Abstract
Aims: To evaluate the influence of central corneal thickness (CCT) on intraocular pressure (IOP) measurements made with the Goldmann applanation tonometer (GAT), Tono-Pen XL, ocular blood flow tonograph (OBF), and Canon TX-10 non-contact tonometer (NCT).
Methods: CCT was recorded for either eye (randomly selected) of each of 105 untreated patients with ocular hypertension and glaucoma attending the glaucoma research unit at Moorfields Eye Hospital. For each of the selected eyes, IOP was measured with the GAT (two observers), Tono-Pen, OBF, and NCT in a randomised order. The relation of measured IOP and of inter-tonometer differences with CCT and subject age was explored by linear regression analysis.
Results: A significant association between measured IOP and CCT was found with each instrument. The change in measured IOP for a 10 μm increase in CCT was 0.28, 0.31, 0.38, and 0.46 for the GAT, Tono-Pen, OBF, and NCT, respectively (all p⩽0.05). There was a significant association between the NCT/GAT differences and CCT, with a tendency of NCT to overestimate GAT in eyes with thicker corneas. There was a significant association between GAT/Tono-Pen and OBF/Tono-Pen differences and age, with a tendency of GAT and OBF to overestimate the Tono-Pen in eyes of older subjects.
Conclusion: IOP measurement by all four methods is affected by CCT. The NCT is affected by CCT significantly more than the GAT. Subject age has a differential effect on the IOP measurements made by the GAT and OBF compared to the Tono-Pen.
Keywords: tonometry, intraocular pressure, cornea, age, measurement error
Central corneal thickness (CCT) is known to affect the accuracy of intraocular pressure (IOP) measurements by applanation tonometry.1,2 A thicker cornea requires greater force to applanate and, conversely, a thinner cornea is more easily flattened. A thin cornea is a significant risk factor for the development of glaucoma3 and it has yet to be determined whether this is an independent effect or a result of the influence of CCT on IOP measurements.
Most published studies concerning the effect of CCT on measured IOP relate to the Goldmann applanation tonometer (GAT). However, there is increasing evidence that other tonometers share this problem.4–6 The GAT, Tono-Pen, ocular blood flow tonograph (OBF), and non-contact tonometer (NCT) all use an applanation principle. Thin shell theory was used by Orssengo and Pye to demonstrate that corneal radius, thickness and material stiffness affect the applanation pressure for a given IOP. Reducing the applanation area reduces the difference between the applanation pressure and IOP, because of the reduced resistance offered by the cornea for a smaller contact area.7 There may also be some reduced effects from surface tension.
The GAT is based on the Imbert-Fick law,1,8 which assumes that the cornea has a dry surface, is infinitely thin, and behaves as a “membrane” where the applanating pressure will equal the IOP. In practice, a resistance force, because of the thickness of the cornea, and a surface tension force, the result of the tear film, act upon the applanator causing this membrane assumption to be incorrect. These forces balance each other for the GAT (applanation diameter of 3.06 mm) when the CCT is 520 μm, providing a “reference” value where the applanating pressure does equal the IOP.1
The NCT uses a puff of air directed at the cornea with an applanation area, for the Canon TX-10, similar to that of the GAT. The force produced by the air puff is linearly increased over 8 ms and progressively flattens the cornea. When flat, the cornea acts as a mirror reflecting a light beam onto a sensor that triggers a reading. The Tono-Pen works on a principle similar to the MacKay-Marg tonometer9 and has an applanation area smaller (2.36 mm2) than that of the GAT (7.35 mm2).10 The OBF, or pneumatonometer, measures the pressure in a flowing column of gas (tonometer chamber) directed towards a thin membrane (diameter about 2.5 mm) in contact with the surface of the cornea. The probe tip has an outer diameter of about 5 mm. A portion of the gas flow pushes the outer part of the tonometer tip against the cornea, depressing its surface, and a portion maintains the pressure required to balance the pressure on the other side of the tip membrane (that is, the IOP) in the central part of the probe tip.11,12 The probe tip applanates the cornea for about 5–10 seconds while a continuous IOP trace is recorded.
In the companion paper, we reported the level of agreement between IOP measurements made with the GAT, Tono-Pen XL, OBF, and Canon TX-10 NCT. The effect of CCT and subject age on tonometric measurements made with these four techniques is described in this paper. The study reported in this paper is the first to compare all four tonometric methods in the same eyes.
MATERIALS AND METHODS
Details of the study design, and materials and methods have been given in the companion paper. Table 1 of the companion paper lists patient data, CCT values and range of IOP measurements made with the four tonometers.
Table 1.
Association between measured intraocular pressure and central corneal thickness for each method, as determined by linear regression analysis
| Slope | 95% CI for slope | Adjusted R2 | p Value | |
| GAT 1 | 0.028 | 0.006 to 0.049 | 0.05 | 0.011 |
| GAT 2 | 0.026 | 0.0002 to 0.051 | 0.04 | 0.033 |
| Tono-Pen | 0.031 | 0.010 to 0.053 | 0.07 | 0.004 |
| OBF | 0.038 | 0.009 to 0.068 | 0.05 | 0.012 |
| NCT | 0.046 | 0.022 to 0.070 | 0.12 | 0.000 |
Statistical analyses
Linear regression analysis was used to explore the relations between measured IOP and CCT and subject age and between tonometry inter-method differences and CCT and age. With 105 subjects, the study had a power of 80% at p = 0.05 to detect a correlation of 0.245 (≡ r2 0.06) between measured IOP and CCT (one sided test). Estimation of the effect of age was a post hoc analysis justified by suggestions in the literature that the cornea stiffens with age.13–15
The relation between tonometry inter-method differences and CCT and inter-method mean IOP was sought by stepwise multiple linear regression (CCT and IOP as the independent variables; probability of F to enter = 0.05 and to remove = 0.10).
RESULTS
The association of measured IOP and CCT with each tonometer is summarised in table 1. The effect of CCT was least for the GAT and greatest for NCT, although the 95% confidence limits for the slopes overlapped for all four methods.
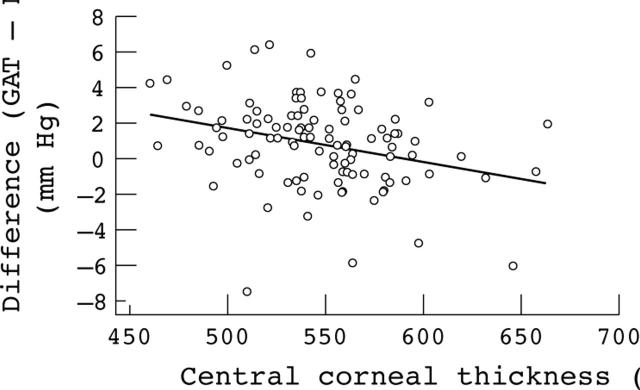
The GAT/NCT differences were significantly related to CCT for both GAT observers (see fig 1 for GAT observer 1); the equations were:
Figure 1.
Differences between intraocular pressure measurements made with the Goldmann applanation tonometer by observer 1 and those made with the Canon TX-10 non-contact tonometer plotted against central corneal thickness.
Observer 1: GAT/NCT difference = (−0.187×CCT) + 10.9 (adjusted R2 = 0.07; p = 0.003)
Observer 2: GAT/NCT difference = (−0.199×CCT) + 12.0 (adjusted R2 = 0.08; p = 0.002)
GAT/NCT differences were significantly related both to method mean IOP and to CCT for GAT observer 1 only; the equations were:
GAT/NCT difference = (−0.129×IOP) + (−0.014×CCT) + 10.5 (adjusted R2 = 0.11; p = 0.02 for the IOP coefficient and p = 0.03 for the CCT coefficient). Thus, the difference between GAT observer 1 and NCT increased both with the level of IOP and CCT.
OBF/NCT differences were also significantly related to IOP and CCT; the equation was:
OBF/NCT difference = (−0.218×IOP) + (−0.018×CCT) + 6.7 (adjusted R2 = 0.12; p = 0.0003 for the IOP coefficient and p = 0.03 for the CCT coefficient)
GAT/tonometer differences for other pairs of instruments were not related to CCT.
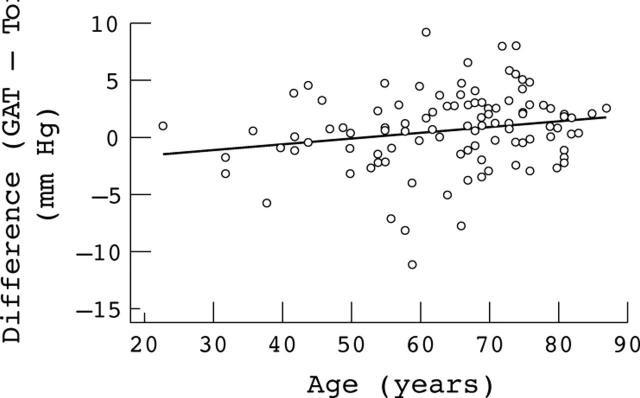
CCT and IOP measured by each tonometer were unrelated to subject age. However, GAT/Tono-Pen (fig 2) and OBF/Tono-Pen differences were significantly related to subject age; the equations were:
Figure 2.
Differences between intraocular pressure measurements made with the Goldmann applanation tonometer by observer 1 and those made with the Tono-Pen plotted against subject age.
GAT/Tono-Pen difference = (0.05×age) − 2.70 (adjusted R2 = 0.04; p = 0.035)
OBF/Tono-Pen difference = (0.06×age) − 3.51 (adjusted R2 = 0.04; p = 0.045)
DISCUSSION
Several studies have examined the relation between IOP measured by various tonometers and CCT (table 2). The findings from an early study, in which eyes were cannulated and true IOP was measured with a manometer, showed an average tonometric (Perkins or Draeger) error of ±0.7 mm Hg per 10 μm deviation of CCT from the normal thickness of 520 μm.1 A lower average correction of 0.18–0.23 mm Hg per 10 μm was observed by Whitacre et al in a similar in vivo study in 15 eyes with normal corneas.2 This latter finding is close to that found in the present study. However, an association between applanation tonometry error (the difference between Tono-Pen or Perkins tonometer and manometric IOP) and CCT was not found by Feltgen et al16 or Foster et al.17
Table 2.
Increase in IOP (mm Hg) for every 10 μm increase in CCT. Summary of previous findings regarding effect of CCT on IOP measurements
| Author | Study type | Country | GAT | Tono-Pen | OBF | NCT |
| This study | Clinic based | United Kingdom | 0.28 | 0.31 | 0.38 | 0.46 |
| Ko et al, 20046 | Clinic based | Taiwan | 0.37 | 0.47 | 0.63 | |
| Siganos et al, 200436 | Clinic based | Greece | 0.26 | 0.39 | ||
| Bhan et al, 20025 | Clinic based | United Kingdom | 0.23 | 0.10 | 0.28 | |
| Gunvant et al, 200421 | Clinic based | United Kingdom | 0.27 | 0.48 | ||
| Morgan et al, 200312 | Clinic based | United Kingdom | 0.30 | |||
| Shimmyo et al, 200322 | Clinic based | United States | 0.16 | |||
| Eysteinsson et al, 200223 | Population based | Iceland | 0.22 (M) | |||
| 0.28 (F) | ||||||
| Dohadwala et al, 19984 | Population based | Indian subcontinent | 0.29 (M) | |||
| 0.12 (F) | ||||||
| Foster et al, 200324 | Population based | Singapore | 0.15 (R) | |||
| 0.18 (L) | ||||||
| Foster et al, 199825 | Population based | Mongolia | 0.18 (R) | |||
| 0.24 (L) | ||||||
| Wolfs et al, 199738 | Population based | Netherlands | 0.19 | |||
| Nemesure et al, 200339 | Population based | Barbados | none | |||
| Feltgen et al, 200116 | Manometry | Germany | none | |||
| Foster et al, 200017 | Manometry | Singapore | none | |||
| Ehlers, 19751 | Manometry | Denmark | 0.71 |
M, male; R, right eye; F, female; L, left eye.
In general, there is good agreement between clinic based and population based studies of an increase in GAT measured IOP as CCT increases (table 2). The slope estimates in clinic based studies are slightly steeper than those in population based studies. This may result from a bias introduced by referral patterns, where tonometry is almost universally performed for glaucoma case finding.
NCT was significantly more susceptible to the effects of CCT than GAT, in accordance with previous findings.18–20 The slope of the relation GAT/NCT difference versus CCT was about −0.2 mm Hg per 10 μm, compared to −0.37 mm Hg per 10 μm reported by Graf.18 In clinic and population studies, CCT explains between 1% and 6% of the variance in GAT measured IOP and 7% to 12% of the variance in NCT measured IOP.21–25 A possible explanation of the greater effect of CCT on NCT measured IOP lies in the viscoelastic property of the cornea,26 in which stiffness is related to the rate of application of strain. The cornea is deformed over about 8 ms, resulting in relatively greater stiffness than under the conditions of GAT, where IOP measurement is effectively static. Other possible explanations include the relative effects of ocular expansion in the rapid and slow applanation conditions and the effect of pressure waves reflected back and forth through the eye with rapid applanation. A new NCT, the ocular response analyser (ORA; Reichert Inc, Depew, NY, USA), exploits the viscoelastic properties of the cornea. The ORA measures two applanation events, one as the pressure in the air jet rises and one as it falls. There is a difference in pressure for the inward and outward applanation events—a property called hysteresis. Preliminary data suggest that the hysteresis value correlates well with CCT.27
We observed an overestimation of IOP by NCT relative to GAT and OBF at higher IOP levels. Possible explanations include a non-linear increase in corneal stiffness as IOP rises and corneal viscoelastic properties that are not accounted for by CCT. A small tonographic effect was seen with one of the GAT observers and with the OBF, so there may be a contribution from the effect of reduced aqueous outflow facility on measured IOP differences, the effect being greater on tonometry with very rapid flattening of the cornea.
The finding in this study of an increase in IOP measured by the Tono-Pen of 0.31 mm Hg per 10 μm increase in CCT is greater than previously reported figures of 0.19 mm Hg/10 μm4 and 0.10 mm Hg/10 μm5 (table 2), although the confidence intervals for the estimate are wide (table 1). It is thought that the Tono-Pen may be less affected by CCT than the GAT because it applanates a smaller area of the cornea.7,10
Walker and Litovitz28 proposed that IOP measurements by pneumotonometry would be little affected by CCT as flexural rigidity could be ignored, because the outer edges of the probe flatten the cornea and the tension forces, by which IOP is measured, occur under the central portion of the probe. However, this and other studies have reported a dependence of OBF measured IOP on CCT.5,12,21,29 An explanation is provided by Morgan et al.12 A portion of the air flow of the pneumotonometer holds the probe against the cornea to provide the initial corneal flattening and is susceptible to the effects of the CCT.
The results of a re-analysis of published data demonstrated that a 10% difference in CCT results in a difference of 1.1 (SD 0.6) mm Hg in IOP measurements,30 equivalent to a change of 0.20 mm Hg for every 10 μm change in CCT. This result is supported by more recent findings (table 2). The validity of this relation is based on the assumption of a linear dependence of measured IOP on CCT, and on the absence of a relation between true IOP and CCT. Ehlers et al found a significant (p<0.001) correlation between the error of GAT IOP readings and CCT. However, the relation was non-linear, and IOP measurements required correction for CCT in relation to true IOP.1 The latter findings were confirmed by Orssengo and Pye, who demonstrated that the modulus of elasticity of the cornea was related to true IOP.7
Opinion is divided about the clinical significance of the effect of CCT on IOP measurements. Singh et al suggested that the effect was small and probably not relevant for most patients.29 Conversely, a recent report suggested that a correction for corneal effects might be needed for some groups of patients.5 In a literature review, Doughty and Zaman reported a mean CCT of 544 (SD 34) μm for measurements made by ultrasound pachymetry.30 From this, 95% of corneas should have a CCT in the range 477–611 μm. If a value of 0.20 mm Hg IOP increase per 10 μm increase in CCT is assumed,30 then the CCT could account for a difference in measured IOP of 2.7 mm Hg between the thickest and the thinnest corneas. One in 20 eyes will fall outside these extremes. Although this difference may be quite small in relation to the GAT measurement error, the distribution of CCT values in clinic populations is unlikely to reflect that of the general population. Falsely high IOP readings made (especially by NCT) in the community will lead to a concentration of thicker corneas in clinic populations. Thus, CCT measurement is useful to identify normal eyes falsely classified as ocular hypertensive. Similarly, the classification of eyes on the basis of IOP as normal or high tension glaucoma inevitably leads to a relatively greater proportion of eyes with thin corneas in the normal tension group.
The cornea is thought to stiffen with age13 as a result of ultrastructural changes in the collagen fibrils of the corneal stroma.14,15 The finding of a significant relation between GAT/Tono-Pen (fig 2) and OBF/Tonopen differences and subject age, with GAT and OBF overestimating IOP relative to the Tono-Pen in older subjects, may be explained by a stiffer cornea in older subjects, if Tono-Pen IOP measurements are less dependent on the biomechanical properties of the cornea. An effect of a reduced tear film may contribute. Eisenberg et al31 measured IOP by manometry, Perkins tonometry, pneumotonometry, and the Tono-Pen in nine subjects aged from 0.1 to 85 years. There was a significant effect of subject age on Perkins IOP measurement error, but not on the measurement error of the Tono-Pen and pneumotonometry. The Perkins overestimated the Tono-Pen at older ages. The magnitude of the effect in present study was a relative increase in measured IOP (by GAT or OBF over the Tono-Pen) of about 0.5 mm Hg per decade, or 3.2 mm Hg across the age range of subjects in the study.
The effect of corneal biomechanics on IOP measurement is a research area that is gaining importance, given the increasing prevalence of individuals having undergone corneal refractive surgery. Stromal thinning following refractive procedures has been demonstrated to result in changes in IOP measured by the GAT, NCT, and Tono-Pen.32–34 A new method of tonometry, the Pascal dynamic contour tonometer (DCT; Ziemer Ophthalmic Systems AG, Port Switzerland), is said not to be affected by corneal biomechanical properties. The applanation tip has a concave surface (radius of curvature 10.5 mm) with an embedded pressure sensor and, when contour matching between the tonometer tip and the cornea is achieved, the mechanical properties of the cornea do not contribute to the IOP measurement. Two studies have reported that DCT measured IOP is independent of CCT35,36 and studies on patients undergoing laser corneal refractive surgery have demonstrated that, unlike GAT IOP measurements, Pascal IOP measurements are unaltered by the laser surgery.36,37
In conclusion, the findings of the present study demonstrate that IOP measurements by the GAT, Tono-Pen, OBF, and NCT are all significantly influenced by CCT, and that the effect of CCT on NCT is significantly greater than on the GAT.
Acknowledgments
The authors thank Haag-Streit UK for providing the Canon TX-10 non-contact tonometer and the reviewer, Dr Gunvant, for the suggestion to explore tonometer measurement differences with respect to subject age.
Abbreviations
CCT, central corneal thickness
DCT, dynamic contour tonometer
GAT, Goldmann applanation tonometer
IOP, intraocular pressure
NCT, non-contact tonometer
OBF, ocular blood flow
ORA, ocular response analyser
REFERENCES
- 1.Ehlers N, Bramsen T, Sperling S. Applanation tonometry and central corneal thickness. Acta Ophthalmol 1975;53:34. [DOI] [PubMed] [Google Scholar]
- 2.Whitacre MM, Stein RA, Hassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol 1993;115:592–6. [DOI] [PubMed] [Google Scholar]
- 3.Gordon MO, Beiser JA, Brandt JD, et al. The ocular hypertension treatment study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120:714–20. [DOI] [PubMed] [Google Scholar]
- 4.Dohadwala AA, Munger R, Damji KF. Positive correlation between Tono-Pen intraocular pressure and central corneal thickness. Ophthalmology 1998;105:1849–54. [DOI] [PubMed] [Google Scholar]
- 5.Bhan A, Browning AC, Shah S, et al. Effect of corneal thickness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer, and Tono-Pen. Invest Ophthalmol Vis Sci 2002;43:1389–92. [PubMed] [Google Scholar]
- 6.Ko YC, Liu CL, Hsu WM. Varying Effects of corneal thickness on intraocular pressure measurements with different tonometers. Eye 2004;16:16. [DOI] [PubMed] [Google Scholar]
- 7.Orssengo GJ, Pye DC. Determination of the true intraocular pressure and modulus of elasticity of the human cornea in vivo. Bull Math Biol 1999;61:551–72. [DOI] [PubMed] [Google Scholar]
- 8.Gloster J, Perkins ES. The validity of the Imbert-Flick law as applied to applanation tonometry. Exp Eye Res 1963;44:274–83. [DOI] [PubMed] [Google Scholar]
- 9.Mackay RS, Marg E, Oechsli R. Automatic tonometer with exact theory: various biological applications. Science 1960;131:1668–9. [DOI] [PubMed] [Google Scholar]
- 10.Mok KH, Wong CS, Lee VW. Tono-Pen tonometer and corneal thickness. Eye 1999;13:35–7. [DOI] [PubMed] [Google Scholar]
- 11.Silver DM, Farrell RA. Validity of pulsatile ocular blood flow measurements. Surv Ophthalmol 1994;38:S72–80. [DOI] [PubMed] [Google Scholar]
- 12.Morgan AJ, Harper J, Hosking SL, et al. The effect of corneal thickness and corneal curvature on pneumatonometer measurements. Curr Eye Res 2002;25:107–12. [DOI] [PubMed] [Google Scholar]
- 13.Friedenwald JS. Contribution to the theory and practice of tonometry. Am J Ophthalmol 1937;20:985. [Google Scholar]
- 14.Malik NS, Moss SJ, Ahmed N, et al. Ageing of the human corneal stroma: structural and biochemical changes. Biochim Biophys Acta 1992;1138:222–8. [DOI] [PubMed] [Google Scholar]
- 15.Daxer A, Misof K, Grabner B, et al. Collagen fibrils in the human corneal stroma: structure and aging. Invest Ophthalmol Vis Sci 1998;39:644–8. [PubMed] [Google Scholar]
- 16.Feltgen N, Leifert D, Funk J. Correlation between central corneal thickness, applanation tonometry, and direct intracameral IOP readings. Br J Ophthalmol 2001;85:85–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foster PJ, Wong JS, Wong E, et al. Accuracy of clinical estimates of intraocular pressure in Chinese eyes. Ophthalmology 2000;107:1816–21. [DOI] [PubMed] [Google Scholar]
- 18.Graf M. [Significance of the corneal thickness in non-contact tonometry]. Klin Monatsbl Augenheilkd 1991;199:183–6. [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto T, Makino H, Uozato H, et al. The influence of corneal thickness and curvature on the difference between intraocular pressure measurements obtained with a non-contact tonometer and those with a Goldmann applanation tonometer. Jpn J Ophthalmol 2000;44:691. [DOI] [PubMed] [Google Scholar]
- 20.Recep OF, Hasiripi H, Cagil N, et al. Relation between corneal thickness and intraocular pressure measurement by noncontact and applanation tonometry. J Cataract Refract Surg 2001;27:1787–91. [DOI] [PubMed] [Google Scholar]
- 21.Gunvant P, Baskaran M, Vijaya L, et al. Effect of corneal parameters on measurements using the pulsatile ocular blood flow tonograph and Goldmann applanation tonometer. Br J Ophthalmol 2004;88:518–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shimmyo M, Ross AJ, Moy A, et al. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am J Ophthalmol 2003;136:603–13. [DOI] [PubMed] [Google Scholar]
- 23.Eysteinsson T, Jonasson F, Sasaki H, et al. Central corneal thickness, radius of the corneal curvature and intraocular pressure in normal subjects using non-contact techniques: Reykjavik Eye Study. Acta Ophthalmol Scand 2002;80:11–5. [DOI] [PubMed] [Google Scholar]
- 24.Foster PJ, Machin D, Wong TY, et al. Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study. Invest Ophthalmol Vis Sci 2003;44:3885–91. [DOI] [PubMed] [Google Scholar]
- 25.Foster PJ, Baasanhu J, Alsbirk PH, et al. Central corneal thickness and intraocular pressure in a Mongolian population. Ophthalmology 1998;105:969–73. [DOI] [PubMed] [Google Scholar]
- 26.Hjortdal JO, Jensen PK. In vitro measurement of corneal strain, thickness, and curvature using digital image processing. Acta Ophthalmol Scand 1995;73:5–11. [DOI] [PubMed] [Google Scholar]
- 27.Kotecha A, Shewry JM, Garway-Heath DF. Corneal thickness independent IOP measurements [abstract]. Invest Ophthalmol Vis Sci 2004;45 ARVO Abstract 956. [Google Scholar]
- 28.Walker RE, Litovitz TL. An experimental and theoretical study of the pneumatic tonometer. Exp Eye Res 1972;13:14–23. [DOI] [PubMed] [Google Scholar]
- 29.Singh RP, Goldberg I, Graham SL, et al. Central corneal thickness, tonometry, and ocular dimensions in glaucoma and ocular hypertension. J Glaucoma 2001;10:206–10. [DOI] [PubMed] [Google Scholar]
- 30.Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol 2000;44:367–408. [DOI] [PubMed] [Google Scholar]
- 31.Eisenberg DL, Sherman BG, McKeown CA, et al. Tonometry in adults and children. A manometric evaluation of pneumatonometry, applanation, and TonoPen in vitro and in vivo. Ophthalmology 1998;105:1173–81. [DOI] [PubMed] [Google Scholar]
- 32.Mardelli PG, Piebenga LW, Whitacre MM, et al. The effect of excimer laser photorefractive keratectomy on intraocular pressure measurements using the Goldmann applanation tonometer. Ophthalmology 1997;104945–8; discussion 949,. [DOI] [PubMed] [Google Scholar]
- 33.Chatterjee A, Shah S, Bessant DA, et al. Reduction in intraocular pressure after excimer laser photorefractive keratectomy. Correlation with pretreatment myopia. Ophthalmology 1997;104:355–9. [DOI] [PubMed] [Google Scholar]
- 34.Garzozi HJ, Chung HS, Lang Y, et al. Intraocular pressure and photorefractive keratectomy: a comparison of three different tonometers. Cornea 2001;20:33–6. [DOI] [PubMed] [Google Scholar]
- 35.Kaufmann C, Bachmann LM, Thiel MA. Comparison of dynamic contour tonometry with goldmann applanation tonometry. Invest Ophthalmol Vis Sci 2004;45:3118–21. [DOI] [PubMed] [Google Scholar]
- 36.Siganos DS, Papastergiou GI, Moedas C. Assessment of the Pascal dynamic contour tonometer in monitoring intraocular pressure in unoperated eyes and eyes after LASIK. J Cataract Refract Surg 2004;30:746–51. [DOI] [PubMed] [Google Scholar]
- 37.Kaufmann C, Bachmann LM, Thiel MA. Intraocular pressure measurements using dynamic contour tonometry after laser in situ keratomileusis. Invest Ophthalmol Vis Sci 2003;44:3790–4. [DOI] [PubMed] [Google Scholar]
- 38.Wolfs RC, Klaver CC, Vingerling JR, et al. Distribution of central corneal thickness and its association with intraocular pressure: the Rotterdam Study. Am J Ophthalmol 1997;123:767–72. [DOI] [PubMed] [Google Scholar]
- 39.Nemesure B, Wu SY, Hennis A, et al. Corneal thickness and intraocular pressure in the Barbados eye studies. Arch Ophthalmol 2003;121:240–4. [DOI] [PubMed] [Google Scholar]