Abstract
Aim: To investigate how long patients’ improved visual function lasts after a cataract extraction.
Methods: Patients’ self assessed visual function was evaluated using the Catquest questionnaire both before and 6 months after a cataract extraction. The study population consisted of 615 patients undergoing a cataract extraction during 1995–2002. A final follow up with a new questionnaire was performed in 2003, between 1 year and 8 years after surgery.
Results: 445 (72.4%) patients were alive at follow up and agreed to participate in the study. The number of subjects still showing improved visual function after surgery decreased with longer follow up. After 7 years, 80% had improved visual function compared with before surgery. 50% of all originally operated subjects were alive 7 years postoperatively and enjoyed better visual function than they had done before surgery. Ocular co-morbidity in the operated eye or self assessed poor visual function before surgery was significantly related to deteriorated visual function at follow up.
Conclusion: The number of subjects who experienced improved visual function after a cataract extraction decreased over the course of time postoperatively. Presence of ocular co-morbidity was significantly related to worsened function.
Keywords: cataract extraction, visual function
Patients’ self assessed visual function is regarded as the single most important variable when priority for cataract surgery is determined.1 This variable has also been considered as the most important outcome measure in a cataract extraction.2 A number of questionnaires for evaluating patients’ self assessed visual function have therefore been designed.3–6 The cataract questionnaire Catquest5,7 has been used in the outcome studies performed by the Swedish National Cataract Register (NCR).8 The impact of a cataract extraction on self assessed visual function and, consequently, on the quality of life (QoL) of a patient has been found to be very good.3–6
An important question in health economics analyses is how long improvement in visual function will last after a cataract extraction. This question has rarely been addressed in the literature except in a number of life expectancy studies in patients postoperatively.9–11 Also, two utility studies have discussed the question, estimating the duration of benefit from cataract surgery to be 5 years12 and 12 years.13 The aim of the present study was to analyse self assessed visual function in patients operated for cataract 1–8 years previously and to compare this result with their self assessed visual function both before and 6 months after surgery.
MATERIALS AND METHODS
The Department of Ophthalmology at Blekinge Hospital in Karlskrona, Sweden, has participated in the outcome studies performed by the Swedish NCR8 since 1995. These outcome studies have included all cataract extractions performed during the month of March each year. A questionnaire for cataract patients, Catquest, has been included in the data collection performed as part of the outcome study.5,7 The Catquest contains questions about degree of difficulty in performing seven common and vision dependent activities in daily life. The total possible disability score sum (DS) ranges from 7 (“no difficulty at all”) to 34 (“giving up doing the activity” because of poor vision). This questionnaire was completed by the patients before surgery and 6 months after surgery. In addition to the questionnaire, data were collected prospectively for each patient, according to the protocol of the NCR.8 During the period under study (1995–2002) a total of 622 operations performed at the Department of Ophthalmology, Blekinge Hospital, were included in the outcome study, with full outcome data and completed questionnaires. Patients operated on both eyes during the study period (March) but during different years (n = 7) were included only once (year of first eye surgery). This means that 615 patients were included in the present study. In April 2003, when the present study started, 523 patients were still alive and a new Catquest questionnaire was sent to them by mail. In addition, a new short questionnaire was sent out with questions regarding changes in self assessed visual function and information on any ocular surgeries performed, recent ocular diagnoses, and any general diseases since the primary cataract extraction. The patients’ ophthalmic records were checked with regard to any visits since the primary surgery.
RESULTS
Study population and excluded cases
The patients in this study were recruited from eight cataract surgery cohorts undergoing surgery between 1995 and 2002. Demographic data for each cohort are shown in table 1. The total DS, according to the Catquest, before and 6 months after surgery differed between the surgical cohorts but there was no obvious trend over time (table 1).
Table 1.
Demographic data for each surgical cohort included in the study
| Year of surgery | No | Mean/median age (years) | Women (%) | VA, | DS (median value) | ||
| Operated eye (median) | Better eye (median) | Preop | Postop (6 months) | ||||
| 1995 | 49 | 75.8/77 | 65.3 | 0.2 | 0.5 | 11 | 8 |
| 1996 | 45 | 77.7/79 | 66.7 | 0.2 | 0.6 | 14 | 8 |
| 1997 | 49 | 76.7/78 | 65.3 | 0.3 | 0.7 | 11 | 7 |
| 1998 | 73 | 76.1/77 | 61.6 | 0.3 | 0.7 | 14 | 8 |
| 1999 | 93 | 76.2/78 | 63.4 | 0.3 | 0.6 | 13 | 7 |
| 2000 | 83 | 76.2/78 | 63.9 | 0.4 | 0.8 | 11 | 7 |
| 2001 | 98 | 74.5/77 | 62.2 | 0.4 | 0.8 | 13 | 7 |
| 2002 | 125 | 76.2/77 | 60.8 | 0.4 | 0.7 | 13 | 7 |
DS, total disability score sum, as defined by the Catquest.
VA, visual acuity, decimal notation.
Postop = postoperatively; preop = preoperatively.
The number of patients originally included who were still alive and responded to the last questionnaire is shown in table 2.
Table 2.
Number of operated patients, patients still alive at follow up, and patients who completed the questionnaire at follow up, by year of surgery
| Year of surgery | Total No of patients included | Still alive | Completed questionnaire |
| 1995 | 49 | 27 (55.1%) | 24 |
| 1996 | 45 | 30 (66.7%) | 23 |
| 1997 | 49 | 40 (81.6%) | 34 |
| 1998 | 73 | 56 (76.7%) | 51 |
| 1999 | 93 | 80 (86.0%) | 66 |
| 2000 | 83 | 75 (90.4%) | 63 |
| 2001 | 98 | 93 (94.9%) | 83 |
| 2002 | 125 | 122 (97.6%) | 101 |
| Total during period | 615 | 523 (85.0%) | 445 (72.4%) |
Altogether, 615 patients were initially included in the study. In April 2003, when the present study was performed, 523 (85%) were still alive, and 473 (90.4%) responded to the last questionnaire and agreed to participate in the study. However, 28 questionnaires were returned incomplete, which means that 445 patients were included in the final analysis. In table 3 demographic data are compared between deceased subjects, subjects responding incompletely or not at all (“Not responding”), and subjects included in the final study. There was no large difference in the preoperative DS between the three groups. The difference in mean age at surgery among the eight surgical cohorts was small. The mean age at follow up in 2003 varied from 82.5 years (surgery in 1995) to 76.1 years (surgery in 2002). Patients who did not respond had a lower preoperative DS and poorer preoperative visual acuity (VA). The non-respondents’ improvement, in terms of VA and DS, after surgery was not as good as that of patients who did respond to the follow up questionnaire (data not shown).
Table 3.
Demographic data at the time of surgery for deceased subjects, subjects not responding to the questionnaire, and subjects included in the final analysis
| Subjects | p Value* | |||
| Dead | Not responding | Included | ||
| No | 92 | 78 | 445 | |
| Women (%) | 56.5 | 55.7 | 65.8 | |
| Mean age (years) | 81.1 | 77.6 | 74.7 | |
| VA, surgery eye (median) | 0.2 | 0.1 | 0.4 | |
| VA, better eye (median) | 0.6 | 0.6 | 0.7 | |
| Ocular co-morbidity (%) | 65.2 | 48.1 | 38.2 | |
| Second eye surgery (%) | 39.1 | 29.1 | 35.1 | |
| Total DS† (median (mean)) | 13 (14.1) | 11 (12.2) | 12 (13.1) | 0.319 |
*Calculated using the Kruskal-Wallis test.
†With a possible score range of 7–34.
DS, disability score.
Most of the cataract extractions were performed using phacoemulsification (94.4%), with 62.5% of operations done by this method in 1995 and almost 100% done by this method during the last two study years (table 4). An intraocular lens was implanted in the posterior chamber in all eyes except one, which was left aphakic.
Table 4.
Number (%) of patients with higher, unchanged, and lower DS at follow up (2003) compared with preoperative DS. The table also shows the percentage of operations done by phacoemulsification, and the relation between surgical technique and higher DS
| Year of surgery | Lower | Unchanged | Higher | Phaco (%) | Higher (phaco/ECCE) |
| 1995 | 15 (62.5%) | 3 (12.5%) | 6 (25.0%) | 62.5 | 4/2 |
| 1996 | 18 (78.3%) | 1 (4.3%) | 4 (17.4%) | 95.7 | 4/0 |
| 1997 | 28 (82.4%) | 2 (5.8%) | 4 (11.8%) | 82.4 | 3/1 |
| 1998 | 35 (68.6%) | 4 (7.9%) | 12 (23.5%) | 88.2 | 9/3 |
| 1999 | 49 (74.2%) | 5 (7.6%) | 12 (18.2%) | 98.5 | 11/1 |
| 2000 | 51 (81%) | 7 (11.1%) | 5 (7.9%) | 98.4 | 5/0 |
| 2001 | 69 (83.1%) | 9 (10.9%) | 5 (6.0%) | 100.0 | 5/0 |
| 2002 | 79 (78.2%) | 11 (10.9%) | 11 (10.9%) | 99.0 | 10/1 |
| Total | 344 (77.3%) | 42 (9.4%) | 59 (13.3%) | 94.4 | 51/8 |
ECCE, extracapsular cataract extraction; phaco, phacoemulsification.
Benefit of surgery at follow up
In 77.3% of all respondents the total DS was lower at follow up than it was before surgery, which means that the benefits of the operation had lasted. In 9.4% the score was unchanged while in 13.3% the DS was higher than before surgery—in other words, their condition had worsened. The longer the follow up the greater the number of subjects with higher DS. Analysis of variance (ANOVA) showed that the relation between time after surgery and higher DS compared with before surgery was statistically significant (p = 0.006). Table 4 shows the changes in DS for each year of follow up. There was a statistically significant relation between a higher DS (that is, a worsened condition) at follow up and the existence of an ocular co-morbidity in the operated eye before surgery (p<0.001; χ2 test). As many as 22.9% of cases with an ocular co-morbidity before surgery had worsened, compared with 7.3% of cases with no ocular co-morbidity. There was no significant relation between surgical technique and benefit of surgery at follow up for any year of surgery (table 4).
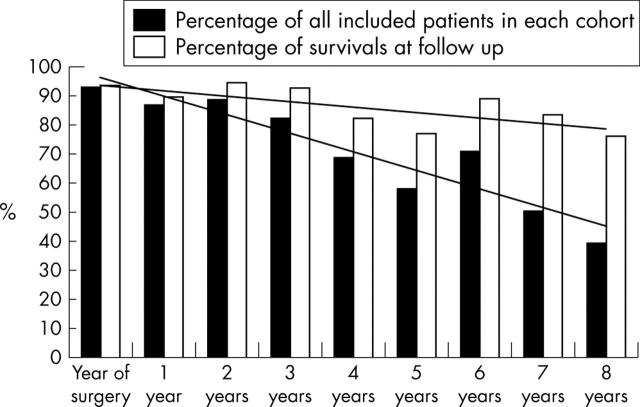
Mean and median DS before surgery, 6 months after surgery, and at follow up are shown in table 5. The DS for the total number of cases at follow up was significantly higher in patients with an ocular co-morbidity than in patients with no co-morbidity (p<0.001, Mann-Whitney U test). The percentage of patients with improved DS at follow up compared with the preoperative DS is shown in figure 1. Trend lines based on observations show that among those alive at follow up about 80% still had improved visual function 7 years after surgery. If all originally operated patients are included, about 50% still had improved visual function 7 years after surgery.
Table 5.
Mean and median DS before surgery, 6 months after surgery, and at follow up for subjects with and without an ocular co-morbidity
| Before surgery | After 6 months | At follow up | ||
| No ocular co-morbidity (n = 275) | Mean | 12.25 | 7.73 | 7.68 |
| Median | 12.00 | 7.00 | 7.00 | |
| Ocular co-morbidity (n = 170) | Mean | 14.36 | 10.59 | 11.39 |
| Median | 14.00 | 9.00 | 9.00 | |
Figure 1.
Percentage of patients with either lasting improvement or a DS, at follow up, which is equal to the preoperative DS. The figure shows the percentage of all operated and included patients in each cohort compared with the percentage of patients still living at follow up.
Benefit of surgery, and first and second eye surgery
The cataract surgery investigated was first eye surgery with no further surgery in 98 cases (22.0%), second eye surgery in 156 cases (35.1%), and first eye surgery when the study started followed by second eye surgery during the follow up period in 191 cases (42.9%).
Irrespective of which DS (that is, before surgery, 6 months after surgery, or at follow up) was compared, there was no significant difference between the three treatment groups (data not shown).
Benefit of surgery, and new diseases during follow up
During the follow up period 72 patients had a new eye disease in the operated eye. In 35 cases this was an age related macular degeneration (ARMD), while in 12 cases it was glaucoma; in five cases diabetic retinopathy, and in 20 cases, another unspecified eye disease. A new serious general disease occurred during the follow up period in 93 cases. Nineteen patients had a stroke, 15 had cancer, 13 had a cardiac infarction, seven had diabetes, and in 39 cases another disease was diagnosed. Deterioration in self assessed visual function during follow up was significantly related to the occurrence of a new ocular co-morbidity in the operated eye. This was true both for subjects originally without any ocular co-morbidity in the operated eye (p<0.001; χ2 test) and for subjects with such an ocular co-morbidity (p = 0.013; χ2 test). There was no significant relation between deterioration in self assessed visual function during follow up and the occurrence of a new serious general disease.
Benefit of surgery, and preoperative condition
The relation between deterioration in self assessed visual function after surgery and demographic data including co-morbidity was tested in a logistic regression analysis. Only two variables were significantly related to a worse outcome: DS 6 months after surgery (p<0.001) and the occurrence of a preoperative ocular co-morbidity (p = 0.015). A new logistic analysis was performed separately on cases with and cases without occurrence of a preoperative ocular co-morbidity. In cases with no preoperative ocular co-morbidity the only variable that was significantly related to a worse outcome at follow up was the occurrence of an ARMD in the operated eye during the follow up period (p = 0.030; logistic regression analysis). In cases with a preoperative ocular co-morbidity the DS 6 months after surgery was the only variable that was significantly related to a worse outcome (p<0.001; logistic regression analysis).
DISCUSSION
Cataract extraction has been stated to be a very cost effective procedure.12,13 Three variables must be known in order to support this statement, however: the cost of surgery, the impact of surgery on visual function, and the duration of the improved function after surgery. The cost of a cataract extraction has been studied previously,14,15 and the functional outcome has been extensively reported in the literature.3–6 To our knowledge, however, this study represents the first report of the duration of functional improvement after a cataract extraction. We have used patients’ self assessed visual function as an outcome measure.
This study has a number of limitations. We followed up eight cohorts of cataract surgery cases. Each cohort consisted of consecutive cases operated during 1 month over the previous 1–8 years. This study design was used as a substitute for a longitudinal follow up study of one group of patients operated in the same year. This design may introduce a source of error owing to variation among the cohorts when interpreting the results. The study cohorts represent consecutive cases, without any specific selection, during eight different years; however, over the course of time there were changes in both indications for surgery and surgical technique. Despite this potential source of error the outcome measure, DS, in this study did not differ significantly between the cohorts, either before or 6 months after surgery. Because of the different lengths of follow up, the cohorts had a mean age varying from 76.1 years to 82.5 years at follow up. With regard to age at surgery, the studies performed by the NCR8 showed that age as a single variable, if corrected for the occurrence of other eye diseases, does not influence the DS. Our findings indicate that the number of individuals who continue to benefit from a cataract extraction decreases with time after surgery. A significant loss of cases as a result of death of subjects occurred during follow up. Among those still alive at follow up there was a difference in DS between respondents and non-respondents. This may introduce an error, as non-respondents tend to be less healthy, with a poorer prognosis, than are those who respond to questionnaires.7 The mortality rate in the original group of included subjects was identical to that reported previously for a larger group of cataract surgery patients from the same area.16 Among surviving patients, age was not related to a higher percentage of worsened visual function in our study. The occurrence of an ocular co-morbidity (mostly ARMD) before or after surgery was related to deteriorated visual function. The occurrence of new general diseases after the cataract extraction did not significantly influence visual function. The influence of complications and a more detailed risk analysis will be discussed elsewhere.
Acknowledgments
We would like to thank Jonas Ranstam for valuable help with statistics.
Abbreviations
ANOVA, analysis of variance
ARMD, age related macular degeneration
DS, total disability score sum
ECCE, extracapsular cataract extraction
NCR, national cataract register
QoL, quality of life
VA, visual acuity
Competing interests: none declared
REFERENCES
- 1.Romanchuk KG, Sanmugasunderam S, Hadorn DC. Developing cataract surgery priority criteria: results from the Western Canada Waiting List Project. Can J Ophthalmol 2002;37:145–54. [DOI] [PubMed] [Google Scholar]
- 2.Cataract Management Guideline Panel. Cataract in adults: management of functional impairment. Rockville, MD: US Department of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research, 1993 (AHCPR Publication No 93-0542; Clinical Practice Guideline No 4,.
- 3.Mangione CM, Phillips RS, Seddon JM, et al. Development of the “Activities of Daily Vision Scale.” A measure of visual functional status. Med Care 1992;30:1111–26. [DOI] [PubMed] [Google Scholar]
- 4.Steinberg EP, Tielsch JM, Schein OD, et al. The VF-14: an index of functional impairment in patients with cataract. Arch Ophthalmol 1994;112:630–8. [DOI] [PubMed] [Google Scholar]
- 5.Lundström M, Jensen S, Fregell G, et al. Catquest questionnaire for use in cataract surgery care: description, validity and reliability. J Cataract Refract Surg 1997;23:1226–36. [DOI] [PubMed] [Google Scholar]
- 6.Mangione CM. NEI VFQ-25 scoring algorithm. Bethesda, MD: National Eye Institute, 1997.
- 7.Lundström M, Stenevi U, Thorburn W, et al. Catquest questionnaire for use in cataract surgery care: assessment of surgical outcomes. J Cataract Refract Surg 1998;75:688–91. [DOI] [PubMed] [Google Scholar]
- 8.Lundström M, Stenevi U, Thorburn W. The Swedish National Cataract Register: a 9-year review. Acta Ophthalmol Scand 2002;80:248–57. [DOI] [PubMed] [Google Scholar]
- 9.Meddings DR, Marion SA, Barer ML, et al. Mortality rates after cataract extraction. Epidemiology 1999;10:288–93. [PubMed] [Google Scholar]
- 10.McKibbin M, Mohammed M, James TE, et al. Short-term mortality among middle-aged cataract surgery patients. Eye 2001;15:209–12. [DOI] [PubMed] [Google Scholar]
- 11.Ninn-Pedersen K, Stenevi U. Cataract patients in a defined Swedish population, 1986–90; VII. Inpatient and outpatient standardised mortality ratios. Br J Ophthalmol 1995;79:1115–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobelt G, Lundström M, Stenevi U. Measuring utility and outcome in cataract surgery. J Cataract Refract Surg 2002;28:1742–9. [DOI] [PubMed] [Google Scholar]
- 13.Busbee BG, Brown MM, Brown GC, et al. Incremental cost-effectiveness of initial cataract surgery. Ophthalmology 2002;109:606–13. [DOI] [PubMed] [Google Scholar]
- 14.Lundström M, Brege KG, Florén I, et al. Cataract surgery and effectiveness. 1. Variation in costs between different providers of cataract surgery. Acta Ophthalmol Scand 2000;78:335–9. [DOI] [PubMed] [Google Scholar]
- 15.Filer J, Roberts-Harry TJ, Jagger JD. Cutting the cost of cataract surgery—a financial audit. Br J Ophthalmol 1991;75:227–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lundström M, Albrecht S. Previous cataract surgery in a defined Swedish population. J Cataract Refract Surg 2003;29:50–6. [DOI] [PubMed] [Google Scholar]