Abstract
Aim: To describe the experience of using electron beam tomography (EBT) in imaging of osteo-odonto-keratoprosthesis (OOKP) to identify early bone and dentine loss which may threaten the viability of the eye.
Methods: Seven patients with an OOKP in one eye underwent EBT. The OOKP lamina dimensions were measured on EBT and compared to the manual measurements at the time of surgery.
Results: There was a high degree of resolution of the OOKP lamina noted with EBT. In particular, it identified three patients with a marked degree of thinning of the lamina edges. Two of these patients had OOKP that were allografts. The mean time from surgery to examination was 3.6 years (range 1.2–5 years) while the mean age of the patients was 56 years (range 31–79 years).
Conclusions: It is important to monitor regularly the dimensions and stability of the OOKP lamina as it will help detect cases that are at risk of extrusion of the optical cylinder and consequent endophthalmitis. Prophylactic measures can then be taken to prevent such serious complications from occurring. In this series, the authors found EBT to have excellent resolution and speed and they would support regular scanning of the OOKP lamina in all patients.
Keywords: osteo-odonto-keratoprosthesis, electron beam tomography
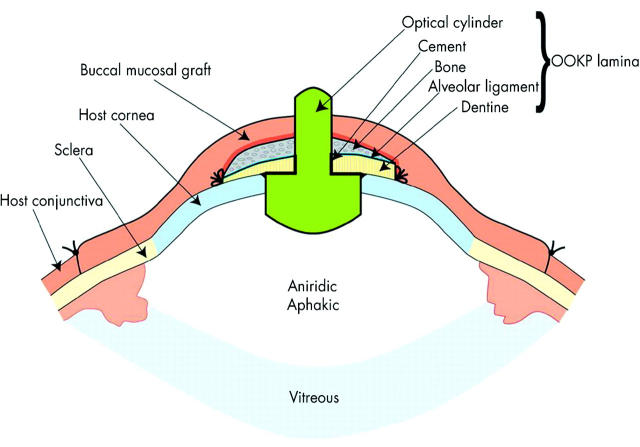
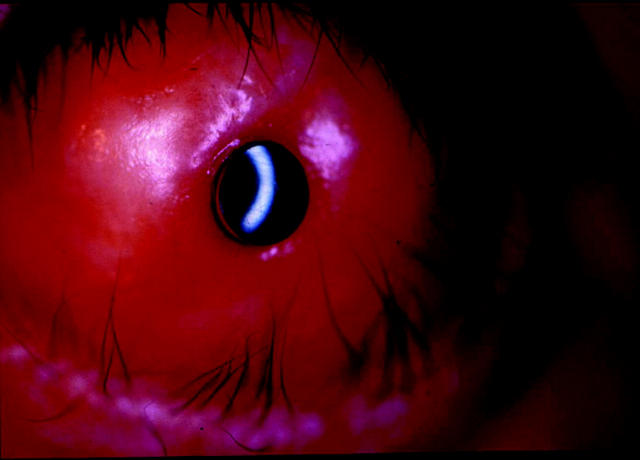
The osteo-odonto-keratoprosthesis (OOKP) as described by Strampelli1 with the modifications by Falcinelli et al2 and Liu et al3 provides good long term results in patients who are not amenable to any other type of conventional corneal transplantation. The keratoprosthesis (KPro) consists of an optical cylinder made from poly(methylmethacrylate) (PMMA) and a supporting lamina prepared from a single rooted tooth with its supporting alveolar bone (fig 1). This is usually covered with a buccal mucous membrane graft (fig 2) but should there be insufficient mucous membrane available, the patient’s own lid skin after removal of the tarsal plate can be using in a “transpalpebral” approach.4
Figure 1.
Cross sectional diagram describing the anatomy and structure of an osteo-odonto-keratoprosthesis.
Figure 2.
Appearance of a healthy OOKP with a buccal mucous membrane graft overlying it.
The critical feature for the long term stability of the OOKP appears to be in the maintenance of the osteo-odonto-lamina. Reduction in the dimensions of the laminae can result in aqueous leakage, inflammation, extrusion of the optical cylinder, and endophthalmitis. As such, it is important to detect such cases of lamina resorption so that prophylactic measures can be taken to prevent such complications from occurring. Imaging techniques such as electron beam tomography (EBT) and multidetector computed tomography (MDCT) are valuable in detecting such cases. Other methods of imaging like B-scan ultrasonography are limited because the lamina causes sound attenuation and shadowing while magnetic resonance imaging (MRI) is subject to movement artefact with poor spatial resolution and conventional CT only allows two dimensional reconstruction.5 Image acquisition with MRI is also longer than CT.
The ability of EBT to detect dentine and bone loss in OOKP was studied in a series of patients.
METHODS
EBT was performed in seven patients after successful OOKP surgery. The study was carried with approval from the local research ethics committee and informed consent was obtained from all patients before the EBT was performed. In all eyes, the osteo-odonto-lamina was covered by a buccal mucous membrane graft. EBT (GE Imatron, GE Medical Systems, USA) with the patient in the supine position was performed using the following parameters: axial plane scan with an acquisition time = 100 ms, slice thickness = 1.5 mm, table feed = 1 mm, and pitch = 0.66. Three dimensional volumetric reconstruction of the OOKP was then performed using an Aquarius Terarecon Workstation. Maximum intensity projections (MIP) and shaded surface display (SSD) techniques were then used to calculate the dimensions of the OOKP lamina. These dimensions were then correlated with those obtained at the time of surgery.
According to the degree of bone reduction, the lamina were classified using a score that grades bone reduction6: osteo-odonto-lamina that presented with no reduction compared with preoperative baseline measurements was classified as belonging to group 0. Lamina with minor reductions was classified as group 1. Lamina with moderate reductions of dentine and bone loss but still displaying a tight fixation of the optic cylinder was considered group 2. Lamina showing severe destruction of tissue and therefore at high risk of spontaneous loss of the optical cylinder was classed as group 3.
RESULTS
Table 1 summarises the clinical data of all the patients in the study. The mean age of the patients was 52 years (range 32–79 years) and the mean time from surgery to EBT was 38 months (range 12–62 months). In all patients, EBT with three dimensional surface reconstruction was feasible with a high level of resolution (figs 3 and 4). Minor reductions of the lamina could be seen in all the patients, mainly in the inferior rim. Patient 4 was found to have thinning of the nasal rim of the OOKP (fig 5) while patient 3 had marked thinning of the inferior rim (figs 6 and 7).
Table 1.
Patient details and OOKP lamina dimensions
| Patient No | Sex | Age (years) | Diagnosis | Allograft/autograft | Lamina dimensions at surgery (mm) | Lamina dimensions at EBT (mm) | Grade of bone reduction | Visual acuity | Time to EBT (months) | |
| Preop | Postop | |||||||||
| 1 | M | 40 | SJS | Autograft | 11×7×2.3 | 11×7×2.1 | 1 | HM | 6/12 | 62 |
| 2 | M | 79 | SJS | Autograft | 11.5×7×2.1 | 11.5×7×2.1 | 0 | HM | 6/9 | 60 |
| 3 | M | 33 | SJS | Autograft | 11×9×2.5 | 11×7×2.4 (inferior rim = 0.9) | 3 | HM | 6/9 | 52 |
| 4 | F | 77 | OCP | Allograft | 12.5×8.5×2.5 | 9×5×2.4 (nasal rim = 1.3) | 2 | PL | CF | 36 |
| 5 | F | 68 | SJS | Autograft | 11×7.5×3 | 11×7.5×2.5 | 0 | HM | 6/9 | 16 |
| 6 | F | 32 | SJS | Autograft | 11×7.5×2.5 | 11×6.7×2.2 | 0 | PL | 6/6 | 26 |
| 7 | M | 32 | Ectodermal dyplasia | Allograft | 12×7.5×2.5 | 11×6.3×2 (inferior rim resorption) | 1 | CF | 6/9 | 12 |
SJS, Stevens-Johnson syndrome; OCP, ocular cicatricial pemphigoid; CF, counting fingers; HM, hand movements; PL, perception of light.
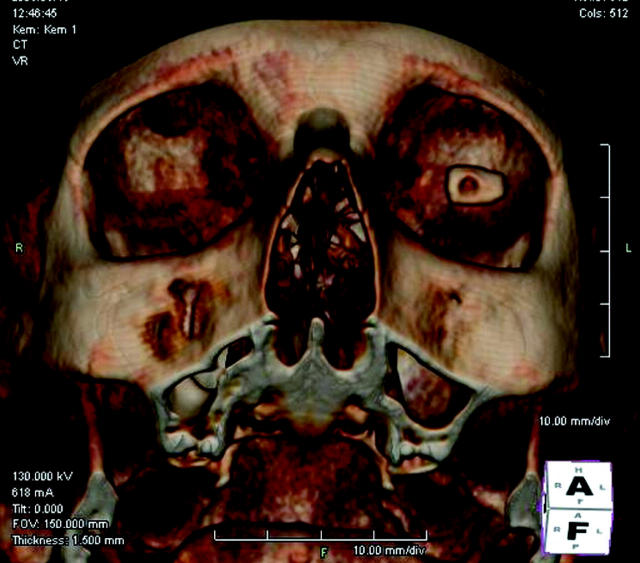
Figure 3.
Frontal view of electron beam tomography of the left eye of patient 6 showing a well defined osteo-odonto-keratoprosthesis lamina with a good rim around the optic.
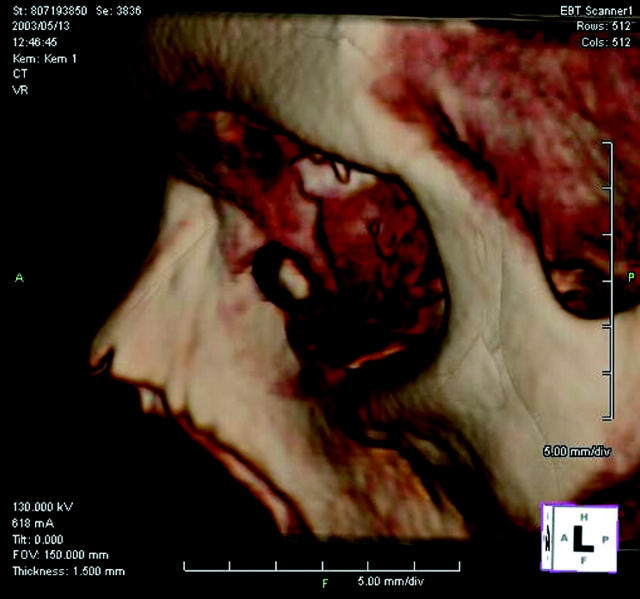
Figure 4.
Lateral view of electron beam tomography of the left eye of patient 6.
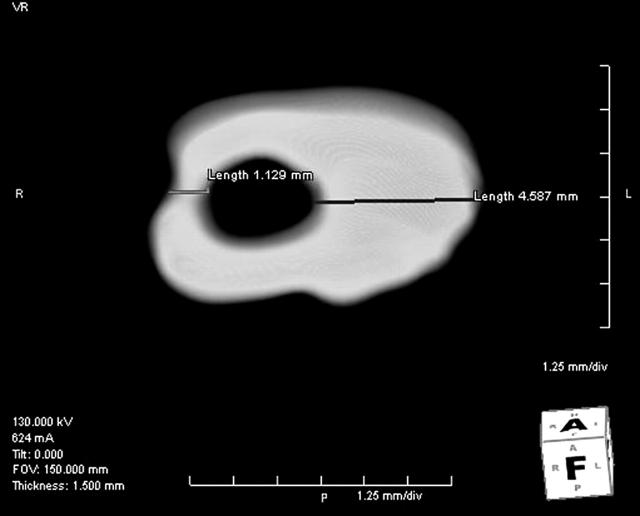
Figure 5.
Detailed shaded surface display reconstruction of left osteo-odonto-keratoprosthesis of patient 4 showing the nasal rim to measure only 1.3 mm in thickness.
Figure 6.
Electron beam tomography of osteo-odonto-keratoprosthesis in the left eye of patient 3 showing significant thinning of the inferior rim. The right eye is phthisical and calcified.
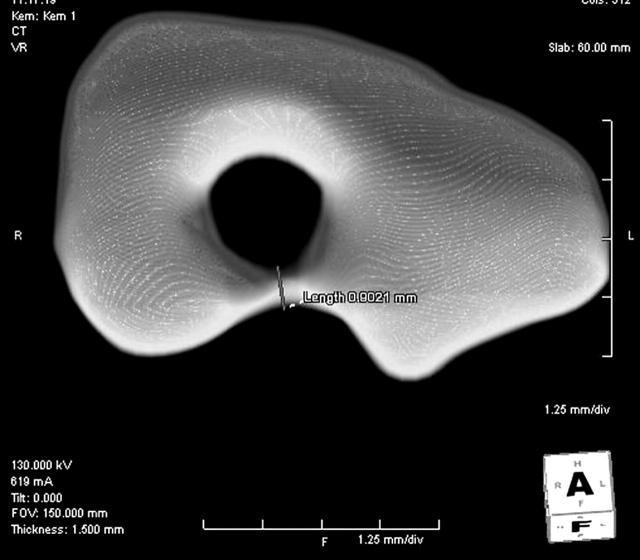
Figure 7.
Detailed shaded surface display reconstruction of left osteo-odonto-keratoprosthesis from figure 6 showing the inferior rim measuring only 0.9 mm.
Five of the patients received an autologous osteo-odonto-lamina while the other two patients had teeth and surrounding jaw bone harvested from a living related donor followed by long term immunosuppression with ciclosporin A. Indications for surgery included Stevens-Johnson syndrome, ocular cicatricial pemphigoid, and ectodermal dysplasia syndrome.
DISCUSSION
The use of a KPro is usually a last surgical attempt to restore vision in patients not amenable to conventional corneal transplantation or other types of ocular surface reconstruction such as amniotic membrane or stem cell grafting. Many types of KPros have been developed and implanted in patients over the past two decades with variable long term success. These include the Dohlman-Doane7 KPro (now known as the Boston KPro), the AlphaCor artificial cornea (Argus Biomedical, Australia) (previously known as the Chirila KPro),8 the Pintucci KPro,9 and the OOKP, as described by Strampelli1 and modified by Falcinelli et al.2
The OOKP shows good long term results10 but the surgeon must be constantly aware of signs of resorption of the osteo-odonto-lamina. The potential risks associated with reduction of the lamina means that regular assessment of its state is needed. B-scan echography with an ultrasound biomicroscope (UBM) can be used in evaluating the anterior segment before OOKP surgery but is of limited value after surgery because the lamina causes sound attenuation and shadowing.11 MRI5 and conventional CT12 make two dimensional reconstruction of the axial or coronal planes of the OOKP possible giving a vague impression of the condition of the OOKP.
MDCT with three dimensional surface reconstruction (Toshiba X-press/SX, Toshiba Corporation, Japan) were recently used in nine patients with OOKP.6 The dimensions of the OOKP were measured and compared with the measurements taken at the time of surgery. A minor reduction in laminae, mainly in the anterior and inferior part, could be found in all the patients. In one patient, there was complete resorption of the inferior half of the laminae (79 years old, ocular pemphigoid, autograft, laminae covered with lower lid skin, OOKP surgery 24 months before scan). No correlation between the degree of reduction in the dimensions and patient age, diagnosis, or length of follow up could be found. The degree of resolution on MDCT was impressive as even Baerveldt glaucoma implants were visible on the scans.
EBT is a modified form of computed tomography and utilises electron beams that are focused onto tungsten target rings positioned beneath the patient. This is then passed to an array of detectors that generates cross sectional images. EBT is rapid (50–100 ms per scan) and is widely used for evaluating cardiac function,13 coronary artery calcium content,14 and blood flow analysis.15 EBT has two advantages over MDCT in that lower doses of radiation are involved (one third that of MDCT) and image acquisition by EBT is much more rapid thus reducing the potential problem of movement artefact. Problems in defining the actual dimensions of the OOKP relate to the fact that the alveolar and denticular bone have a wide range of densities and the target of the scan is small and close to the spatial limits of resolution of either modality. MDCT will deliver higher quality images with greater signal to noise in the data sets obtained but at greater exposure to radiation dose. As it is likely that these patients will require imaging of their OOKP lamina on a regular basis, EBT will expose the patient to lower cumulative doses of radiation over the lifetime of the patient.
In our series of patients, EBT of the OOKP was feasible with a high degree of resolution obtained. We have used the results of the EBT to manage our OOKP patients more proactively in that patients with high degrees of bone reduction (grade 2 or 3) are monitored more frequently. In the case of patient 3 with a very thin inferior OOKP rim detected on EBT, this represented an eye at high risk of OOKP extrusion and possible endophthalmitis. As such, after discussion with the patient, prophylactic removal of the OOKP followed by a tectonic corneal graft was performed. The very thin inferior rim was confirmed visually when the OOKP was explanted, thus suggesting a good correlation between the EBT findings and the true in vivo condition of the OOKP. A new OOKP lamina was fashioned and the patient has since had a new OOKP implanted in his eye with a good result. Frequent follow up of high risk patients allowed us to detect early leakage of aqueous fluid from the allograft OOKP of patient 7. The patient underwent emergency removal of the OOKP followed by a tectonic corneal graft to preserve the globe integrity and visual function. He is now awaiting another KPro.
Histopathological analysis of explanted OOKPs suggests that chronic inflammation has an important role in the dissolution of the osteo-odonto-lamina.16–18 Bony tissue was found to be focally replaced by connective tissue, there was a reduction in dentine and a layer of immature woven bone surrounded the remnants. The alveolo-dental ligament appears to have an important role in the preservation of the osteo-odonto-lamina. This is because in places where the ligament was found to be preserved, no destruction of the bone or dentine could be found. The ligament probably acts as a kind of seal against epithelial downgrowth between the optical PMMA cylinder and the tooth.17
In our series, most of the resorption seen on EBT occurred in the inferior part of the lamina. This could be because the OOKP is usually implanted with the thicker part of the OOKP located superiorly. Stoiber et al6 suggest that bone resorption is less in the superior rim of the OOKP because the alveolo-dental ligament is more under tension superiorly owing to the presence of the upper lid. Lack of tension in the inferior rim may push the balance between bone formation and resorption towards gradual resorption in that area.
To the best of our knowledge, this is the first reported series of patients with OOKP who have undergone EBT to monitor the thickness and structure of the OOKP laminae and we could not find any reference to this in a computerised search using Medline. Our results show that life long follow up is necessary for patients with OOKP. Up to recently, there was no reliable method of imaging the lamina precisely in vivo. It is now possible to image the lamina with modalities like EBT or MDCT and significant thinning of the lamina has been found using both modalities. This allows closer follow up of this group of patients to look out for signs of aqueous leakage, optic extrusion, or inflammation. In the case of patients with significant lamina thinning, prophylactic measures like removing the OOKP and preparing a new OOKP may be considered to preserve the structure and function of the eye. Both EBT and MDCT appear to be practical and accurate diagnostic tools in imaging the OOKP. We would recommend a baseline morphological assessment of the OOKP initially by either EBT or MDCT after the OOKP has been implanted to define the dimensions radiologically. We would then regularly monitor the dimensions of the OOKP with clinical assessment to identify cases at risk of optic extrusion and consequent endophthalmitis.
Abbreviations
EBT, electron beam tomography
KPro, keratoprosthesis
MDCT, multidetector computed tomography
MIP, maximum intensity projections
MRI, magnetic resonance imaging
OOKP, osteo-odonto-keratoprosthesis
SSD, shaded surface display
Competing interests: none declared
REFERENCES
- 1.Strampelli B. Keratoprosthesis with osteodental tissue. Am J Ophthalmol 1963;89:1029–39. [Google Scholar]
- 2.Falcinelli G, Barogi G, Taloni M, et al. Osteoodontokeratoprosthesis: present experience and future prospects. Refract Corneal Surg 1993;9:193–4. [Google Scholar]
- 3.Liu CSC, Scisio A, Smith GT, et al. Indications and technique of modern osteo-odonto-keratoprosthesis (OOKP) surgery. Eye News 1998;4:17–22. [Google Scholar]
- 4.Marchi V, Ricci R, Pecorella I, et al. Osteo-odonto-keratoprosthesis: description of surgical technique with results in 85 patients. Cornea 1994;13:125–30. [PubMed] [Google Scholar]
- 5.Bellelli A, Avitto A, Liberali M, et al. Osteo-odonto-keratoprosthesis. Radiographic, CT and MR features. Radiol Med (Torino) 2001;102:143–7. [PubMed] [Google Scholar]
- 6.Stoiber J, Forstner R, Csaky D, et al. Evaluation of bone reduction in osteo-odontokeratoprosthesis (OOKP) by three-dimensional computed tomography. Cornea 2003;22:126–30. [DOI] [PubMed] [Google Scholar]
- 7.Dohlman CH, Waller SG, Netland PA. Keratoprosthesis surgery. In: Linquist TD, Lindstrom RI, eds. In: Ophthalmic surgery update. 4th ed. Vol V–L. Chicago: Mosby Year Book, 1996:1–32.
- 8.Hicks CR, Crawford GJ, Lou X, et al. Corneal replacement using a synthetic hydrogel cornea, AlphaCor: device, preliminary outcomes and complications. Eye 2003;17:385–92. [DOI] [PubMed] [Google Scholar]
- 9.Pintucci S, Pintucci F, Caiazza S, et al. The Dacron felt colonizable keratoprosthesis: after 15 years. Eur J Ophthalmol 1996;6:125–30. [DOI] [PubMed] [Google Scholar]
- 10.Liu CSC, Pagliarni S. Independent survey of long term results of the Falcinelli osteo-odonto-keratoprosthesis (OOKP). An Inst Barraquer (Barc) 1999;28:91–3. [Google Scholar]
- 11.Colliardo P, Avitabile T, Buratto E, et al. Echography in osteo-odonto-keratoprosthesis. An Inst Barraquer (Barc) 1999;28:137–8. [Google Scholar]
- 12.Taloni M, Manni T, Micozzi I, et al. Computerized tomography study of the osteo-odonto-acrylic lamina. An Inst Barraquer (Barc) 1999;28:145–7. [Google Scholar]
- 13.Thomas PJ, McCollough CH, Ritman EL. An electron-beam CT approach for transvenous coronary arteriography. J Comput Assist Tomogr 1995;19:383–9. [DOI] [PubMed] [Google Scholar]
- 14.Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. [DOI] [PubMed] [Google Scholar]
- 15.Budoff MJ, Oudiz CP, Zalace CP, et al. Intravenous three-dimensional coronary angiography using contrast-enhanced electron beam computed tomography. Am J Cardiol 1999;83:840–5. [DOI] [PubMed] [Google Scholar]
- 16.Caiazza S, Falcinelli G, Pintucci S. Exceptional case of bone resorption in an osteo-odonto-keratoprosthesis: a scanning electron microscopy and x-ray microanalysis study. Cornea 1990;9:23–7. [PubMed] [Google Scholar]
- 17.Ricci R, Pecorella I, Della Rocca C, et al. Strampelli’s osteo-odonto-keratoprosthesis: clinical and histologic long-term features of three prosthesis. Br J Ophthalmol 1992;76:232–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stoiber J, Csaky D, Schedle A, et al. Histopathologic findings in explanted osteo-odontokeratoprosthesis. Cornea 2002;21:400–4. [DOI] [PubMed] [Google Scholar]