Abstract
Background: People with retinitis pigmentosa (RP) experience functional and psychological challenges as they adjust to progressive loss of visual function. The authors aimed to understand better the process of adjusting to RP in light of the emotional suffering associated with this process.
Methods: Adults with RP were recruited from the Foundation Fighting Blindness and the Wilmer Eye Institute in Baltimore. Focus groups and semistructured interviews addressed the process of adjusting to RP and were audiotaped and transcribed. The transcripts were analysed qualitatively in order to generate a model of adjustment.
Results: A total of 43 individuals participated. It was found that, on diagnosis, people with RP seek to understand its meaning in their lives. Mastering the progressive functional implications associated with RP is contingent upon shifting personal identity from a sighted to a visually impaired person. In this sample, six participants self identified as sighted, 10 self identified as in transition, and 27 self identified as visually impaired. This adjustment process can be understood in terms of a five stage model of behaviour change.
Conclusions: The proposed model presents one way to understand the process of adjusting to RP and could assist ophthalmologists in meeting their moral obligation to lessen patients’ suffering, which arises in the course of their adjustment to progressive loss of visual function.
Keywords: retinitis pigmentosa, progressive loss of vision, psychological challenges, adjustment model, qualitative methods
Retinitis pigmentosa (RP) is a relatively common type of progressive diffuse retinal degeneration. There is no prevention, cure, or means to restore retinal function.1,2 Adjusting to RP inevitably entails a certain degree of suffering. Suffering can be defined as a state of distress that occurs when a person’s integrity or life plan is threatened, disrupted, or burdened; it lasts until integrity is restored, either by eliminating the threat or adjusting to it. It is not the physical impairments themselves, but the impact of the physical state on the person as a whole that causes suffering. This has been referred to as “existential suffering.”3–6 It is arguably the case that physicians are morally obligated to lessen suffering in their patients.7 In the case of RP, where there is little that physicians can do to alter the course of retinal degeneration, one means by which to lessen suffering is to participate in patients’ process of adjusting to it.
When people with RP confront challenges related to education, employment, mobility, and socialisation,8 psychosocial development,9 use of assistive technology,10,11 and mental health,12 suffering may manifest as denial, anger, fear, or depression.13–19 Despite what is known about these challenges, the process of adjusting to vision loss is only touched upon in the clinical ophthalmology literature.20,21 It has been reported that the presence of role models,22,23 social supports,24,25 and a positive doctor-patient relationship may influence adjustment.26 By developing an appreciation of their patients’ adjustment process, ophthalmologists would be doing more than fostering a positive doctor-patient relationship. They would, it has been argued,5 be meeting a moral obligation to understand the lived experiences of their patients as a means by which to lessen patient suffering.
In light of the limitations in the quantitative literature to date, we set out to explore the process of adjusting to the loss of visual function associated with RP through a qualitative approach. In this paper we report our findings and develop a model for ophthalmologists to consider in their effort to understand and lessen their patients’ suffering. Seven practical steps are suggested as means by which to incorporate this model into clinical practice.
METHODS
While quantitative tools are available to “measure” the extent to which someone has adjusted to a given circumstance, a qualitative approach better captures the essence of the adjustment process and factors that influence its course that may not be revealed by available quantitative tools.27–30 For this reason, we chose to use qualitative methodology.
Adults with RP were recruited from the Baltimore chapter of the Foundation Fighting Blindness (FFB) and The Wilmer Eye Institute at Johns Hopkins Hospital. FFB registrants were stratified into three predetermined age categories before recruitment since these data were available at this time, whereas Wilmer patients were stratified according to age following a preliminary screening questionnaire to determine eligibility (table 1). This theoretical sampling technique28 enabled us to collect data that reflected the adjustment process at various life stages. By telephone or mail, all eligible individuals were invited to participate. Consent was obtained by a paper or by voice recorded consent. This study was approved by the joint committee of clinical investigation at Johns Hopkins Medical Institute.
Table 1.
Recruitment stratification (theoretical sampling frame)
| Group 1 | Group 2 | Group 3 | |
| Age at diagnosis | <18 years | 18–35 years | >35 years |
| Age at study participation | <35 years | 35–50 years | >50 years |
Data were collected through semistructured interviews and focus groups. Three focus groups were conducted by trained moderators, lasted 2 hours, and were transcribed by court stenographers. Telephone interviews were conducted by trained interviewers, were approximately 45 minutes in duration, and were audiotaped and transcribed.
Transcripts were analysed qualitatively (see appendix). The end product of our analysis is a process oriented model that depicts the relationships among the codes and the core category. Demographic data were analysed descriptively.
Sample
In all, 43/88 individuals agreed to participate (response rate 49%). Table 2 presents demographic data on participants. Among non-participants for whom demographic data were available (32/45; FFB registrants only), the mean age at the time of recruitment was 51 years and mean age of diagnosis was 26 years; 67% were male and 25% had a known family history of RP.
Table 2.
Demographic characteristics of participants
| Variable | Age group 1 | Age group 2 | Age group 3 | Total |
| (x/8) | (x/19) | (x/16) | (x/43) | |
| Sex | ||||
| Male | 5 (62%) | 11 (58%) | 8 (50%) | 24 (56%) |
| Female | 3 (38%) | 8 (42%) | 8 (50%) | 19 (44%) |
| Age now | ||||
| Mean (range) | 33.5 (21,44) | 49 (39,77) | 61 (49,79) | 48 (21,79) |
| Age at diagnosis | ||||
| Mean (range) | 15 (4,35) | 18 (5,30) | 41 (27,52) | 25 (4,52) |
| Race | ||||
| White | 8 (100%) | 16 (84%) | 16 (100%) | 40 (93%) |
| African-American | 0 | 3 (16%) | 0 | 3 (7%) |
| Religion | ||||
| Catholic | 3 (38%) | 5 (26%) | 5 (31%) | 13 (30%) |
| Protestant | 4 (50%) | 9 (47%) | 7 (44%) | 20 (46%) |
| Jewish | 1 (12%) | 0 (0%) | 4 (25%) | 5 (12%) |
| Other/none | 0 (0%) | 5 (26%) | 0 (0%) | 5 (12%) |
| Relationship status | ||||
| Married | 6 (75%) | 13 (68%) | 14 (88%) | 33 (77%) |
| Single | 2 (25%) | 3 (16%) | 0 (0%) | 5 (12%) |
| Partner | 0 (0%) | 2 (1%) | 0 (0%) | 2 (0.5%) |
| Divorced/separated | 0 (0%) | 0 (0%) | 1 (6%) | 1 (0.2%) |
| Widowed | 0 (0%) | 1 (1%) | 1 (6%) | 2 (0.5%) |
| Grade level | ||||
| High school | 0 (0%) | 3 (16%) | 5 (31%) | 8 (19%) |
| Some college | 3 (38%) | 9 (47%) | 3 (19%) | 15 (35%) |
| 4 years at college | 3 (38%) | 4 (21%) | 3 (19%) | 10 (23%) |
| Post grad school | 2 (25%) | 3 (16%) | 5 (31%) | 10 (23%) |
| Income | ||||
| <$20 000 | 0 (0%) | 4 (21%) | 1 (0.6%) | 5 (12%) |
| $20 000–$34 999 | 1 (12%) | 3 (16%) | 5 (31%) | 9 (21%) |
| $35 000–$49 999 | 1 (12%) | 4 (21%) | 1 (0.6%) | 6 (14%) |
| $50 000–$74 999 | 1 (12%) | 5 (26%) | 3 (2%) | 9 (21%) |
| >$75 000 | 5 (62%) | 3 (16%) | 6 (38%) | 14 (32%) |
| Employment | ||||
| Full time | 5 (62%) | 8 (42%) | 4 (25%) | 17 (40%) |
| Part time | 1 (12%) | 2 (11%) | 3 (19%) | 6 (14%) |
| Retired | 0 (0%) | 0 (0%) | 7 (44%) | 7 (16%) |
| Unemployed | 2 (25%) | 9 (47%) | 2 (12%) | 13 (305%) |
| Affiliation | ||||
| FFB | 7 (88%) | 15 (79%) | 13 (81%) | 35 (81%) |
| Support group | 3 (38%) | 8 (42%) | 9 (56%) | 20 (46%) |
| Family history of RP | ||||
| Present | 3 (38%) | 3 (16%) | 1 (6%) | 7 (16%) |
| Absent | 4 (50%) | 10 (53%) | 13 (81%) | 27 (63%) |
| Unknown | 1 (12%) | 6 (32%) | 2 (12%) | 9 (21%) |
| Self identified as | ||||
| Sighted | 2 (25%) | 2 (10%) | 2 (12%) | 6 (14%) |
| In transition | 3 (38%) | 2 (10%) | 5 (31%) | 10 (23%) |
| Visually impaired | 3 (38%) | 15 (80%) | 9 (56%) | 27 (63%) |
RESULTS
The qualitative data presented below illustrate particularly salient themes reflected by the majority of participants. Each theme is placed in the context of the adjustment model, illustrated diagrammatically in figure 1. Participants’ sex, age at participation, and age at diagnosis are indicated following their remarks.
Figure 1.
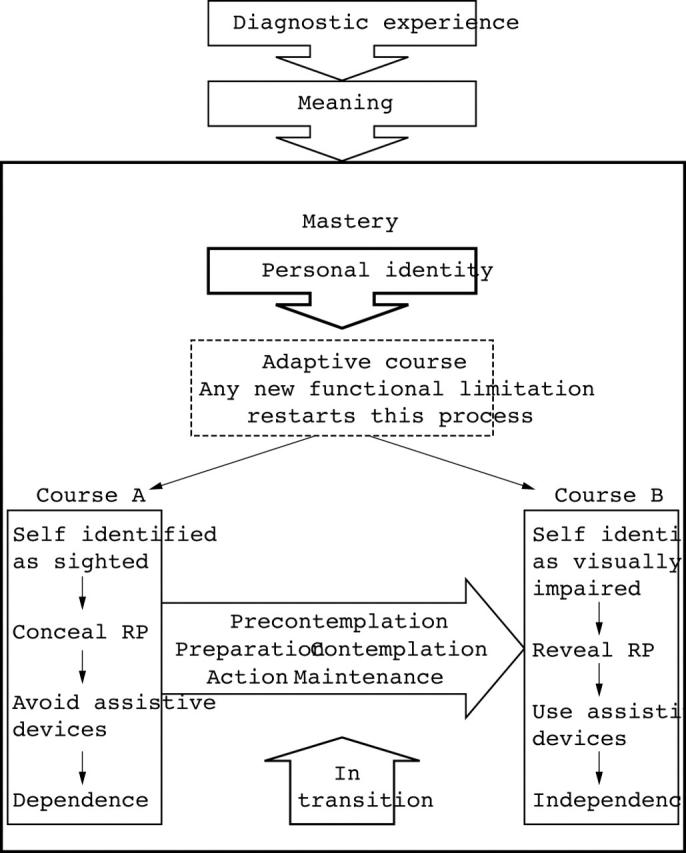
Adjustment model.
Diagnostic experience and reactions
Participants described a range of reactions at the time of their diagnosis that were influenced by the way in which physicians communicated the diagnosis to them. When physicians used what the majority of participants described as “blunt” language, participants described feeling devastated:
“He said, ‘by the time you’re 50 you’re not going to be able to drive. You’re not going to be able to read by the time you’re 60 or see light by the time you’re 70.’ I was completely devastated. I was 30 years old… the end of my life felt like it occurred that day.” (F55/30)
When physicians used what some participants described as “vague” language, participants described feeling anxious:
“He told me I had RP but didn’t tell me I would likely go blind. I didn’t know what it was…I went through a lot of anxiety attacks because I had no knowledge of what was actually going to happen….” (M62/40)
In contrast, when physicians used what some participants described as “mild” language, many participants felt hopeful:
“He said, ‘it’s a progressive disease. It’s a long slow process…you’re not going to have any immediate problems, it could happen in five years or in 50 years’…so I chose to hope it would happen in 50 and move on…” (M56/15)
Meaning
In order to make sense of their diagnosis, all participants searched to understand why it happened. Many participants considered both genetic and non-genetic causes of RP:
“either I got it from a hard blow to the head or I inherited it…since nobody going back has it they narrowed it down to when I fell down the stairs.” (F35/22)
And some participants used spirituality to reflect on this question:
“You wonder, God, why is it me? Well, maybe I’m an inspiration to someone, maybe I’m affecting other people’s lives positively…maybe that’s the reason.” (M42/27)
Personal identity
For most participants, resolving personal identity as a sighted versus a visually impaired person posed an early and pivotal challenge. We deemed personal identity to be the core variable of our analysis since participants’ described their adjustment as contingent upon it:
“Now I’m just sort of lost in between…one of the hardest things for me has been not feeling like a sighted person and not feeling like a blind person. I’ve gotten to know some blind people and seen how amazingly well they’ve adapted and then I see my sighted friends, and then I see myself, and I am neither. I feel like I am going to be inferior until I am either or.” (M21/6)
“What was particularly vexing for me, since it is so slow, you really have a hard time putting your finger on when it is you need to change the way you do this or that, how you present yourself to other people…” (M62/37)
Course of action
Two courses of action emerged as participants were in the process of resolving their personal identity.
Figure 1, course A (self identified as sighted)
At various ages, six participants identified as sighted and resisted using assistive devices and making lifestyle changes (table 2). They described making an effort to conceal any evidence of visual impairment.
“I’m not at the point where I’m comfortable with the idea of people looking at me differently. If I wear my contacts I look totally normal and people just don’t know.” (F29/16)
“I do my own private little shopping…I hate the stores…I order whatever over the phone, flip out my credit card, and UPS delivers it to my door.” (F54/20)
Figure 1, Course B (self identified as visually impaired)
Irrespective of their age, 27 participants identified as visually impaired and described assistive devices and certain lifestyle changes as adaptive (table 2) because they:
explain RP to others: “…the stick lets everybody know that when I walk into a pole or bump into them, there is a reason for it.” (M57/21)
promote independence: “To me the cane is gonna let me walk without tripping, and get places that I wouldn’t be able to go.” (M24/18)
promote competence: “I worked nights and weekends to learn these computer programs because my goal was to be more proficient than anybody…and then my boss put me in charge of computerising the entire department.” (M42/27)
promote safety: “[my guide dog] takes me downtown to work…I feel more at ease because I know she won’t let anything like a car come at me…” (M62/40)
Behaviour change
Course A appears to act as a default path until individuals make certain behavioural and/or lifestyle changes and approach course B. Our data illustrate various stages between course A and course B. Ten participants, between the ages of 21 and 59 identified themselves as in transition between sighted and visually impaired (table 2). They could acknowledge some of the benefits of assistive devices but were not ready to use them:
“I would like that visible symbol for people to know and understand…but I wish there was something other than a cane.” (F49/38)
Five of these ten participants expressed tentative readiness to make changes:
“I look totally normal with my glasses on, but then I put those clips on, like my parents do…I’m not even 30…I’m forcing myself to wear them around my comfort zone but I haven’t gone out with them yet.” (F29/16)
Three participants who were currently further along in their transition process described their adaptive steps. For example,
“[the mobility trainer] said…before you go out the door, you pick up your purse and you pick up your cane …then my husband came home and said let’s go out for dinner, grab your cane…okay, here we go, so I get outside and I open my cane…” (F50/18)
Others reflected on new ways of meeting their same goals:
“I’m not able to play basketball or golf anymore…so I’ve tried independent sports where I can still challenge and exercise myself like roller-blading and wind-surfing.” (M34/6)
Some participants recalled vacillating between ambiguous identities and related behaviours. For example,
“There was a time when I used to drive a car and use a cane. I would keep the cane concealed underneath the dash and use the cane at night.” (F55/30)
As well, many participants reflected on the continuous processing required as they encountered new functional limitations over time, irrespective of age:
“At any age…you’re constantly in flux. You get to levels of acceptance and levels of accomplishment and then it gets a little worse so you drop down a step and then you need another apparatus…every step is a process to where you’re going…you have to be mentally strong and self confident because you get knocked down and have tough days…but you have to keep moving forward.” (M42/27)
Ultimately, once participants viewed behavioural and lifestyle changes as personal benefit rather than as social risk, adaptive changes became integrated into their lives:
“I discovered that [the cane] was positively liberating. It means I don’t have to have someone with me and I can go out anytime anywhere by myself.” (M62/37)
Many participants referred to their public use of assistive devices as “outing” themselves:
“Once you’re ‘out,’ the cane is the only way you know.” (M49/16)
Self esteem
All participants described self esteem as critical to moving through this continuum. This was particularly salient among younger participants and participants in transition:
“Sure I’ve had my inferiority problems…I’ve been ashamed that I couldn’t be the one to drive and macho stuff like that…that was a low point for me.” (M24/18)
“I try to feel good about myself in other ways. I keep myself in shape, do my hair and make-up, so if people look at me and see me with dark glasses and a cane, I can still look and feel attractive…” (F29/16)
DISCUSSION
Ages of participants and non-participants at the time of participation and diagnosis were similar (48 years and 51 years, respectively, 25 years and 26 years respectively). While there were more male than female non-participants, there were also more male participants. The X linked pattern of inheritance that can be associated with RP may account for a greater proportion of males in this population in general. Participation did not appear to be a function of age or sex therefore these variables are unlikely to have affected the nature of the model developed. Family history was slightly more common among non-participants. Perhaps those with a family history perceived adjustment as a family norm rather than as a process that required significant exploration. We could speculate, therefore, that the model presented better applies to individuals who do not have a known family history of RP.
Adjustment model
Our data suggest that the process of adjusting to RP is a dynamic one composed of a series of inter-related steps. As stated in the appendix, we found our data to be consistent with certain existing concepts in the adjustment literature.31 The search for meaning involves understanding why a disability has occurred. Mastery centres around gaining control over the implications in order to manage them. Self esteem reflects the effort to regain a positive view of oneself in a new life situation.
Applying in-depth qualitative analysis techniques to participants’ personal stories, we were able to construct a model that reflects true lived experiences rather than objective measurements that emerge from highly structured quantitative approaches. We found that adjustment proceeds as follows (fig 1). The diagnostic experience combined with individuals’ reactions to it can lead to emotional suffering. In response, individuals search to understand the meaning and cause of their RP; they attribute causation to inheritance, childhood accidents, and spiritual intervention.
Functional limitations ensue and challenge a person’s integrity. Mastering these limitations is motivated, in part, by that person’s interest in reducing his/her own suffering and appears to be contingent upon resolving personal identity as a sighted or visually impaired person. This may involve changing deeply engrained behaviours, a process that has been described as a series of five stages.32 The stage of precontemplation characterised those who did not need to change behaviour, had not acknowledged their need to change, or were not ready to change. During contemplation, participants reflected the profound ambivalence between sighted and visually impaired identities. In this phase, the disadvantages of changing outweighed the advantages. As the balance began to tip, participants reflected plans to give up driving or to take mobility training as examples of the preparation stage and continued to move through the action phase as they began to use assistive devices in public or find novel solutions to their limitations. The action stage was characterised by participants “outing” themselves. Once they were “out,” the benefits of independence and competence outweighed previously perceived social risks. This shift enabled these adjustments to be maintained.
Ultimately, adjustment was achieved when individuals self identified as visually impaired, revealed their RP, used assistive devices, and made lifestyle changes in order to regain self esteem and independence. Since the behavioural, lifestyle, and psychological changes that constitute adjustment appear to be contingent upon participants’ identity as sighted or visually impaired, personal identity was deemed the core category of this model.
It is noteworthy that responses among participants in various age categories were relatively consistent. Our sample reflected preliminary (sighted identity described by six participants), transitional (ambiguous identity described by 10 participants), and final (visually impaired described by 27 participants) stages of this process. Since each age group was represented in each of these identity categories, we suggest that, although the task at hand may vary with age or stage of life, the core assumptions of the model can be used to navigate adjustment at any age.
Using quantitative methodology, Dodds et al21 developed an adjustment model that specified internal self worth and self as agent as key variables and suggested that these variables be integrated into a cognitively oriented therapeutic approach with patients. Zaborowski33 endorsed this approach by suggesting that adjusting to blindness requires an individual to make a cognitive shift which acknowledges that being blind can be compatible with remaining functionally independent. This suggests that a healthcare provider could use our model as a tool by which to help their patients approach this necessary cognitive shift in personal identity.
Limitations
This model reflects only one interpretation of these data. Specific limitations are highlighed in table 3.
Table 3.
Study limitations
| (1) Biased sample |
| (a) the youngest age group is poorly represented and may be particularly vulnerable to emotional suffering; |
| (b) the majority of this sample self identified as visually impaired and represents a white, well educated, middle upper class population and may not represent the experiences of those in other visual function or demographic groups. |
| (2) An inherent limitation of focus groups is the tendency for more vocal participants to dominate the discussion, making their views seem like the most important ones. |
| (3) While participants were asked to comment on their prediagnostic experiences, undoubtedly an influence on their adjustment process, this model begins with the diagnostic experience itself as the formal starting point of the adjustment process described. |
| (4) Given the uniquely predictable course of progression of RP,34 the generalisability of these findings to other populations of patients with progressive vision loss is limited. |
Contribution to the literature
Our data support an integration of adjustment and behaviour change theories by illustrating how adjustment implicates behaviour change through the construct of personal identity. Our data add to the suffering literature by providing a concrete clinical example of the distinction between “symptom related” suffering and “existential” suffering.6
Finally, we believe that this model may be of particular importance since it is patient driven and, hopefully, of clinical value to physicians. As physicians endeavour to lessen suffering, addressing personal identity with patients is paramount. Physicians can better fulfil their moral obligation to lessen suffering by contributing to identity resolution and adjustment. Practical steps by which to do so are outlined in table 4. Rather than reacting to suffering after it presents, this model may help ophthalmologists be proactive in predicting it, minimising it, and/or seeking appropriate consultation for patients. By eliciting and attending to patients’ subjective experiences associated with a shift in personal identity, ophthalmologists can fine tune their care in order to lessen patients’ suffering that arises in the course of their adjustment to progressive loss of vision.
Table 4.
Seven practical steps for ophthalmologists to integrate into practice
| (1) Understand the meaning patients ascribe to their diagnosis |
| (2) Recognise and acknowledge the manifestations of an unresolved identity (concealing RP, avoiding adaptive change) |
| (3) Normalise any personal identity conflict patients express by (anonymously) sharing similar conflicts experienced by other patients, for example |
| (4) Help patients weigh the advantages and disadvantages of behaviour and lifestyle changes |
| (5) Tailor their dialogue and recommendations to patients’ functional and psychological readiness for change |
| (6) Acknowledge patients’ progress |
| (7) Provide guidance and supportive resources in anticipation of this suffering in order to facilitate smooth and adaptive transitions. |
Acknowledgments
We thank Stephanie Rice Davis, MSW, for contributing to the original project proposal and facilitating communication with the donors.
We thank Julia Slutsman, PhD, for assisting with the qualitative analysis of these data.
This project was made possible by an anonymous gift.
Abbreviations
FFB, Foundation Fighting Blindness
RP, retinitis pigmentosa
APPENDIX
QUALITATIVE ANALYSIS
Criteria used to identify salient themes within the transcripts included: (1) text that described key elements of the participants’ adjustment processes and (a) recurred in multiple transcripts, (b) recurred in both telephone interview and focus group transcripts, or (c) recurred among participants in different demographic categories (for example, age, sex groups). Salient themes were then assigned codes. Some codes reflected direct responses to interview questions and other codes emerged from the experiences shared by participants over the course of the interview or discussion. The theme upon which adjustment was deemed to be contingent by the majority of participants was considered to be the core category.27,28
A qualitative analysis software package called Nvivo was used to organise the coded data.35 Nvivo enables the analyst to code text as it is reviewed, quantify the frequency of relevant themes across transcripts, and discern relations among salient themes by way of coding trees and conceptual maps.
While telephone interview and focus group data reflected different experiences and emphases on some topics, themes pertinent to the adjustment process and captured by the proposed model were similar. For this reason, these data were combined for the purpose of this paper.
We integrated the concepts generated from our data with related concepts reported in the literature. Specifically, meaning, mastery, self esteem,31 and the five stages of behaviour change32 are constructs derived from the literature that support the data generated. The components of the adaptive courses (course A and course B), the construct of personal identity, and the relation among all of these components of the model emerged from the data themselves.
REFERENCES
- 1.Phelan JK, Bok D. A brief review of retinitis pigmentosa and the identified retinitis pigmentosa genes. Mol Vis 2001;6:16–24. [PubMed] [Google Scholar]
- 2.Pagon RA. Retinitis pigmentosa: major review. Surv Ophthalmol 1988;33:137–77. [DOI] [PubMed] [Google Scholar]
- 3.Cassell EJ. Diagnosing suffering: a perspective. Ann Intern Med 1999;131:531–4. [DOI] [PubMed] [Google Scholar]
- 4.Cassell EJ. The nature of suffering and the goals of medicine. N Engl J Med 1982;306:639–45. [DOI] [PubMed] [Google Scholar]
- 5.Kleinman A. Writing at the margin: discourse between anthropology and medicine. Berkeley, CA: University of California Press, 1997:95–101.
- 6.Gunderman RB. Is suffering the enemy? Hastings Center Report 2002;32:40–4. [PubMed] [Google Scholar]
- 7.Schultz DS, Carnevale FA. Engagement and suffering in responsible caregiving: on overcoming maleficence in health care. Theor Med 1996;17:189–207. [DOI] [PubMed] [Google Scholar]
- 8.Nemshick LA, Vernon McC, Ludman F. The impact of retinitis pigmentosa on young adults: psychological, educational, vocational, and social considerations. J Vis Imp Blindness Sept 1986:859–62.
- 9.Rogow S. The impact of visual impairments on psychosocial development. Handbook of psychosocial characteristics of exceptional children. Plenum series on human exceptionality. NY: Kluwer Academic/Plenum Publishers, 1999:523–39.
- 10.Lueck AH, Dote-Kwan J, Senge JC, et al. Selecting assistive technology for greater independence. Review 2001;33:21–33. [Google Scholar]
- 11.Wainapel SF. Attitudes of visually impaired persons toward cane use. J Vis Imp Blindness 1989;83:446–8. [Google Scholar]
- 12.Reis JB. The psychological experience of retinitis pigmentosa. Dissertation Abstracts International 1996;57:1504. [Google Scholar]
- 13.Wuslin LR, Jacobson AM, Rand LJ. Psychosocial correlates of mild vision loss. Psychosom Med 1991;53:109–17. [DOI] [PubMed] [Google Scholar]
- 14.Koenes SG, Karshmer JF. Depression: a comparison study between blind and sighted adolescents. Issues Ment Health Nurs 2000;21:269–79. [DOI] [PubMed] [Google Scholar]
- 15.Mangione CM, Berry S, Spritzer K, et al. Identifying the content area for the 51-item National Eye Institute function questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol 1998;116:227–33. [DOI] [PubMed] [Google Scholar]
- 16.De Leo D, Hickey PA, Meneghel G, et al. Blindness, fear of sight loss, and suicide. Psychosomatics 1999;40:339–44. [DOI] [PubMed] [Google Scholar]
- 17.Abolfotouh MA, Telmesani A. A study of some psycho-social characteristics of blind and deaf male students in Abha City, Asir region, Saudi Arabia. Public Health 1993;107:261–9. [DOI] [PubMed] [Google Scholar]
- 18.Cox DJ, Kiernan BD, Schroeder DB, et al. Psychosocial sequelae of visual loss in diabetes. Diabetes Educ 1998;24:481–4. [DOI] [PubMed] [Google Scholar]
- 19.Fitzgerald RG, Ebert JN, Chambers M. Reactions to blindness: a four-year follow-up study. Percept Mot Skills 1987;64:363–78. [DOI] [PubMed] [Google Scholar]
- 20.Rakes SM, Reid WH. Psychologic management of loss of vision. Can J Ophthalmol 1982;17:178–80. [PubMed] [Google Scholar]
- 21.Dodds A, Ferguson E, Ng L, et al. The concept of adjustment: a structural model. J Vis Imp Blindness 1994:487–97.
- 22.Allen M. Adjusting to visual impairment. J Ophthal Nurs Tech 1990;9:47–51. [PubMed] [Google Scholar]
- 23.Koestler FA. Visually impaired women and the world of work: theme and variations. J Vis Imp Blindness 1983;77:276–7. [Google Scholar]
- 24.Pfanstiehl MR. Role models for high-achieving visually impaired women. J Vis Imp Blindness 1983;77:259–61. [Google Scholar]
- 25.Duncan E, Prickett HT, Finkelstein D, et al. Usher’s syndrome: what it is, how to cope, and how to help. Springfield, IL: Charles C Thomas, 1988.
- 26.Hopper SV, Fischbach RL. Patient-physician communication when blindness threatens. Patient Educ Couns 1989;14:69–79. [DOI] [PubMed] [Google Scholar]
- 27.Creswell JW. Qualitative Inquiry and research design: choosing among five traditions. Thousand Oaks, CA: Sage Publications, 1998.
- 28.Strauss A, Corbin J. Basics of qualitative research: grounded theory procedures and techniques. 2nd ed. Newbury Park, CA: Sage Publications, 1998.
- 29.Sandelowski M. What ever happened to qualitative description? Res Nurs Health 2000;23:334–40. [DOI] [PubMed] [Google Scholar]
- 30.Thorne S, Reimer Kirkham S, MacDonald-Emes J. Interpretive description: a non-categorical qualitative alternative for developing nursing knowledge. Res Nurs Health 1997;20:169–77. [DOI] [PubMed] [Google Scholar]
- 31.Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am Psychol 1983;38:1161–73. [Google Scholar]
- 32.Prochaska JO, DiClemente CC. Stages and processes of self change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983;51:390–5. [DOI] [PubMed] [Google Scholar]
- 33.Zaborowski B. Adjustment to vision loss and blindness: a process of reframing and retraining. J Rational-Emotive Cognitive Behav Therapy 1997;15:215–21. [Google Scholar]
- 34.Massof RW, Finkelstein D. A two-stage hypothesis for the natural course of retinitis pigmentosa. Adv Biosci 1987;62:29–58. [Google Scholar]
- 35.NVivo—Nud*ist for qualitative research. Australia: Qualitative Solutions and Research Pty Ltd 1999.


