a more thorough evaluation of the relation between increased stray light measurements and the detrimental effects on perception as well as an investigation of the prevalence of impaired values in the driving population.
Acknowledgments
This study was supported by grant I TREN E3 200/7/SI2.282.826 of the European Commission. The authors thank Rodenstock GmbH and Oculus GmbH for the provision of Nyktotests and Mesotests. TJTP van den Berg has a proprietary interest in the stray light meter; the remaining authors do not have any proprietary interest in any of the tests.
Abbreviations
BCVA, best corrected visual acuity
CS, contrast sensitivity
CSLM, conventional stray light meter
NSLM, new stray light meter
RC, repeatability coefficients
ROCs, receiver operating characteristics
VA, visual acuity
REFERENCES
- 1.Mäntyjärvi M, Tuppurainen K. Cataract in traffic. Graefes Arch Clin Exp Ophthalmol 1999;237:278–82. [DOI] [PubMed] [Google Scholar]
- 2.Deutsche Ophthalmologische Gesellschaft. Emfehlungen der Deutschen Ophthalmologischen Gesellschaft zur Fahreignungen für den Strassenverkehr. Heidelberg: Deutsche Ophthalmologische Gesellschaft, 1999.
- 3.Mainster MA, Timberlake GT. Why HID headlights bother older drivers. Br J Ophthalmol 2003;87:113–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adamsons I, Rubin GS, Vitale S, et al. The effect of early cataracts on glare and contrast sensitivity. A pilot study. Arch Ophthalmol 1992;110:1081–6. [DOI] [PubMed] [Google Scholar]
- 5.Eisenmann D, Jacobi FK, Dick B, et al. Glare sensitivity of phakic and pseudophakic eyes. Klin Monatsbl Augenheilkd 1996;208:87–92. [DOI] [PubMed] [Google Scholar]
- 6.Ruckhofer J, Grabner G. Driving behavior of patients before cataract operation--is an unlimited driver’s license justifiable? Results of an analysis of 1,124 patients of the ophthalmology department of a central hospital. Klin Monatsbl Augenheilkd 1998;212:106–10. [DOI] [PubMed] [Google Scholar]
- 7.Butuner Z, Elliott DB, Gimbel HV, et al. Visual function one year after excimer laser photorefractive keratectomy. J Refract Corneal Surg 1994;10:625–30. [PubMed] [Google Scholar]
- 8.Veraart HG, van den Berg TJ, IJspeert JK, et al. Stray light in radial keratotomy and the influence of pupil size and straylight angle. Am J Ophthalmol 1992;114:424–8. [DOI] [PubMed] [Google Scholar]
- 9.Veraart HG, van den Berg TJ, Hennekes R, et al. Stray light in photorefractive keratectomy for myopia. Doc Ophthalmol 1995;90:35–42. [DOI] [PubMed] [Google Scholar]
- 10.Niesen U, Businger U, Hartmann P, et al. Glare sensitivity and visual acuity after excimer laser photorefractive keratectomy for myopia. Br J Ophthalmol 1997;81:136–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghaith AA, Daniel J, Stulting RD, et al. Contrast sensitivity and glare disability after radial keratotomy and photorefractive keratectomy. Arch Ophthalmol 1998;116:12–18. [DOI] [PubMed] [Google Scholar]
- 12.Katlun T, Wiegand W. Change in twilight vision and glare sensitivity after PRK. Ophthalmologe 1998;95:420–6. [DOI] [PubMed] [Google Scholar]
- 13.Nagy ZZ, Munkacsy G, Krueger RR. Changes in mesopic vision after photorefractive keratectomy for myopia. J Refract Surg 2002;18:249–52. [DOI] [PubMed] [Google Scholar]
- 14.Fan-Paul NI, Li J, Miller JS, et al. Night vision disturbances after corneal refractive surgery. Surv Ophthalmol 2002;47:533–46. [DOI] [PubMed] [Google Scholar]
- 15.Massie DL, Green PE, Campbell KL. Crash involvement rates by driver gender and the role of average annual mileage. Accid Anal Prev 1997;29:675–85. [DOI] [PubMed] [Google Scholar]
- 16.Mortimer RG, Fell JC. Older drivers: their night fatal crash involvement and risk. Accid Anal Prev 1989;21:273–82. [DOI] [PubMed] [Google Scholar]
- 17.Schneck ME, Haegerstrom-Portnoy G. Practical assessment of vision in the elderly. Ophthalmol Clin N Am 2003;16:269–87. [DOI] [PubMed] [Google Scholar]
- 18.Van den Berg TPTP. On the relation between glare and straylight. Doc Ophthalmol 1991;78:177–81. [DOI] [PubMed] [Google Scholar]
- 19.Rubin GS. Amercian academy of ophthalmology report. contrast sensitivity and glare testing in the evaluation of anterior segment diseases. Ophthalmology 1990;97:1233–7. [DOI] [PubMed] [Google Scholar]
- 20.Elliot DB, Bullimore MA. Assessing the reliability, discriminative ability, and validity of disability glare tests. Invest Ophthalmol Vis Sci 1993;34:108–19. [PubMed] [Google Scholar]
- 21.Van den Berg TJTP, IJspeert JK. The straylightmeter. In: Technical Digest on Noninvasive Assessment of the Visual System. Washington, DC: OSA, 1, 1991:256–9.
- 22.Van den Berg TJTP, IJspeert JK. Clinical assessment of intraocular straylight. Appl Optics 1992;31:3694–6. [DOI] [PubMed] [Google Scholar]
- 23.Ijspeert JK, van den Berg TJTP. Design of a portable straylight Meter. Proceedings annual conference IEEE Engineering in Medicine and Biology Society 1992;14:1592–4. [Google Scholar]
- 24.Elliott DB, Hurst MA, Weatherill J. Comparing clinical tests of visual function in cataract with the patient’s perceived visual disability. Eye 1990;4:712–17. [DOI] [PubMed] [Google Scholar]
- 25.Aulhorn E, Harms H. Über die Untersuchung der Nachtfahreignung von Kraftfahrern mit dem Mesoptometer. Klin Monatsbl Augenheilkd 1970;157:843–73. [PubMed] [Google Scholar]
- 26.Hartmann E, Wehmeyer K. Untersuchung des Dämmerungssehens und des Blendempfindens met dem neuen Nyktometer. Klin Monatsbl Augenheilkd 1980;176:859–63. [DOI] [PubMed] [Google Scholar]
- 27.Scharwey K, Krzizok T, Herfurth M. Night driving capacity of ophthalmologically healthy persons of various ages. Ophthalmologe 1998;95:555–8. [DOI] [PubMed] [Google Scholar]
- 28.Lachenmayr B, Pateras N. [Twilight vision and glare sensitivity in pseudophakic eyes]. Fortschr Ophthalmol 1987;84:173–9. [PubMed] [Google Scholar]
- 29.Grosskopf U, Wagner R, Jacobi FK, et al. Twilight vision and glare sensitivity in monofocal and multifocal pseudophakia. Ophthalmologe 1998;95:432–7. [DOI] [PubMed] [Google Scholar]
- 30.Rassow B. Effect of luminance on contrast sensitivity and glare in the mesopic range. Klin Monatsbl Augenheilkd 1999;214:401–6. [DOI] [PubMed] [Google Scholar]
- 31.Von Hebenstreit B. Sehvermögen und Verkehrsunfälle. Klin Monatsbl Augenheilkd 1984;185:86–90. [PubMed] [Google Scholar]
- 32.Von Hebenstreit B. Untersuchungen zur Sehschärfe unter nächtlichen Fahrbedingungen im Strassenverkehr (dämmerungssehschärfe). Bayern: Unternehmensgruppe TUV, 1995.
- 33.Lachenmayr B, Berger J, Buser A, et al. Reziertes Sehvermögen führt zu erhöhtem Unfallrisiko im Strassenverkehr. Ophthalmologe 1998;95:44–50. [DOI] [PubMed] [Google Scholar]
- 34.Van Rijn LJ, Wilhelm H, Emesz M, et al. Relation between perceived driving disability and scores of vision screening tests. Br J Ophthalmol 2002;86:1262–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferris FL, Kassoff A, Bresnick GH, et al. New visual acuity charts for clinical research. Am J Ophthalmol 1982;94:91–6. [PubMed] [Google Scholar]
- 36.Arditi A, Cagenello R. On the statistical reliability of letter-chart visual acuity measurements. Invest Ophthalmol Vis Sci 1993;34:120–9. [PubMed] [Google Scholar]
- 37.The Age-Related Eye Disease Study Research Group. The Age-Related Eye Disease Study (AREDS). design implications AREDS report no 1. Control Clin Trials 1999;20:573–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vis Sci 1988;2:187–99. [Google Scholar]
- 39.Rubin GS. Reliability and sensitivity of clinical contrast sensitivity tests. Clin Vis Sci 1988;2:169–77. [Google Scholar]
- 40.Elliott DB, Sanderson K, Conkey A. The reliability of the Pelli-Robson contrast sensitivity chart. Ophthalmic Physiol Opt 1990;10:21–4. [PubMed] [Google Scholar]
- 41.Owsley C, Stalvey BT, Wells J, et al. Visual risk factors for crash involvement in older drivers with cataract. Arch Ophthalmol 2001;119:881–7. [DOI] [PubMed] [Google Scholar]
- 42.Chylack LT Jr, Jakubicz G, Rosner B, et al. Contrast sensitivity and visual acuity in patients with early cataracts. J Cataract Refract Surg 1993;19:399–404. [DOI] [PubMed] [Google Scholar]
- 43.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- 44.Bailey IL, Bullimore MA, Raasch TW, et al. Clinical grading and the effects of scaling. Invest Ophthalmol Vis Sci 1991;32:422–32. [PubMed] [Google Scholar]
- 45.Elliott DB, Sheridan M. The use of accurate visual acuity measurements in clinical anti-cataract formulation trials. Ophthalmic Physiol Opt 1988;8:397–401. [DOI] [PubMed] [Google Scholar]
- 46.Office For Official Publications of the European Communities. Council Directive 91/439/EEC of 29 July 1991 on driving licences. Official Journal of the European Communities. L 237, Vol 34, 24 August 1991. L-2985 ed. Luxembourg: Office For Official Publications of the European Communities,.
- 47.Van Rijn LJ, Völker-Dieben HJ. Assessment of vision impairment in relation to driving safety. A literature study. Amsterdam,:1999.


