Abstract
Aims: To define the frequency of seeing (FOS) characteristics of the short wavelength (SW) sensitive visual pathway in clinically normal subjects and in diabetic patients with focal SW sensitivity loss.
Methods: For clinically normal subjects, FOS was assessed at two retinal locations (4.24° and 9.90° eccentricity) for both white on white (WW) and SW stimulus parameters. Interexamination variability was quantified for the clinically normal subjects only. For patients with diabetes, FOS was assessed inside an area of focal SW sensitivity loss, and at the same eccentricity in the quadrant diametrically opposite, using SW stimulus parameters only.
Results: For clinically normal subjects, the group mean SW FOS slope was significantly flatter (p<0.0001) than that of WW at both locations. The coefficient of repeatability for SW FOS slope was ±41.55 dB−1 (relative to a group mean sensitivity of 23.98 dB−1) and ±19.98 dB−1 (group mean sensitivity 16.15 dB−1) for 4.24° and 9.90°, respectively. For the patients with diabetes, the group mean SW FOS slope was significantly flatter (p = 0.020), and group mean SW threshold significantly higher (p = 0.007) in the area of focal SW sensitivity loss than in that of the non-focal sensitivity loss.
Conclusions: The results of this study suggest that the clinical utility of SW automated perimetry will be limited by a greater magnitude of measurement variability, as indicated by a flatter FOS slope, compared to conventional automated perimetry.
Keywords: short wavelength perimetry, frequency of seeing, short term fluctuation, psychometric function, diabetes, children
Short wavelength automated perimetry (SWAP) detects glaucomatous visual field damage earlier than white on white (WW) perimetry.1–4 Other studies have investigated progression of visual field defects using SWAP5–8 and also demonstrated SW field loss in diabetic retinopathy and maculopathy9–14 before the occurrence of WW loss. SWAP may represent a useful clinical tool to aid the management of various ocular diseases.
SWAP exhibits a greater between subject variability and a greater short term fluctuation (SF; that is, variation of sensitivity within an examination), than WW perimetry.15–19 These two factors will reduce the potential of SWAP to detect abnormality and progression—that is, visual field loss will have to be greater to reach significance in areas of high variability.17 For WW perimetry, the lower the sensitivity at a given stimulus location the higher the SF.20 SF only provides an estimate of within examination variability. The magnitude of within examination variability is determined by the frequency of seeing (FOS) function21 that describes the probability of detecting a stimulus as a function of intensity. The flatter the slope of the FOS function, the greater the within examination variability. Previous studies have shown shallower FOS slopes in areas of visual field loss in glaucoma patients for WW and motion stimuli.22–25
The influence of sensitivity level and stimulus location on SWAP SF has to be established. This factor limits the accuracy of threshold determination and also governs the optimum bracketing procedure employed to estimate threshold. The aims of the study were to define the influence of (1) stimulus location on the FOS characteristics of the WW and SW sensitive visual pathways in clinically normal subjects; and (2) localised sensitivity loss on the FOS characteristics of the SW sensitive visual pathway in a diabetic patient group with focal diabetic macular oedema.
MATERIALS AND METHODS
Sample
Sixteen clinically normal subjects (10 males) and 10 patients with diabetes (six males) participated in the study. The study was approved by the research ethics board of the University Health Network, Toronto, Canada. Written informed consent was obtained from all volunteers.
Clinically normal group
The average age of the sample was 26 years (SD 8 years, 20–47 years). Ten right eyes and six left eyes were chosen at random. Inclusion criteria consisted of a logMAR visual acuity of 0.00, or better, a normal fundus appearance (stereo-biomicroscopy using dilated pupils), and normal visual fields (assessed by a minimum of one perimetry examination using Humphrey field analyser (HFA) II program 24-2). Exclusion criteria comprised (i) a distance refractive error of >±6.00 DS or ±1.50 DC, (ii) family history of glaucoma, (iii) a Goldmann IOP ⩾22 mm Hg (iv) central nervous system (CNS) disorders or psychiatric illness, (v) systemic medication with known CNS effects, and (vi) significant lenticular opacities (graded by the Lens Opacity Classification System III—that is, NO>1, NC>1, P>1, C>1).26
Patients with diabetes
The average age of the sample was 55 years (SD 9 years, 38–66 years). Five right eyes and five left eyes were used. Inclusion criteria consisted of a logMAR visual acuity of 0.50, or better, clinically evident focal diabetic macular oedema (DMO), and repeatable sensitivity loss (that is, ⩾5 contiguous stimulus locations of significantly reduced sensitivity as assessed by SWAP and horizontal hemifield asymmetry analysis9) on each of two separate occasions. Exclusion criteria were the same as those imposed for the clinically normal group, apart from LOCS III criteria.
Visits
All volunteers attended for two visits. Only the results from the second visit were analysed, thereby minimising learning effects for both perimetric paradigms.27 Visit 1 was used to undertake refraction, visual acuity (VA) and fundus examination and to perimetrically train volunteers (using WW and SW program 10-2). For the clinically normal group, visit 2 comprised two sessions of four FOS runs each (one before and one after lunch). The order of stimulus condition was randomised between subjects and retained for the post-lunch session. At visit 2, nine clinically normal subjects underwent WW stimulus parameters first. For the patients with diabetes, visit 2 comprised program 10-2 SWAP followed by two FOS test runs using SW stimulus parameters only. Volunteers were given rests every 5 minutes to minimise fatigue.28 The same FOS program was used for both clinically normal subjects and patients with diabetes.
Procedures
A HFA II model 740 (Carl Zeiss Meditec, Dublin, USA) and custom FOS software were utilised. The patient’s correction was adjusted for a viewing distance of 30 cm. For the WW stimulus parameters, a 10 cd/m2 background luminance and a Goldmann III (0.431° subtense) white stimulus were utilised. For the SW stimulus parameters, a high intensity yellow background (100 cd/m2) in conjunction with a Goldmann V (1.724° subtense) blue stimulus were utilised.29 Maximum stimulus intensity (that is, 0 dB) was 10 000 apostilbs and 65 apostilbs for WW and SW stimulus parameters, respectively. Stimulus duration was 200 ms. Fixation was assessed using the corneal reflex monitor and the Heijl-Krakau technique.
Frequency of seeing (FOS)
When performance is expressed as probability, psychometric functions are ogive, or S-shaped, in form. Volunteers were given 5 minutes to adapt to the background luminance before starting each FOS determination. For the clinically normal group, sensitivity was assessed at the fovea and five other retinal locations (at 5.66° eccentricity along the 135°, 225°, and 315° meridians, and at 4.24° and 9.90° along the 45° meridian) using an initial 4 dB crossing of threshold and then a 2 dB reversal. FOS functions were assessed at the 4.24° and 9.90° locations (one per location) along the 45° meridian at each session (fig 1). For the patients with diabetes, sensitivity was assessed for a location inside an area of focal SW sensitivity loss and at the same eccentricity in the quadrant diametrically opposite and at two other locations (one in each of the two remaining quadrants). A hemifield asymmetry analysis using SWAP program 10-2 identified localised areas of focal SW sensitivity loss.9 The hemifield asymmetry analysis compared individual asymmetry across the midline to asymmetry values of a database of normal values.
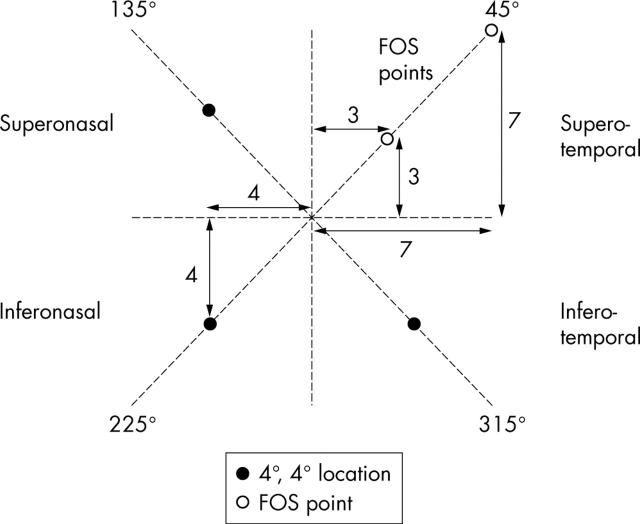
Figure 1.
Schematic diagram showing position of frequency of seeing (FOS) stimulus locations for clinically normal subjects (right eye). FOS stimulus locations were fixed for all subjects at 4.24° (polar coordinates 3°, 3°) and 9.90° (polar coordinates 7°, 7°) along the 45° meridian. Suprathreshold stimuli were presented at 5.66° (polar coordinates 4°, 4°) along the 135°, 225°, and 315° meridians.
For FOS testing, stimuli were presented randomly at preset sensitivity levels (selected by the operator) above and below the estimated threshold. The FOS functions were determined using eight sensitivity levels (two separate FOS test runs comprising four sensitivity levels each). Ten presentations were made at each sensitivity level. Sensitivity levels were selected for the first FOS run at ±1 dB and ±3 dB relative to the estimated threshold. The sensitivity levels for the second FOS run were then empirically chosen based upon the results of the first run. Volunteers who exhibited more than 25% false positive/negative responses or fixation losses were excluded from the analysis. Suprathreshold stimuli were randomly presented in order to introduce spatial uncertainty with the aim of maintaining global attention of the subject. No subjects were excluded because of excessive false positive/negative or fixation losses.
FOS function fitting
The FOS data were fitted using the following function:
P(I) = 1 − [0.5(−(S/α)β)]
where, P(I) is the probability of stimulus detection, S is sensitivity (dB), and α is a point on the x-axis (that is, sensitivity) that corresponds to a certain performance level.30 For this study, α was taken at 0.5 or 50% FOS. β is the slope of the central portion of the function. Statistica (Statsoft, Inc) was used to produce a least squares fit of the function. Sensitivity was compared within a given stimulus parameter (since comparison of sensitivity between WW and SW parameters is invalid owing to differing dynamic ranges). Sensitivity was taken at 50% FOS.
Statistical analysis
For the clinically normal group, slope and r value (that is, goodness of fit) of the FOS functions were compared between the different stimulus parameters (WW/SW). Sensitivity (that is, 50% FOS) was also included in the analysis to determine significant interactions with FOS slope and to monitor systematic change in sensitivity across the two sessions (that is, fatigue). A repeated measures analysis of variance (ANOVA) was undertaken on the data with slope and sensitivity as dependent variables and stimulus condition, eccentricity, and session as the within subject factors (SPSS Inc, Chicago, IL, USA). For the diabetic patient group, slope and sensitivity were compared between locations for SW stimulus parameters using Student’s t test (two tailed).
Intersession variability was quantified using the coefficient of repeatability (COR)31 for the clinically normal group using visit 2 session 1, and session 2 data—that is, 1.96 × SD of the differences across sessions.
RESULTS
Clinically normal group
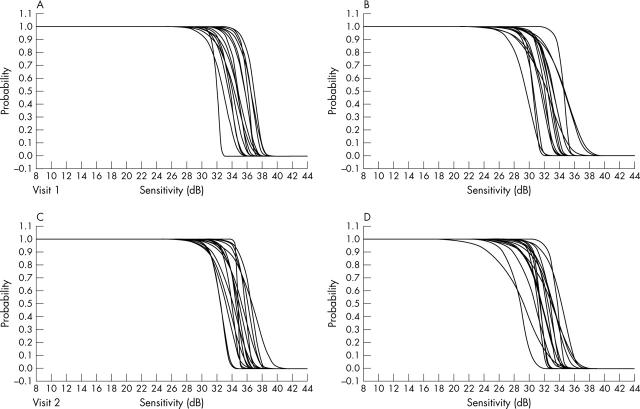
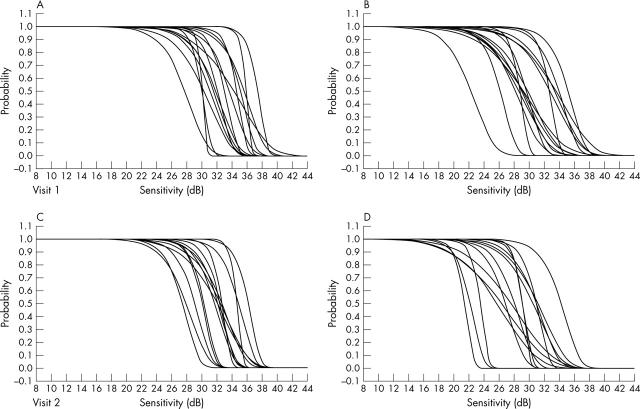
FOS functions of each clinically normal individual are shown for WW and SW stimulus parameters in figures 2 and 3, respectively. Test times to complete each session were not significantly different between sessions or parameters.
Figure 2.
Individual FOS functions using WW stimulus parameters for clinically normal subjects (A, B; session 1. C, D; session 2. A, C; 4.24° eccentricity. B, D; 9.90° eccentricity).
Figure 3.
Individual FOS functions using SW stimulus parameters for clinically normal subjects (A, B; session 1. C, D; session 2. A, C; 4.24° eccentricity. B, D; 9.90° eccentricity).
Group mean slope
Group mean FOS slope data are shown in table 1. The SW slopes were found to be significantly flatter than those attained using WW parameters (p<0.0001) and the slopes for both stimulus conditions were significantly flatter at 9.90° than at 4.24° (p = 0.0198) (figs 2 and 3). The interaction of slope, stimulus parameter and eccentricity was not significant.
Table 1.
Mean sensitivity and FOS slope for WW and SW stimulus parameters at 4.24° and 9.90° eccentricity for clinically normal subjects
| WW 4.24° | WW 9.90° | SW 4.24° | SW 9.90° | |||||
| Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | |
| Sensitivity (dB) | ||||||||
| Mean | 34.78 | 34.59 | 32.17 | 31.93 | 32.83 | 31.78 | 29.65 | 28.54 |
| SD | 1.76 | 1.28 | 1.88 | 1.50 | 2.63 | 2.40 | 3.41 | 2.89 |
| Slope (dB−1) | ||||||||
| Mean | 39.15 | 34.19 | 31.68 | 29.74 | 26.40 | 21.56 | 14.94 | 17.35 |
| SD | 14.20 | 10.52 | 12.70 | 13.85 | 17.80 | 11.36 | 8.78 | 9.00 |
Group mean sensitivity
Group mean FOS sensitivity data are shown in table 1. Sensitivity was significantly higher at 4.24° than at 9.90° (p<0.0001). Sensitivity was not significantly different across sessions.
Group mean r values
Group mean FOS r value data are shown in table 2. Values for r were consistently lower using SW stimulus parameters and at the more eccentric stimulus location.
Table 2.
Mean r value for WW and SW stimulus parameters at 4.24° and 9.90° eccentricity for clinically normal subjects
| rValue | WW 4.24° | WW 9.90° | SW 4.24° | SW 9.90° | ||||
| Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | Session 1 | Session 2 | |
| Mean | 0.99 | 0.98 | 0.99 | 0.97 | 0.96 | 0.97 | 0.94 | 0.94 |
| SD | 0.02 | 0.02 | 0.03 | 0.03 | 0.05 | 0.04 | 0.06 | 0.04 |
Repeatability of FOS determination
Intersession variability was quantified using the COR (table 3). The COR was calculated for the clinically normal group using the session 1 and session 2 data gathered at visit 2.
Table 3.
COR of sensitivity and FOS slope (relative to group mean) for WW and SW stimulus parameters at 4.24° and 9.90° eccentricity for clinically normal subjects
| WW | SW | |||
| 4.24° | 9.90° | 4.24° | 9.90° | |
| Sensitivity (dB) | ||||
| COR | ±2.85 | ±3.38 | ±3.86 | ±4.19 |
| Mean | 34.68 | 32.05 | 32.31 | 29.09 |
| Slope (dB−1) | ||||
| COR | ±30.76 | ±29.91 | ±41.55 | ±19.98 |
| Mean | 36.67 | 30.71 | 23.98 | 16.15 |
Patients with diabetes
Figure 4 shows typical FOS functions for a location within, and distant from, an area of focal sensitivity loss for a patient with diabetes.
Figure 4.
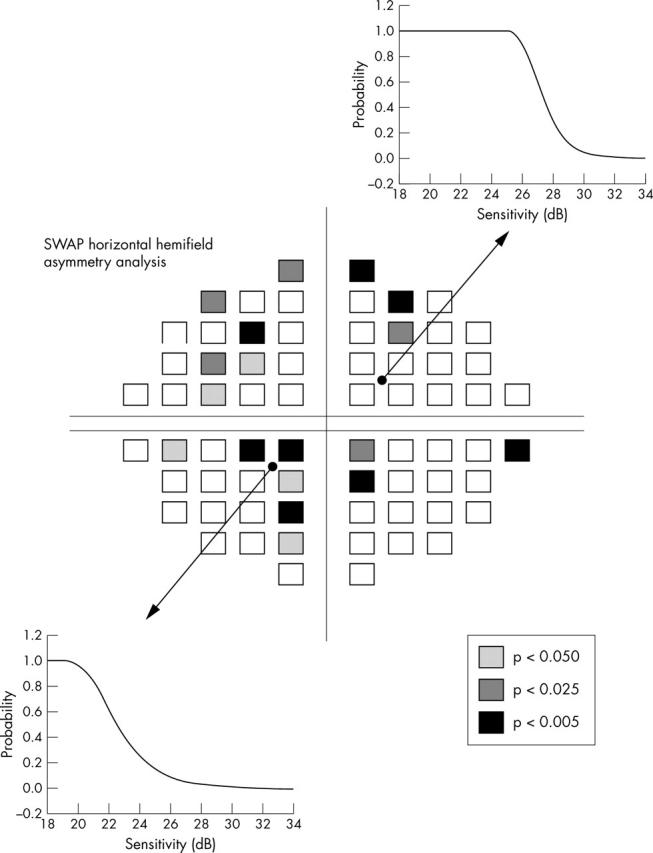
Individual horizontal hemifield analysis (right eye) and FOS functions using SW stimulus parameters for a patient with diabetes (upper; location distant from area of focal SW sensitivity loss. Lower; location within area of focal SW sensitivity loss. SWAP, short wavelength automated perimetry).
Group mean slope
The group mean SW slope values for the diabetic patients are shown in table 4. The SW slopes derived from the focal sensitivity loss location were found to be significantly flatter than those from the non-focal sensitivity loss location (p = 0.007).
Table 4.
Mean sensitivity and FOS slope for SW stimulus parameters at the diabetic macular oedema (DMO) and non-DMO location for patients with diabetes
| SW stimulus parameters | ||
| Non-DMO location | DMO location | |
| Sensitivity (dB) | ||
| Mean | 23.29 | 18.07 |
| SD | 4.80 | 5.05 |
| Slope (dB−1) | ||
| Mean | 16.59 | 7.87 |
| SD | 8.61 | 4.12 |
Group mean sensitivity
The group mean SW sensitivity values for the diabetic patients are shown in table 4. SW sensitivity attained at the focal sensitivity loss location was significantly lower than those attained at the non-focal sensitivity loss location (p = 0.020).
Group mean r values
Using SW stimulus parameters, the group mean r value at the non-focal sensitivity loss location was 0.964 (SD 0.04). At the focal sensitivity loss location, the group mean r value was 0.925 (SD 0.06). Values for r were consistently lower at the focal sensitivity loss location.
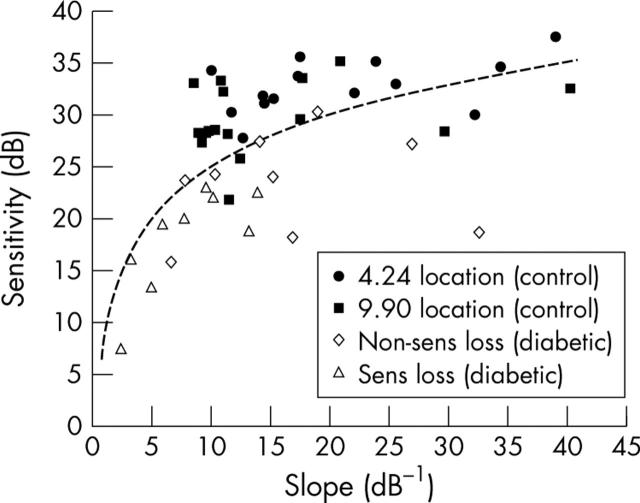
Figure 5 illustrates the relation between SW sensitivity (at 50% FOS) and SW FOS slope for the clinically normal subjects and patients with diabetes. It clearly shows a curvilinear relation between sensitivity and slope, with FOS slope becoming flatter in locations of lower sensitivity.
Figure 5.
Relation between SW sensitivity (at 50% FOS) and SW FOS slope for all volunteers. Clinically normal group: 4.24° location (solid circles); 9.90° location (solid squares). Patients with diabetes: location distant from area of focal sensitivity loss (open diamonds); location within area of focal sensitivity loss (open triangles). A logarithmic best fit line has been fitted to all the data (r = 0.6).
DISCUSSION
For the clinically normal group, the group mean slope of the FOS function using SW stimulus parameters was significantly flatter than that of WW (p<0.0001). For the patients with diabetes, SW FOS slope was flatter in locations of focal sensitivity loss compared to the non-focal sensitivity loss locations (p = 0.007) (fig 5).
It has been established that SWAP exhibits greater SF than that of WW perimetry15,18,32; however, these studies have been based upon double determinations of staircase estimations of threshold. This study found FOS slope in clinically normal subjects to be approximately 38% and 53% flatter for SW than WW perimetry at 4.24° and 9.90°, respectively. Previous studies have tended to underestimate the magnitude of threshold variability for SWAP.15,18,32 This underestimation may be attributed to the staircase estimation of threshold that in turn is used to estimate SF.
For the clinically normal group, the group mean COR for sensitivity was found to be greater for the more eccentric locations and for SW perimetry, indicating greater variability. The magnitude of COR for slope was found to be higher than group mean slope for SW perimetry—that is, the magnitude of variation of the measurement was found to be higher than magnitude of the measurement itself. The absolute sensitivity value was lower for SW automated perimetry parameters. For WW, the magnitude of the COR for slope was found to be lower than the group mean slope.
For WW perimetry, decrease in sensitivity is accompanied by a flattening of the slope of the FOS function20 and glaucomatous patients show enhanced variability when compared to clinically normal subjects.33 For the clinically normal group, the FOS slopes for both stimulus conditions were significantly flatter at 9.90°, while sensitivity was significantly higher at 4.24°. For the patients with diabetes, the results demonstrated that the slope of the SW FOS function was significantly flatter in locations within focal sensitivity loss. Consideration of all the SW data in terms of a plot of sensitivity versus FOS slope clearly showed a curvilinear relation, with slope becoming flatter in locations of lower sensitivity.
In summary, the results of this study confirm that the clinical utility of SWAP will be limited by an increased magnitude of threshold variability compared to that of WW automated perimetry. Despite evidence that SWAP improves the detection of early visual field loss, its utility as a routine clinical tool needs to be treated with caution as a result of exaggerated threshold variability.
Acknowledgments
This study was funded, in part, by a Wellcome Trust Summer Scholarship (awarded to EG) and also a Canadian Institutes of Health Research Operating grant (awarded to CH).
Abbreviations
COR, coefficient of repeatability
FOS, frequency of seeing
SF, short term fluctuation
SW, short wavelength
SWAP, short wavelength automated perimetry
VA, visual acuity
WW, white on white
Ethical approval: The study was approved by the research ethics board of the University Health Network, Toronto. Informed consent was obtained form each subject after explanation of the nature and possible consequences of the study according to the tenets of the Declaration of Helsinki.
REFERENCES
- 1.Demirel S, Johnson CA. Incidence and prevalence of short wavelength perimetry deficits in ocular hypertensive patients. Am J Ophthalmol 2001;131:708–15. [DOI] [PubMed] [Google Scholar]
- 2.Girkin CA, Emdadi A, Sample PA, et al. Short-wavelength automated perimetry and standard perimetry in the detection of progressive optic disc cupping. Arch Ophthalmol 2000;118:1231–6. [DOI] [PubMed] [Google Scholar]
- 3.Johnson CA. Psychophysical measurement of glaucomatous damage. Surv Ophthalmol 2001;45:S313–17. [DOI] [PubMed] [Google Scholar]
- 4.Casson EJ, Johnson JA, Shapiro LR. Longitudinal comparison of temporal-modulation perimetry with white-on-white and blue-on-yellow perimetry in ocular hypertension and early glaucoma. J Opt Soc A 1993;10:1792–806. [DOI] [PubMed] [Google Scholar]
- 5.Johnson CA. Selective versus nonselective losses in glaucoma. J Glaucoma 1994;3 (suppl) :522–44. [PubMed] [Google Scholar]
- 6.Johnson CA, Adams AJ, Casson EJ, et al. Progression of early glaucomatous visual field loss as detected by blue-on-yellow and standard white-on-white automated perimetry. Arch Ophthalmol 1993;111:651–6. [DOI] [PubMed] [Google Scholar]
- 7.Sample PA, Weinreb RN. Progressive color visual field loss in glaucoma. Invest Ophthalmol Vis Sci 1992;33:2068–71. [PubMed] [Google Scholar]
- 8.Bayer AU, Erb C. Short wavelength automated perimetry, frequency doubling technology perimetry, and pattern electroretinography for prediction of progressive glaucomatous standard visual field defects. Ophthalmology 2002;109:1009–17. [DOI] [PubMed] [Google Scholar]
- 9.Hudson C, Flanagan JG, Turner GS, et al. Short-wavelength sensitive visual field loss in patients with clinically significant diabetic macular oedema. Diabetologia 1998;41:918–28. [DOI] [PubMed] [Google Scholar]
- 10.McCreesh BM, Hudson C, Silvestri G, et al. Relative operating characteristic diagnostic test performance of conventional and short-wavelength automated perimetry for patients with clinically significant diabetic macular oedema. Annual Meeting of the Association for Research in Vision and Ophthalmology, 30 April–5 May, Fort Lauderdale, FL, USA. Invest Ophthalmol Vis Sci 2000;41 (Suppl) :654. [Google Scholar]
- 11.Hudson C, McCreesh BM, Quinn MJ, et al. Diabetic macular edema: A comparison of scanning laser derived topographic edema maps and short-wavelength automated perimetry to detect progression. Annual Meeting of the Association for Research in Vision and Ophthalmology 2001; 29 April-4 May, Fort Lauderdale, FL, USA.
- 12.Remky A, Weber A, Hendricks S, et al. Short-wavelength automated perimetry in patients with diabetes mellitus without macular edema. Graefes Arch Clin Exp Ophthalmol 2003;241:468–71 Epub 17 May 2003. [DOI] [PubMed] [Google Scholar]
- 13.Remky A, Arend O, Hendricks S. Short-wavelength automated perimetry and capillary density in early diabetic maculopathy. Invest Ophthalmol Vis Sci 2000;41:274–81. [PubMed] [Google Scholar]
- 14.Nomura R, Terasaki H, Hirose H, et al. Blue-on-yellow perimetry to evaluate S cone sensitivity in diabetics. Ophthalmic Res 2000;32:69–72. [DOI] [PubMed] [Google Scholar]
- 15.Wild JM, Moss ID, Whitaker D, et al. The statistical interpretation of blue-on-yellow visual field loss. Invest Ophthalmol Vis Sci 1995;36:1398–410. [PubMed] [Google Scholar]
- 16.Hutchings N, Hosking SL, Wild JM, et al. Long-term fluctuation in short-wavelength automated perimetry in glaucoma suspects and glaucoma patients. Invest Ophthalmol Vis Sci 2001;42:2332–7. [PubMed] [Google Scholar]
- 17.Wild JM. Short wavelength automated perimetry. Acta Ophthalmol Scand 2001;79:546–59. [DOI] [PubMed] [Google Scholar]
- 18.Kwon YH, Park HJ, Jap A, et al. Test-retest variability of blue-on-yellow perimetry is greater thanwhite-on-white perimetry in normal subjects. Am J Ophthalmol 1998;126:29–36. [DOI] [PubMed] [Google Scholar]
- 19.Blumenthal EZ, Sample PA, Zangwill L, et al. Comparison of long-term variability for standard and short-wavelength automated perimetry in stable glaucoma patients. Am J Ophthalmol 2000;129:309–13. [DOI] [PubMed] [Google Scholar]
- 20.Weber J, Rau S. The properties of perimetric thresholds in normal and glaucomatous eyes. Ger J Ophthalmol 1992;1:79–85. [PubMed] [Google Scholar]
- 21.Flammer J, Drance SM, Zulauf M. Differential light threshold short and long-term fluctuation in patients with glaucoma, normal controls, and patients with suspected glaucoma. Arch Ophthalmol 1984;102:704–6. [DOI] [PubMed] [Google Scholar]
- 22.Westcott MC, Fitzke FW, Crabb DP, et al. Characteristics of frequency-of-seeing curves for a motion stimulus in glaucoma eyes, glaucoma suspect eyes, and normal eyes. Vis Res 1999;39:631–9. [DOI] [PubMed] [Google Scholar]
- 23.Olsson J, Heijl A, Bengtsson B, et al. Frequency-of-seeing in computerized perimetry. In: Mills, ed. Perimetry update 1992/93. Amsterdam: Kugler Publications, 1993:551–6.
- 24.Henson DB, Evans J, Chauhan BC, et al. Influence of fixation accuracy on threshold variability in patients with open angle glaucoma. Invest Ophthalmol Vis Sci 1996;37:444–50. [PubMed] [Google Scholar]
- 25.Wall M, Maw RJ, Stanek KE, et al. The psychometric function and reaction times of automated perimetry in normal and abnormal areas of the visual field in patients with glaucoma. Invest Ophthalmol Vis Sci 1996;37:878–85. [PubMed] [Google Scholar]
- 26.Chylack LT Jr, Wolfe JK, Singer DM, et al. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol 1993;111:831–6. [DOI] [PubMed] [Google Scholar]
- 27.Heijl A, Bengtsson B. The effect of perimetric experience in patients with glaucoma. Arch Ophthalmol 1996;114:19–22. [DOI] [PubMed] [Google Scholar]
- 28.Hudson C, Wild JM, O’Neill EC. Fatigue effects during a single session of automated static threshold perimetry. Invest Ophthalmol Vis Sci 1994;35:268–80. [PubMed] [Google Scholar]
- 29.Sample PA, Johnson CA, Haegerstrom-Portnoy G, et al. Optimum parameters for short-wavelength automated perimetry. J Glaucoma 1996;5:375–83. [PubMed] [Google Scholar]
- 30.Felius J, Swanson WH. Effects of cone adaptation on variability in S-cone increment thresholds. Invest Ophthalmol Vis Sci 2003;44:4140–6. [DOI] [PubMed] [Google Scholar]
- 31.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10. [PubMed] [Google Scholar]
- 32.Sample PA, Cook JN, Weinreb RN. Variability and sensitivity of short-wavelength color visual fields in normal and glaucoma eyes. In: Digest of Topical Meeting on Noninvasive Assessment of the Visual System. Washington, DC: Technical Digest, 1993:292–95.
- 33.Chauhan BC, Tompkins JD, Le Blanc RP, et al. Characteristics of frequency-of-seeing curves in normal subjects, patients with suspected glaucoma, and patients with glaucoma. Invest Ophthalmol Vis Sci 1993;34:3534–40. [PubMed] [Google Scholar]