Abstract
Aim: To assess the intraocular pressure (IOP) variability in patients with primary open angle glaucoma (POAG) under clinical treatment who reached an established target pressure based on isolated office readings.
Methods: Retrospective analysis of 65 eyes from 65 POAG patients under clinical therapy who submitted to modified diurnal tension curve (mDTC) (measurements at every 3 hours between 8 am and 5 pm) followed by a water drinking test (WDT). All subjects had established target IOP ⩽15 mm Hg at 11 am or 2 pm. IOP variability during mDTC or WDT was evaluated.
Results: mDTC revealed IOP measurements ⩾17 mm Hg in 16 of 65 eyes (24.6%). Nine eyes (13.8%) presented values ⩾18 mm Hg. The highest IOP detected by mDTC was 20 mm Hg in one patient (1.5%). WDT demonstrated IOP values ⩾17 mm Hg in 32 of 65 eyes (49.2%). 22 eyes (33.8%) presented values ⩾18 mm Hg after water ingestion. Moreover, IOP levels ⩾20 mm Hg were observed in 14 eyes (21.5%).
Conclusion: A great percentage of POAG patients undergoing clinical treatment and with IOP control based on single office measurement present significantly higher IOP measurements when performing mDTC and, especially, the WDT.
Keywords: glaucoma, intraocular pressure
Elevated intraocular pressure (IOP) is considered the main risk factor for the development of glaucomatous damage. Glaucoma treatment is based mainly on IOP reduction to a level at which no additional damage is expected to occur. This level, the so called target IOP, is established on an individual basis and is usually assessed by single office measurements during working hours.
The benefits of IOP lowering have already been demonstrated by previous studies.1,2 However, a significant group of patients still develop glaucomatous progression despite IOP values considered within adequate limits.3–6 This could be explained by IOP fluctuation during the day or be the result of pressure peaks not detected during office examinations.7,8,9,10
IOP fluctuation is considered a risk factor for the progression of glaucoma.7,8 Drance9 demonstrated that almost one third of patients with single IOP measurements at office hours had pressure peaks only detected during a 24 hour pressure curve. Thus, monitoring the IOP at times during 24 hours of the day could be considered the best way to assess the IOP profile of glaucomatous patients.
In spite of its importance, a 24 hour diurnal tension curve (DTC) is not always feasible in the routine practice. Alternatively, a modified diurnal tension curve (mDTC) has become a common practice and consists of four to five IOP measurements during office hours (from 8 am to 6 pm). However, this test may miss as much as 70% of IOP peaks as a result of IOP variability and also because up to 70% of the highest IOP levels occur at 6 am in supine position.11
Another possible way to assess the IOP is the water drinking test (WDT). Besides being a practical way to estimate the pressure peaks through the 24 hours of the day,12–16 the response to this test was also considered a risk factor for the development of glaucomatous visual field progression in open angle glaucoma.15,16
In this study, we assess the IOP variability using the mDTC and the WDT in patients with primary open angle glaucoma (POAG) undergoing clinical treatment who were considered to be well controlled with IOP equal to or under an established target pressure based on isolated office readings.
METHODS
In this retrospective study, we reviewed the charts of 65 POAG patients who submitted to a modified diurnal tension curve (measurements every 3 hours from 8 am to 5 pm) followed by the WDT from the private office of one of the authors (RSJ).
WDT consisted of basal IOP reading followed by ingestion of 1 litre of tap water. IOP was measured afterwards three times at 15 minute intervals.
All subjects had an established target IOP level of 15 mm Hg, based on glaucomatous damage level. One eye of each patient was randomly chosen for analysis. All eyes had to present IOP equal to or under 15 mm Hg at a single office reading at 11 am or 2 pm. IOP peaks were evaluated with mDTC and WDT.
RESULTS
In all, 65 eyes of 65 patients were included in this study; 29 (44.6%) patients were male. The mean age of all participants was 65.26 (SD 11.15, range 41–87) years.
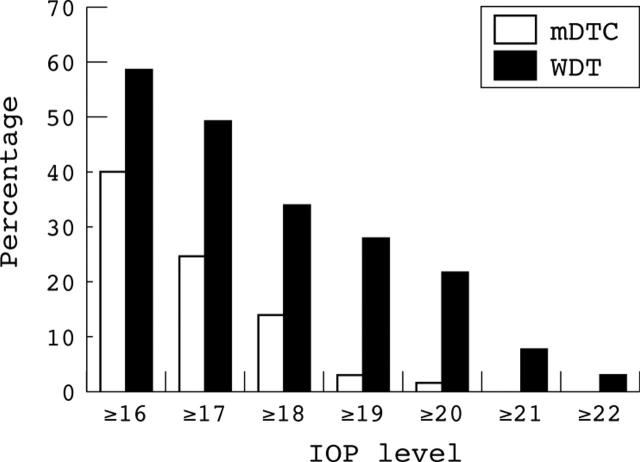
Table 1 and figure 1 summarise IOP peaks detected by mDTC and WDT and their frequencies. mDTC revealed IOP measurements ⩾17 mm Hg in 16 of 65 eyes (24.6%). Nine eyes (13.8%) presented values ⩾18 mm Hg. The highest IOP detected by mDTC was 20 mm Hg in one patient (1.5%).
Table 1.
Frequency of IOP peaks detected by mDTC and WDT
| Maximum IOP detected (mm Hg) | Verified by mDTC | Verified by WDT | ||
| No of patients | % | No of patients | % | |
| 9 | 0 | 0.0 | 1 | 1.5 |
| 10 | 1 | 1.5 | 0 | 0.0 |
| 11 | 2 | 3.1 | 2 | 3.1 |
| 12 | 2 | 3.1 | 4 | 6.2 |
| 13 | 6 | 9.2 | 5 | 7.7 |
| 14 | 8 | 12.3 | 8 | 12.3 |
| 15 | 20 | 30.8 | 7 | 10.8 |
| 16 | 10 | 15.4 | 6 | 9.2 |
| 17 | 7 | 10.8 | 10 | 15.4 |
| 18 | 7 | 10.8 | 4 | 6.2 |
| 19 | 1 | 1.5 | 4 | 6.2 |
| 20 | 1 | 1.5 | 9 | 13.8 |
| 21 | 0 | 0.0 | 3 | 4.6 |
| 22 | 0 | 0.0 | 0 | 0.0 |
| 23 | 0 | 0.0 | 0 | 0.0 |
| 24 | 0 | 0.0 | 2 | 3.1 |
Figure 1.
Frequency of IOP peaks detected by modified diurnal tension curve (mDTC) and water drinking test (WDT) (cumulative frequencies).
WDT demonstrated IOP values ⩾17 mm Hg in 32 of 65 eyes (49.2%). Twenty two eyes (33.8%) presented values ⩾18 mm Hg after water ingestion. Moreover, IOP levels of ⩾20 mm Hg were observed in 14 eyes (21.5%).
DISCUSSION
Despite IOP reduction obtained with glaucoma treatment, even when pressure levels are apparently well controlled, some patients continue to develop glaucomatous progression.3–6 One possible explanation could be the occurrence of IOP peaks not detected during routine examination, as demonstrated by Drance,9 who found that almost one third of patients with single IOP measurements taken at office hours had pressure peaks only detected by a 24 hour tension curve. A study from Zeimer et al11 showed that 29% of patients with progressive visual field damage presented IOP peaks in comparison to 5% of patients with stable visual fields. Also, the occurrence of IOP peaks was related to visual field loss progression in comparison with patients with stable visual fields in a study from Martinez-Belló et al,17 which also did not demonstrate any significant difference between mean IOP levels of patients who developed progression in comparison to stable ones. These studies support the importance of detecting IOP peaks in glaucoma treatment.
A 24 hour daily tension curve would be a candidate for such task. However, this is a time consuming test associated with structural difficulties and costs as major drawbacks. Thus, other practical methods to detect pressure peaks and to assess fluctuation are needed.
The water drinking test was first described in the 1960s as a diagnostic test for glaucoma. After water ingestion, a 6 mm Hg or 8 mm Hg rise in IOP was considered a positive test for the diagnosis of glaucoma.14 However, this test presented unacceptable false positive and false negative results.18
On the other hand, the WDT presents a good correlation between IOP peaks after water overload and IOP peaks detected during a daily tension curve.14 Also, the importance of this test was demonstrated by Armaly et al.16 In a prospective study of 5000 patients with open angle glaucoma, these authors studied 26 potential risk factors for the development of glaucomatous visual field lesion. From these, only five were considered significant: outflow facility, age, IOP, cup/disc ratio and change in IOP after water ingestion. Moreover, Yoshikawa et al18 demonstrated that WDT was the main predictive test for glaucomatous progression in a group of patients with normal tension glaucoma.
It has been hypothesised that the WDT could be used as an indirect tool to measure outflow facility. Indeed, Susanna and Medeiros,19 using this test, were able to demonstrate reduced IOP fluctuation in patients controlled with filtering surgery in comparison with those controlled with topical medication.
All these data have changed the concept of the WDT, which is not used as a diagnostic test anymore, but as a useful tool to assess IOP peaks and IOP fluctuation.
In this study the IOP profile of POAG patients undergoing clinical treatment and apparently well controlled, as verified by single office measurements was assessed. This was done with a modified daily tension curve, widely used in general clinical practice, followed by the WDT. Both tests were capable of demonstrating the existence of IOP peaks. However, the frequency of detected peaks was higher when assessed by the WDT, which also demonstrated higher levels of IOP and higher fluctuation.
One explanation for this difference could be the fact that the modified daily tension curve does not measure the IOP during the times when it is expected to be higher (for example, 6 am) which, in turn, could be a result of the supine position of the patient at the time of measurement. Indeed, Hirooka and Shiraga20 found a significant difference between IOP levels measured in the sitting and supine positions, the greater differences being in eyes with worse visual field damage. It is worth noting that their results suggested that more glaucomatous damage could happen during sleep in the supine position.
On the other hand, assuming that the WDT has a good correlation with the IOP peaks detected during a 24 hour daily tension curve, it is reasonable to accept that these high IOP levels are actually occurring through the day, presenting a considerable risk for the progression of the disease and which were revealed by this promising test. Moreover, this is an easy test to perform, involving the natural and physiological act of drinking water.
In summary, our data demonstrate the importance of a careful assessment of IOP profile in glaucomatous patients, even when clinical treatment seems to be adequate. The modified daily tension curve can demonstrate IOP peaks, although with lower frequency and lower amplitude in comparison with the water drinking test. This study also emphasises the value that the water drinking test may have as a complementary test in clinical practice.
Abbreviations
mDTC, modified diurnal tension curve
POAG, primary open angle glaucoma
WDT, water drinking test
REFERENCES
- 1.The AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS). 7. The relationship between control of intraocular pressure and visual field deterioration. Am J Ophthalmol 2000;130:429–40. [DOI] [PubMed] [Google Scholar]
- 2.Leske MC, Heijl A, Hussein M, et al. Factors for glaucoma progression and the effect of treatment: the early manifest glaucoma trial. Arch Ophthalmol 2003;121:48–56. [DOI] [PubMed] [Google Scholar]
- 3.Kidd MN, O’Conner M. Progression of field loss after trabeculectomy: a five-year follow-up. Br J Ophthalmol 1985;69:827–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schulzer M, Mikelberg FS, Drance SM. Some observations on the relation between intraocular pressure and the progression of glaucomatous visual field loss. Br J Ophthalmol 1987;71:486–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Brien C, Schwartz B, Takamoto T, et al. Intraocular pressure and the rate of visual field loss in chronic open-angle glaucoma. Am J Ophthalmol 1991;111:491–500. [DOI] [PubMed] [Google Scholar]
- 6.Chauhan BC, Drance SM. The relationship between intraocular pressure and visual field progression in glaucoma. Graefes Arch Clin Exp Ophthalmol 1992;230:521–6. [DOI] [PubMed] [Google Scholar]
- 7.Zeimer RC, Wilensky JT, Gieser DK, et al. Association between intraocular pressure peaks and progression of visual field loss. Ophthalmology 1991;98:64–9. [DOI] [PubMed] [Google Scholar]
- 8.Asrani S, Zeimer R, Wilensky J, et al. Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma 2000;9:134–42. [DOI] [PubMed] [Google Scholar]
- 9.Drance SM. Diurnal variation of intraocular pressure in treated glaucoma. Arch Ophthalmol 1963;70:302–11. [DOI] [PubMed] [Google Scholar]
- 10.Katavisto M. The diurnal variations of ocular tension in glaucoma. Acta Ophthalmol 1994;78 (suppl) :1–131. [PubMed] [Google Scholar]
- 11.Zeimer R. Circadian variations in intraocular pressure. In: Ritch R, Shields MB, Krupin T, eds. The glaucomas. St Louis: CV Mosby, 1996.
- 12.Miller D. The relationship between diurnal tension variation and the water-drinking test. Am J Ophthalmol 1964;58:243–7. [DOI] [PubMed] [Google Scholar]
- 13.Susanna R, Medeiros FA, Vessani RM. Correlation between intraocular pressure peaks in the diurnal tension curve and in the water-drinking test [ARVO Abstract]. Invest Ophthalmol Vis Sci. 2001;42: S558 (abstract no 2995),.
- 14.Medeiros FA, Leite CA, Susanna R Jr. Correlação entre os picos pressóricos da curva tensional diária e do teste de sobrecarga hídrica. Estudo em pacientes com glaucoma primário de ângulo aberto em uso de tilmolol e dorzolamida. Rev Bras Oftal 2001;60:418–23. [Google Scholar]
- 15.Yoshikawa K, Inohue T, Inohue Y. Normal tension glaucoma: the value of predictive tests. Acta Ophthalmol 1993;71:463–70. [DOI] [PubMed] [Google Scholar]
- 16.Armaly MF, Krueger DE, Maunder L, et al. Biostatistical analysis of the Collaborative Glaucoma Study. I. Summary report of the risk factors for glaucomatous visual-field defects. Arch Ophthalmol 1980;98:2163–71. [DOI] [PubMed] [Google Scholar]
- 17.Martinez-Bello C, Chauhan BC, Nicolela MT, et al. Intraocular pressure and progression of glaucomatous visual field loss. Am J Ophthalmol 2000;129:302–8. [DOI] [PubMed] [Google Scholar]
- 18.Roth JA. Inadequate diagnostic value of the water drinking test. Br J Ophthalmol 1974;58:55–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Medeiros FA, Pinheiro A, Susanna R Jr, et al. Intraocular pressure fluctuations in medical versus surgically treated glaucomatous patients. J Ocul Pharmacol Ther 2002;18:489–98. [DOI] [PubMed] [Google Scholar]
- 20.Hirooka K, Shiraga F. Relationship between postural change of the intraocular pressure and visual field loss in primary open angle glaucoma. J Glaucoma 2003;12:379–82. [DOI] [PubMed] [Google Scholar]