Abstract
Background and aims: Over the past two decades in Taiwan, pyogenic liver abscess has usually been caused by a single microorganism, Klebsiella pneumoniae, and is frequently associated with the serious complication of endophthalmitis, especially in diabetic patients. However, the relationship between the clinical presentation and bacterial factors remains unclear. The aim of this study was to investigate the clinical features of patients and the serotype and ribotype of K pneumoniae liver abscess.
Methods: From July 1991 to June 1998, a total of 134 cases of K pneumoniae liver abscess with 248 K pneumoniae isolates from the same patients were collected from two large medical centres in northern Taiwan. Clinical data were collected from medical records. Serotyping and ribotyping were performed using the countercurrent immunoelectrophoresis method and automated Riboprinter.
Results: Serotyping revealed that the most common serotypes were K1 (63.4%) and K2 (14.2%). K1 isolates occurred at a significantly higher frequency (p<0.01) than all other serotypes. Among 134 patients, 105 (78.4%) had suffered from diabetes mellitus for 3–15 years. Fourteen patients (10.4%) had metastatic infection to the eye causing septic endophthalmitis. Liver aspirates, and blood and vitreous pus cultures yielded the same serotype of K pneumoniae in all patients. Among patients with septic endophthalmitis, 92.3% (13/14) were diabetic, and 85.7% (12/14) of the isolates belonged to serotype K1. For molecular typing, different degrees of genetic polymorphism among isolates with the same K1 serotype suggested no particular prevalence of any one strain in K pneumoniae liver abscess.
Conclusion: K pneumoniae serotype K1 was significantly associated with liver abscess and the complication of endophthalmitis, especially in diabetic patients. Physicians should request an immediate report of serotyping and susceptibility test results simultaneously if a diagnosis of pyogenic liver abscess has been made so that early and appropriate management for possible complications will not be delayed. The use of ceftriaxone because of its higher concentration in the aqueous humor is suggested to decrease the chance of septic endophthalmitis.
Keywords: Klebsiella pneumoniae, liver abscess, serotype K1
Pyogenic liver abscess is usually a polymicrobial infection that has ascended from the gastrointestinal tract. In Western countries, the most frequent aetiological agents of pyogenic liver abscess were Escherichia coli, streptococci, and anaerobic bacteria.1–3 However, over the past two decades in Taiwan, liver abscess has usually been caused by a single microorganism, Klebsiella pneumoniae, presenting in 50–88% of pyogenic liver abscesses.4, 5 Approximately 3–7.8% of cases involving this organism have distant metastases to the eye via the bloodstream causing septic endophthalmitis.4, 6, 7 An extremely poor visual outcome seems unavoidable in septic K pneumoniae endophthalmitis despite aggressive treatment. Many victims develop permanent loss of visual acuity despite systemic and intravitreal therapy, and several cases requiring vitrectomy or enucleation of the affected eye for removal of the infectious focus have been reported.8–10 Previous studies from Taiwan demonstrated that diabetes mellitus is the most common underlying condition, with a prevalence ranging from 45% to 75% in patients with K pneumoniae liver abscess.4, 5, 11, 12 The same findings were found in recent reports from Trinidad, the USA, and Singapore.13–15 Furthermore, metastatic septic endophthalmitis complicating pyogenic liver abscess caused by K pneumoniae in diabetic patients has also been reported in Australia, Granada, and the USA.16–18 The relationship of this condition to race or environment, as well as its pathogenesis, remains uncertain. It is undoubtedly becoming a global problem rather than being confined to Taiwan.
In this study we evaluated the frequency of capsular serotypes and ribotypes among 134 Taiwanese patients with K pneumoniae liver abscess using K pneumoniae isolates from different sites on the same patient, and compared the epidemiological features and underlying diseases in these patients.
MATERIALS AND METHODS
Case definition
Consecutive patients with K pneumoniae liver abscess were enrolled in the study if computed tomographic (CT) scanning revealed one or more space occupying lesions, or ultrasonography showed one or more areas of echolucency in the liver and a culture of CT guided or ultrasonic guided percutaneous liver aspirates revealed K pneumoniae. Patients with a positive blood culture for K pneumoniae but lacking tissue culture (for example, liver aspirates or eye aspirates) were excluded. Diabetes mellitus was defined as a fasting blood glucose level >140 mg/dl, a random plasma glucose level >200 mg/dl, or a previous diagnosis of diabetes mellitus in a patient receiving oral hypoglycaemic agents or insulin therapy. Other underlying diseases and clinical data were collected from the medical records.
Bacterial isolates
Clinical isolates of K pneumoniae from liver aspirates, blood, vitreous aspirates, or other sterile body areas from patients with a diagnosis of K pneumoniae liver abscess were identified in the hospital clinical microbiology laboratory using the API 20E system (Bio-Merieux, Marcy I'Etoile, France). Liver isolates, blood, and other isolates from sterile body areas were accepted only once during each episode of infection from the same patient. All isolates were stored in brain-heart infusion broth at −70° C until used.
Antimicrobial susceptibility testing
Susceptibility to antimicrobial agents was studied using the disc diffusion method on Mueller-Hinton agar medium (BBL Microbiological System, Cockeysville, Maryland, USA). The antibiotics tested were ampicillin (10 μg), carbenicillin (100 μg), cefazolin (30 μg), cefonicid (30 μg), cefotaxime (30 μg), ceftriaxone (30 μg), cefoperazone (75 μg), ceftazidime (30 μg), gentamicin (10 μg), and amikacin (30 μg). All antibiotic containing discs were purchased from Becton Dickinson (BBL Microbiological System). Interpretations were performed according to the guidelines of the National Committee for Clinical Laboratory Standards.19
Serotyping
All isolates were serotyped by a countercurrent immunoelectrophoresis method.20 Antisera were kindly provided by the Laboratory of Hospital Infection, Central Public Health Laboratory (CPHL), London. K pneumoniae ATCC9997 (K2) was used as a control strain.
Ribotyping
To study whether the K pneumoniae isolated from liver abscess patients was caused by the spreading of a single strain, ribotying was used because of its high discriminatory power. Ribotyping was performed using the automated Riboprinter microbial characterisation system (Qualicon, Wilmington, Delaware, USA) according to the manufacturer's instructions. Colonies were picked and loaded into the Riboprinter microbial characterisation unit (MCU). Within the MCU, total DNA was digested with EcoRI enzyme, separated by electrophoresis, and transferred directly to nylon membranes. Ribopatterns were expressed by hybridisation with a chemiluminescence labelled DNA probe containing an rRNA operon (rrnB) from E coli. The patterns were automatically imaged and stored in the MCU computer. The positions of standard markers were used to correct for both lane to lane and membrane to membrane variations in band position. The ribopattern for each isolate was compared with other patterns in the Riboprinter database. Assignment to a particular ribogroup was based on differences in band numbers, band position, and signal intensity at a given banding position.21
Statistical analysis
Statistical analysis was performed using the χ2 test with Yates' correction; p<0.05 was considered to be statistically significant.
RESULTS
Patients and bacterial culture
From July 1991 to June 1998, a total of 134 patients with K pneumoniae liver abscess were treated in Taipei Veterans General Hospital or Tri-Service General Hospital, and 248 K pneumoniae isolates from different sites of infection in these patients were collected from the clinical microbiology laboratories of these hospitals. All cases were community acquired. The male to female ratio was 3.06 (101:33). Mean age was 56.4 years. Of the 248 K pneumoniae isolates, 134 were obtained from liver aspirates, 96 from blood cultures, 14 from vitreous pus cultures, two from cerebrospinal fluid, one from knee joint fluid, and one from a lung abscess. Generally, cultures of blood and liver aspirates were performed in the emergency room on the first day when liver abscess was diagnosed, and vitreous pus cultures were performed on the ward when the ocular symptoms appeared and endophthalmitis was suspected by an ophthalmologist, usually within 48–72 hours after the pyogenic liver abscess had been diagnosed (table 1 ▶).
Table 1.
Properties of patients and bacteria studied
| Patients | |
| Duration | 1/7/1991–1/6/1998 |
| Cases | 134 |
| M/F ratio | 3.06/1 |
| Age (y) | |
| Range | 34–78 |
| Mean | 56.4 |
| Bacterial culture | |
| No of culture | |
| Liver aspirates | 134 |
| Blood | 96 |
| Eye | 14 |
| CSF | 2 |
| Knee joint fluid | 1 |
| Lung abscess | 1 |
| Location of specimen collection | |
| Liver aspirates and blood | Emergency room |
| Vitreous pus | 48–72 h after admission |
CSF, cerebrospinal fluid
Comparison of the serotype of K pneumoniae with underlying conditions
Seroepidemiological study in this series identified a total of 14 of the 77 known capsular serotypes. Approximately 98.5% of the strains were typeable. Serotypes K1 and K2 were predominant, accounting for 63.4% and 14.2% of all isolates, respectively. K1 isolates occurred at a significantly higher frequency than all other serotypes (p<0.01). The serotypes of isolates from different specimens in the same patients were uniformly identical.
Diabetes mellitus was the most common underlying disease and was present in 78.4% (105/134) of patients. Most of these patients (102) had suffered from diabetes mellitus for 3–15 years and had used oral hypoglycaemic agents or insulin therapy during this period. The most common serotype of K pneumoniae isolated from diabetic patients was K1 (78 isolates), followed by K2 (14 isolates), K16 (three isolates), K21 (two isolates), K28 (two isolates), and K29, K38, K54, and K57 (one isolate each). Interestingly, serotype K1 was not found in any patient with the following underlying diseases: gall stones, biliary tract stones, or cirrhosis of the liver. K2 was the predominant type for these conditions (table 2 ▶).
Table 2.
Serotype of Klebsiella pneumoniae liver abscess in relation to underlying diseases (n=134)
| Underlying disease* | No of cases (%) | Serotype distribution of isolates (n) |
| Diabetis mellitus | 105 (78.4) | K1 (78), K2 (14), K5 (2), K16 (3), K21 (2), K28 (2), K29 (1), K38 (1), K54 (1), K57 (1) |
| Cholelithiasis | 11 (8.2) | K2 (8), K21 (2), K57 (1) |
| Neoplasms† | 7 (5.2) | K1 (4), K2 (2), K68 (1) |
| Steroid or chemotherapy | 2 (1.5) | K1 (1), K2 (1) |
| Cirrhosis of the liver | 2 (1.5) | K2 (2) |
*Some patients had more than one underlying disease.
†Hepatoma three; colon cancer two; gall bladder cancer one; and breast cancer one.
Relation of K pneumoniae serotype to diabetes and the incidence of bacteraemia, septic endophthalmitis, and other distal site metastases
Ninety six patients (71.6%) with K pneumoniae liver abscess had a positive blood culture for K pneumoniae. Only serotypes K1 and K2 were found in patients with septic endophthalmitis, in particular K1 which was found in 85.7% of all septic endophthalmitis cases (12/14). Of the 14 patients with septic endophthalmitis, 13 (93%) had a past history of diabetes mellitus (table 3 ▶).
Table 3.
Occurrence of Klebseiella pneumoniae liver abscess with septic endophthalmitis between 1991 and 1998
| Serotype (K) | No of cases | No with diabetes mellitus (%) | No with bacteraemia (%) | No with septic endophthalmitis (%) | No with other site metastasis (%) |
| K1 | 85 | 78 (91.8) | 72 (84.7) | 12 (14.1) | 3 (3.5) |
| K2 | 19 | 14 (73.7) | 11 (57.9) | 2 (10.5) | 1 (5.3) |
| K16 | 6 | 3 | 3 | 0 | 0 |
| K21 | 4 | 2 | 1 | 0 | 0 |
| K28 | 4 | 2 | 2 | 0 | 0 |
| K54 | 3 | 1 | 2 | 0 | 0 |
| K5 | 2 | 2 | 2 | 0 | 0 |
| K29 | 2 | 1 | 1 | 0 | 0 |
| K38 | 2 | 1 | 0 | 0 | 0 |
| K39 | 2 | 0 | 0 | 0 | 0 |
| K57 | 2 | 1 | 1 | 0 | 0 |
| K68 | 1 | 0 | 0 | 0 | 0 |
| NT | 2 | 0 | 0 | 0 | 0 |
| Total | 134 | 105 (78.3) | 96 (71.6 ) | 14 (10.4) | 4 (3.0) |
NT, not typeable.
Antimicrobial susceptibility pattern and clinical features during treatment
The antimicrobial susceptibility pattern was the same in all 248 K pneumoniae isolates, with uniform resistance to ampicillin and carbenicillin and susceptibility to all cephalosporins and aminoglycosides. Patients without complications received standard treatments including pigtail catheter drainage and parenteral cefazolin plus gentamicin for two weeks, followed by cefazolin treatment for 2–3 weeks and oral cephalosporin for 2–3 months to prevent relapse. In patients with septic endophthalmitis or other distal metastases, the regimen was shifted to a third generation cephalosporin—for example, ceftriaxone—or ceftazidime. The mortality rate of patients with liver abscess was low (5.2%, 7/134). All patients with primary liver abscess survived except for four patients with septic endophthalmitis (two of whom had meningitis), two with an underlying disease of hepatoma, and one with lung abscess. Among the 10 patients with endophthalmitis who survived, only two had recovered completely from early treatment with ceftriaxone. The other patients had extremely poor visual acuity or total blindness of the affected eyes.
Molecular epidemiology
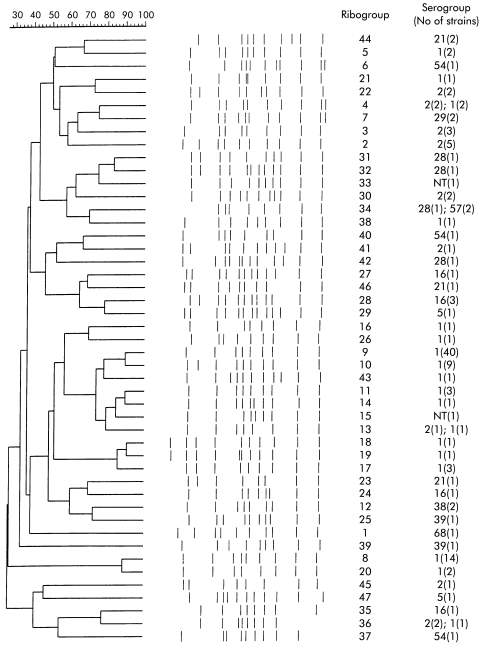
Automated ribotyping identified 47 different ribotype profiles. A high degree of genetic polymorphism between the serogroups and ribotypes was observed. Sixty three of 85 isolates (74.1%) in serotype K1 belonged to ribotypes 8, 9, and 10. Ribotype 9 was identified in 40 of 85 (47.1%) seotype K1 isolates. Among the 47 ribotypes identified, most ribotypes were specific to particular serotypes except for ribotypes 2, 3, 4, 12, 30, 34, and 36 (fig 1 ▶). No clonal spreading of a particular serotype responsible for liver abscess was observed based on the results of ribotyping.
Figure 1.
Ribotypes and genetical linkage calculated by the unweighted pair group method using arithmetic averages (UPGMA) among 134 Klebsiella pneumoniae isolates. NT, non-typeable.
DISCUSSION
Research on the pathogenesis of experimental infections with K pneumoniae has shown capsular polysaccharide (CPS, K antigen) to be a prime factor in the microorganism's virulence. Animal studies have shown that K pneumoniae isolates belonging to serotypes K1 and K2 are the most virulent when injected intraperitoneally.22, 23 However, there have been no data from human studies to show that serotypes K1 and K2 are the most virulent types. In this study, K pneumoniae liver abscess caused by K1 and K2 comprised 78% of the total isolates, which was significantly higher than for the other serotypes identified (p<0.001). We previously reported a 21.7% prevalence of K1 in 1000 patients with non-selected K pneumoniae.24 According to these data, the incidence of K1 serotype in liver abscess patients in the present series was significantly higher than in patients from the same population with non-selected K pneumoniae infections (χ2; p<0.001). Thus a relatively high prevalence of K1 in the community could not be the sole explanation for the greater than 63% prevalence of K1 liver abscess in the present study. In patients with septic endophthalmitis, 85.7% (12/14) of K pneumoniae isolates from vitreous pus belonged to serotype K1 and 14.3% to serotype K2; all of the involved organisms could be detected from liver aspirates and blood simultaneously. In addition, isolates from the eye were detected when ocular symptoms appeared, usually 48–72 hours after pyogenic liver abscess had been diagnosed. This suggests that all of the septic endophthalmitis cases from K pneumoniae liver abscess developed by ascending via the bloodstream. Also, the development of severe complications could be a consequence of late drainage. Further investigation of the consequences of late drainage of liver abscess in patients with complicated septic endophthalmitis is warranted. This study also provided evidence that K1 and K2 strains, which are known to be the most virulent strains in animals, may also be the most virulent in humans.
It has been shown that certain CPS types could prompt the binding of K pneumoniae to guinea pig alveolar macrophages in serum free media followed by ingestion and killing of the bacteria. The molecular basis for this type of phagocytosis, termed lectinophagocytosis,25, 26 is involved in the macrophage mannose receptor, which recognises sequences such as mannose-α2/3-mannose and L-rhamnose-α2/3-rhamnose found in the CPS of a number of capsular serotypes. Bacteria with a cps gene which lack such sequences that interact with a macrophage lectin could display high resistance to phagocytosis.27 An intriguing finding is that K1 and K2 specifically lack mannose-α2/3-mannose and L-rhamnose-α2/3-rhamnose.25 This finding is in line with the results of the present study that K1 and K2 were the predominant serotypes of K pneumoniae in pyogenic liver abscess, suggesting that they have a more invasive capsular antigen. As for K pneumoniae liver abscess, no previous report has focused on this possible pathogenic mechanism. However, demonstration that blood clearance of the bacteria is mainly due to sequestration of the bacteria into the liver and spleen, which contain macrophages (Kupffer's cells) that express the mannose receptor, suggests a possible mechanism.28, 29 If Klebsiella strains are not recognised by the macrophage lectin, they will be able to escape from lectinophagocytosis and proliferate, and will then express other virulent factors.
A previous study showed that in a high proportion of patients, liver abscess was caused by a cluster of clonal related K pneumoniae.30 Among 134 isolates in the present study, 47 ribotypes were identified. Although a high proportion (40/85; 46.0%) of K1 were observed in ribotype 9 in the present study, ribotyping provided no evidence to suggest that clonal spread of a strain was a cause of disease due to the finding of different degrees of genetic polymorphism. However, the predominance of serotypes K1 and K2 in pyogenic liver abscess suggests that those serotypes have a more invasive capsular antigen. Furthermore, no specific pattern for differentiation of K pneumoniae K1 or K2 isolates from eye aspirates or liver aspirates of diabetic or non-diabetic patients could be detected. Pyogenic liver abscesses caused by K pneumoniae with distant metastasis to the eye resulting in endophthalmitis may be due to the virulent capsule or host factors which could not be found by ribotyping in this study. Further analysis of the cps gene and host factors may provide clues to understanding the pathogenesis of K pneumoniae liver abscess.
In this study, diabetes mellitus was the most common underlying condition associated with 78.4% of cases (105/134). This result is compatible with the findings of previous studies in Taiwan.4, 5, 12 Although diabetes is known to interfere with neutrophil chemotaxis and phagocytosis, its influence on the function of macrophages, including Kupffer's cells, is still unknown. Further study of the phagocytic function of Kupffer's cells may be another approach in the investigation of liver abscess in diabetic patients.
K pneumoniae isolates obtained from patients with liver abscess in this study were susceptible to all antibiotics tested, except for ampicillin and carbenicillin. This observation is consistent with the findings of Wang et al that K pneumoniae which causes liver abscess is community acquired and is not a naturally multiresistant strain.5 In fact, reports of this phenomenon has been consistent for more than 15 years.4, 31, 32 However, it is worth noting that ampicillin and amoxicillin have been widely used for the treatment of respiratory tract infections and urinary tract infections for more than 20 years in Taiwan, where no effective antibiotic control policy has been instituted. Furthermore, a recent study in Taiwan found that over half of all patients admitted to the emergency unit had consumed antibiotics before admission, especially internal medicine outpatients.33 Ampicillin or amoxicillin can be purchased from local drug stores without prescription. Treatment with oral antibiotics changes the ecology of the bowel flora and may lead to overgrowth of already present microorganisms with natural resistance. This may explain why so many cases of K pneumoniae liver abscess arise in the Taiwan population with resistance to ampicillin and carbenicillin and with an especially high prevalence of serotypes K1 and K2.24
Pigtail catheter drainage plus cefazolin and gentamicin parenteral therapy has been the standard treatment for uncomplicated cases. In patients with ocular complications, changing to third generation cephalosporins, especially ceftriaxone, due to their higher concentrations in the human aqueous humor, is recommended.34, 35 Unfortunately, it is generally too late to prevent exacerbation of endophthalmitis if the diagnosis has been delayed. Thus earlier detection of serotype K1 for high risk patients is crucial for the treatment of ocular symptoms, which usually occur 48–72 hours after admission. Since bacterial culture and serotyping for K pneumoniae from liver aspirates require 18 hours, physicians should request an immediate report of serotyping and susceptibility test results simultaneously if the diagnosis of pyogenic liver abscess has been made. If K pneumoniae serotype K1 is identified, prompt reporting of laboratory results is needed to allow modifications to the treatment regimen in order to decrease the chance of developing septic endophthalmitis.
This study demonstrated that cases of pyogenic liver abscess involving serotypes K1 and K2 of K pneumoniae in Taiwan are the most virulent with regard to tissue invasion and dissemination, especially in diabetic patients because of their immunocompromised status with impairment of phagocytic function. Routine serotyping should be promptly reported so that precautions against the development of ocular symptoms can be taken whenever a diabetic patient presents with K pneumoniae liver abscess.
Acknowledgments
This work was supported by grants from Taipei Veterans General Hospital (VGH-88-4) and the National Health Research Institutes, and partly from the National Science Council (NSC89-2314-B-075-031), Taiwan.
Abbreviations
CT, computed tomography
MCU, microbial characterisation unit
CPS, capsular polysaccharide
REFERENCES
- 1.Brook I, Frazier EH. Microbiology of liver and spleen abscesses. J Med Microbiol 1998;47:1075–80. [DOI] [PubMed] [Google Scholar]
- 2.Moore-Gillon JC, Eykyn SJ, Phillips I. Microbiology of pyogenic liver abscess. BMJ (Clin Res Ed) 1981;283:819–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rubin RH, Swartz MN, Malt R. Hepatic abscess. Changes in clinical, bacteriologic and therapeutic aspects. Am J Med 1974;57:601–10. [DOI] [PubMed] [Google Scholar]
- 4.Chang FY, Chou MY. Comparison of pyogenic liver abscesses caused by Klebsiella pneumoniae and non-K. pneumoniae pathogens. J Formos Med Assoc 1995;94:232–7. [PubMed] [Google Scholar]
- 5.Wang JH, Liu YC, Lee SS, et al. Primary liver abscess due to Klebsiella pneumoniae in Taiwan. Clin Infect Dis 1998;26:1434–8. [DOI] [PubMed] [Google Scholar]
- 6.Cheng DL, Liu YC, Yen MY, et al. Septic metastatic lesions of pyogenic liver abscess. Their association with Klebsiella pneumoniae bacteremia in diabetic patients. Arch Intern Med 1991;151:1557–9. [PubMed] [Google Scholar]
- 7.Chou FF, Kou HK. Endogenous endophthalmitis associated with pyogenic hepatic abscess. J Am Coll Surg 1996;182:33–6. [PubMed] [Google Scholar]
- 8.Liao HR, Lee HW, Leu HS, et al. Endogenous Klebsiella pneumoniae endophthalmitis in diabetic patients. Can J Ophthalmol 1992;27:143–7. [PubMed] [Google Scholar]
- 9.Liu YC, Cheng DL, Lin CL. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Intern Med 1986;146:1913–16. [PubMed] [Google Scholar]
- 10.Yarng SS, Hsieh CL, Chen TL. Vitrectomy for endogenous Klebsiella pneumoniae endophthalmitis with massive subretinal abscess. Ophthalmic Surg Lasers 1997;28:147–50. [PubMed] [Google Scholar]
- 11.Chou FF, Sheen-Chen SM, Chen YS, et al. Single and multiple pyogenic liver abscesses: clinical course, etiology, and results of treatment. World J Surg 1997;21:384–8. [DOI] [PubMed] [Google Scholar]
- 12.Yang CC, Chen CY, Lin XZ, et al. Pyogenic liver abscess in Taiwan: emphasis on gas-forming liver abscess in diabetics. Am J Gastroenterol 1993;88:1911–15. [PubMed] [Google Scholar]
- 13.Barton EN, Daisley H, Gilbert DT, et al. Diabetes mellitus and Klebsiella pneumoniae liver abscess in adults. Trop Geogr Med 1991;43:100–4. [PubMed] [Google Scholar]
- 14.Hansen N, Vargish T. Pyogenic hepatic abscess: a case for open drainage. Am Surg 1993;59:219–22. [PubMed] [Google Scholar]
- 15.Yeoh KG, Yap I, Wong ST, et al. Tropical liver abscess. Postgrad Med J 1997;73:89–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lindstrom ST, Healey PR, Chen SC. Metastatic septic endophthalmitis complicating pyogenic liver abscess caused by Klebsiella pneumoniae. Aust N Z J Med 1997;27:77–8. [DOI] [PubMed] [Google Scholar]
- 17.Saccente M. Klebsiella pneumoniae liver abscess, endophthalmitis, and meningitis in a man with newly recognized diabetes mellitus. Clin Infect Dis 1999;29:1570–1. [DOI] [PubMed] [Google Scholar]
- 18.Cobo MF, Aliaga ML, Diaz MF, et al. Liver abscess caused by Klebsiella pneumoniae in diabetic patients. Rev Clin Esp 1999;199:517–19. [PubMed] [Google Scholar]
- 19.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial disk susceptibility tests. Approved standard M2-A6. Villanova, PA: National Committee for Clinical Laboratory Standards, 1997.
- 20.Palfreyman JM. Klebsiella serotyping by counter-current immunoelectrophoresis. J Hyg (Lond) 1978;81:219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brunner S, Fleisch F, Ruef C, et al. Automated ribotyping and pulsed-field gel electrophoresis reveal a cluster of group A streptococci in intravenous drug abusers. Infection 2000;28:314–17. [DOI] [PubMed] [Google Scholar]
- 22.Mizuta K, Ohta M, Mori M, et al. Virulence for mice of Klebsiella strains belonging to the O1 group: relationship to their capsular (K) types. Infect Immun 1983;40:56–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nassif X, Sansonetti PJ. Correlation of the virulence of Klebsiella pneumoniae K1 and K2 with the presence of a plasmid encoding aerobactin. Infect Immun 1986;54:603–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fung CP, Hu BS, Chang FY, et al. A 5-year study of the seroepidemiology of Klebsiella pneumoniae: high prevalence of capsular serotype K1 in Taiwan and implication for vaccine efficacy. J Infect Dis 2000;181:2075–9. [DOI] [PubMed] [Google Scholar]
- 25.Athamna A, Ofek I, Keisari Y, et al. Lectinophagocytosis of encapsulated Klebsiella pneumoniae mediated by surface lectins of guinea pig alveolar macrophages and human monocyte-derived macrophages. Infect Immun 1991;59:1673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ofek I, Sharon N. Lectinophagocytosis: a molecular mechanism of recognition between cell surface sugars and lectins in the phagocytosis of bacteria. Infect Immun 1988;56:539–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ofek I, Kabha K, Athamna A, et al. Genetic exchange of determinants for capsular polysaccharide biosynthesis between Klebsiella pneumoniae strains expressing serotypes K2 and K21a. Infect Immun 1993;61:4208–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ashwell G, Harford J. Carbohydrate-specific receptors of the liver. Annu Rev Biochem 1982;51:531–54. [DOI] [PubMed] [Google Scholar]
- 29.Kabha K, Nissimov L, Athamna A, et al. Relationships among capsular structure, phagocytosis, and mouse virulence in Klebsiella pneumoniae. Infect Immun 1995;63:847–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lau YJ, Hu BS, Wu WL, et al. Identification of a major cluster of Klebsiella pneumoniae isolates from patients with liver abscess in Taiwan. J Clin Microbiol 2000;38:412–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chang FY, Chou MY, Fan RL, et al. A clinical study of Klebsiella liver abscess. J Formos Med Assoc 1988; 87:282–7. [PubMed] [Google Scholar]
- 32.Cheng DL, Liu YC, Yen MY, et al. Causal bacteria of pyogenic liver abscess. J Formos Med Assoc 1989; 88:1008–11. [PubMed] [Google Scholar]
- 33.Liu YC, Huang WK, Huang TS, et al. Extent of antibiotic use in Taiwan shown by antimicrobial activity in urine. Lancet 1999;354:1360. [DOI] [PubMed] [Google Scholar]
- 34.Sharir M, Triester G, Kneer J, et al. The intravitreal penetration of ceftriaxone in man following systemic administration. Invest Ophthalmol Vis Sci 1989; 30:2179–83. [PubMed] [Google Scholar]
- 35.Wang FD, Wang LS, Liu YC, et al. Successful treatment of metastatic endophthalmitis. Ophthalmologica 1989;198:124–8. [DOI] [PubMed] [Google Scholar]