Community optometrists in the United Kingdom carry out 17.2 million primary eyecare examinations per annum,1 which result in at least 0.5 million referrals to the hospital eye service.2,3 Optometrists only infrequently receive a reply to these referrals,4,5 possibly because 69% are handwritten on GOS18 forms,6 which can lack legibility6 and details.5 Most optometrist initiated referrals take place via general practitioners (GPs), who are increasingly likely to forward the optometrist’s letter.6 We improved our referrals and audited the replies.
Methods
The Institute of Optometry set minimum criteria for referrals in 2004 by typing letters on headed notepaper, including the practitioner’s name, enclosing a second copy for the GP to forward to the ophthalmologist, and including text which explicitly requested a reply.
In February–April 2005 we audited referrals from 2004. Handwritten emergency referrals, which make up less than 1% of referrals, were not included.
Results
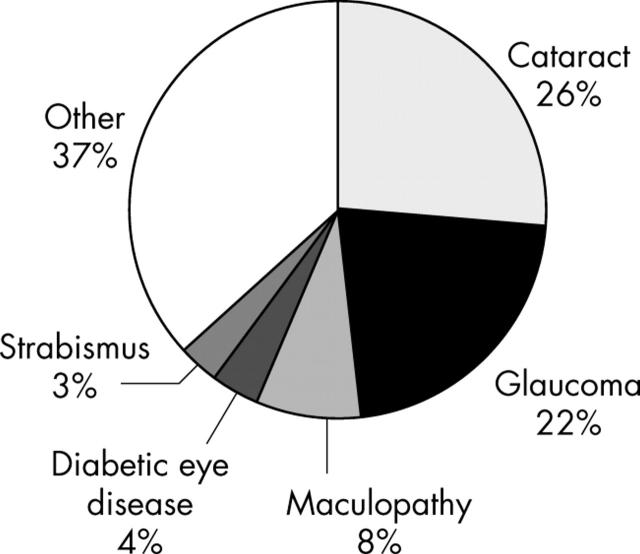
There were 181 referrals following 7164 eye examinations, 51% were female, and the reasons for referral are given in figure 1. The provisional diagnoses for the “other” category include a wide range of conditions, all with a prevalence of less than 3%.
Figure 1.
Reasons for referral.
A reply was requested in 95% of letters, but was received for only 23 (13%). There was no relation between the likelihood of reply and the reason for referral (p = 0.37).
Comment
The institute’s referral rate (2.5%) is lower than previously reported for optometrists.2,3 This might reflect better facilities for monitoring (for example, ocular hypertension) or managing (for example, dry eye) conditions and an ethos that encourages management when appropriate.
Although our results are only for one centre it is disappointing that, despite taking steps to encourage a reply, this is still rarely forthcoming. The proportion of referrals that receive replies is so low (13%) that we think it unlikely to be attributable to patients failing to consult the GP or ophthalmologist after referral. For the few ophthalmologists who do reply this is not an onerous task: they instruct their secretary to copy the reply to the GP to the optometrist. The NHS code of practice on confidentiality notes that explicit consent is not usually required for information disclosures that support the delivery of the patient’s care.7 Even if it is thought necessary to obtain consent, there is no good reason why the ophthalmologist should not obtain this.4 The issue of consent does not seem to be the main reason for lack of replies: a study found that ophthalmologists actually replied to a higher proportion of referrals when the optometrists had not obtained consent than when they had.4
Replying to referrals helps optometrists provide continuing patient care and avoids possible errors from the optometrist relying on the patient’s recollection of the ophthalmologist’s findings. Feedback also contributes to optometrists’ professional development and helps to ensure that inappropriate referrals are minimised in the future.8
Now that direct referral from primary care optometrists to secondary care ophthalmology units is becoming more commonplace,9 we hope that a two way flow of information will become the norm.
References
- 1.Department of Health. Sight tests volume and workforce survey 2003–2004. www.dh.gov.uk/assetRoot/04/08/65/64/04086564.pdf 2004, accessed 11 April 2005.
- 2.Hobley AJ, Woodward EG, Port MJ. Retrospective study of optometric referrals. Ophthalmic Physiol Opt 1992;12:395–9. [PubMed] [Google Scholar]
- 3.Port MJ. Referrals and notifications by optometrists within the UK: 1988 survey. Ophthalmic Physiol Opt 1989;9:31–5. [DOI] [PubMed] [Google Scholar]
- 4.Whittaker KW, Ikram K, Anderson DF, et al. Non-communication between ophthalmologists and optometrists. J R Soc Med 1999;92:247–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lash SC. Assessment of information included on the GOS 18 referral form used by optometrists. Ophthalmic Physiol Opt 2003;23:21–3. [DOI] [PubMed] [Google Scholar]
- 6.Pooley JE, Frost EC. Optometrists’ referrals to the hospital eye service. Ophthal Physiol Opt 1999;19:S16–S24. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health. Confidentiality: NHS Code of Practice. www.publications.doh.gov.uk/ipu/confiden/protect/copv3.pdf 2003, accessed 11 April 2005.
- 8.Ingram DV, Culham LE. Ophthalmologists and optometrists—interesting times? Br J Ophthalmol 2001;85:769–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Department of Health. Delivering quality in primary care: General ophthalmic service practitioners. www.dh.gov.uk/assetRoot/04/10/60/33/04106033.pdf 2005, accessed 11 April 2005.