Pneumosinus dilatans (PSD) is abnormal dilatation of paranasal sinuses that may occasionally present with visual symptoms. We present a case of PSD associated with sickle cell trait which occurred with visual deterioration.
Case report
A 13 year old female presented with gradual painless decrease of vision in both eyes for 1.5 years. Over this period her visual acuity dropped from 20/30 (RE) and 20/160 (LE) to hand motion in both eyes. Except for optic atrophy in both eyes, other ocular examinations were normal. In the visual field there was diffuse peripheral field loss and generalised depression. Past medical history was insignificant except for an appendectomy 5 years earlier.
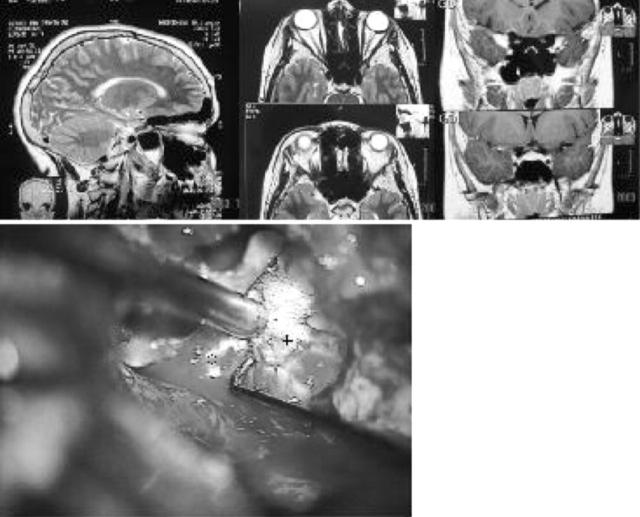
An increased level of sickle cell haemoglobin which constituted 24.9% of her total haemoglobin was documented. Her HbA2 and HbF were in the normal range. She had anaemia with haemoglobin level of 9 g/dl, which we could not find any reason for. Significant expansion of paranasal sinuses including maxillary, frontal, ethmoidal, and sphenoid sinus was visible on magnetic resonance images (MRI) of the patient as shown in figure 1. Based on the MRI of the patient, the diagnosis of PSD would be appropriate.
Figure 1.
(Top) Magnetic resonance images show significant dilatation of paranasal sinuses. (Bottom) Surgical field image. “O” is intracranial part of optic nerve, “+” is the bony canal after partial removal; the metal instrument is a suction device tip.
Bilateral consecutive frontal craniotomy was performed in order to unroof the optic canal with the hope to release stretching of the optic nerve which we thought was the reason for her visual deterioration. Figure 1 (bottom) is an image of the surgical procedure. It is clear that the optic nerves have been entrapped in the bony canal and probably suffered from severe stretching and/or compressive effects. Six months after the procedure her visual acuity was 20/1200 in both eyes.
Comment
Pneumosinus dilatans is an abnormal dilatation of one or more of the paranasal sinuses. It has diverse manifestations including progressive visual loss if the sphenoid sinus is involved and/or if it is associated with optic nerve meningioma. If the ethmoidal sinus is involved it may present with proptosis.1 Although a valve mechanism raising the pressure inside the sinus is thought to be responsible for this condition,2 the exact etiology is unknown.3 In case of optic nerve damage the nerve is usually compressed in long bony tubes.4 Pneumosinus dilatans has been associated with meningioma of the intracanalicular optic nerve and anterior chiasmal angle,5,6 middle cranial fossa arachnoid cyst,7 cerebral hemiatrophy, and prolonged cerebrospinal fluid shunting.8
To our knowledge this is the first case of PSD associated with sickle cell trait. PSD has not been associated previously with haematological disorders. Considering the fact that sickle cell trait is generally an asymptomatic condition and the patient’s mother was also an asymptomatic carrier, an aetiological relation is unproved. On the other hand, both conditions are rare in our population, therefore the probability of coincidence by chance would seem to be extremely low. The question remains whether our patient had an unusual form of sickle cell trait associated with gross bony involvement and deformity.
Different treatments have been proposed for PSD. These include subtotal resection of the medial wall of the maxillary sinus by an endoscopic approach,9 osteotomy of the deformed fronto-orbital bossing, and obliteration of the sinus with fat.10 Because of global and massive expansion of the sinuses and severe optic nerve dysfunction in this case, we preferred to decompress the optic nerve by removing the roof of bony canal which surrounded the intracranial optic nerve. This resulted in mild visual improvement.
References
- 1.Skolnick CA, Mafee MF, Goodwin JA. Pneumosinus dilatans of the sphenoid sinus presenting with visual loss. J Neuro-ophthalmol 2000;20:259–63. [PubMed] [Google Scholar]
- 2.Wolfensberger M. Pathogenesis of pneumosinus maxillaris dilatans. HNO 1984;32:518–20. [PubMed] [Google Scholar]
- 3.Walker JL, Jones NS. Pneumosinus dilatans of the frontal sinuses: two cases and a discussion of its aetiology. J Laryngol Otol 2002;116:382–5. [DOI] [PubMed] [Google Scholar]
- 4.Stretch JR, Poole MD. Pneumosinus dilatans as the aetiology of progressive bilateral blindness. Br J Plast Surg 1992;45:469–73. [DOI] [PubMed] [Google Scholar]
- 5.Hirst LW, Miller NR, Hodges FJ 3rd, et al. phenoid pneumosinus dilatans. A sign of meningioma originating in the optic canal. Neuroradiology 1982;22:207–10. [DOI] [PubMed] [Google Scholar]
- 6.Mai A, Karis J, Sivakumar K. Meningioma with pneumosinus dilatans. Neurology 2003;60:1861. [DOI] [PubMed] [Google Scholar]
- 7.Redla S, Husami Y, Colquhoun IR. Apparent paradoxical vault changes with middle cranial fossa arachnoid cysts—implication for aetiology. Clin Radiol 2001;56:851–5. [DOI] [PubMed] [Google Scholar]
- 8.Van Schayck R, Niedeggen A. Pneumosinus dilatans after prolonged cerebrospinal fluid shunting in young adults with cerebral hemiatrophy. A report of two cases and review of the literature. Neurosurg Rev 1992;15:217–23. [DOI] [PubMed] [Google Scholar]
- 9.Juhl HJ, Buchwald C, Bollinger B. An extensive maxillary pneumosinus dilatans. Rhinology 2001;39:236–8. [PubMed] [Google Scholar]
- 10.Tellado MG, Mendez R, Lopez-Cedrun JL, et al. Pneumosinus dilatans of the frontal and ethmoidal sinuses: case report. J Craniomaxillofac Surg 2002;30:62–4. [DOI] [PubMed] [Google Scholar]