Abstract
Background and aims: Patients suffering from inflammatory bowel disease show increased levels of the mast cell products histamine and tumour necrosis factor α (TNF-α). Treating these patients with antibodies against TNF-α diminishes the symptoms of diarrhoea. In this study, the effect of TNF-α on ion secretion induced by the mast cell mediator histamine in HT29cl.19A cells and mouse distal colon was investigated and the possible second messengers involved were studied.
Methods: Electrophysiology of filter grown HT29cl.19A cells and isolated mouse distal colon was used to monitor the secretory response to histamine with and without prior exposure to TNF-α for 3–24 hours. Phospholipase D (PLD) activity and phosphatidic acid levels were analysed by 32Pi labelling of HT29cl.19A cells.
Results: In both experimental systems TNF-α was found to potentiate ion secretion induced by histamine. Phospholipid analysis of HT29cl.19A cells revealed that histamine activates the PLD pathway. Furthermore, TNF-α pretreated cells were found to have decreased phosphatidic acid levels, the intermediate product of the PLD pathway, which indicates upregulation of the enzyme phosphatidic acid phosphatase.
Conclusions: The mast cell products TNF-α and histamine synergistically stimulate ion secretion in intestinal epithelium via upregulation of the PLD pathway.
Keywords: tumour necrosis factor α, intestinal epithelia, histamine, ion secretion, phospholipase D
Patients suffering from inflammatory bowel diseases (IBD) such as ulcerative colitis or Crohn's disease experience severe diarrhoea. The underlying mechanism of the diarrhoea remains uncertain. Patients show increased release of mast cell products such as histamine and also tumour necrosis factor α (TNF-α).1, 2, 3 A number of studies have supported a predominant role for the cytokine TNF-α in the pathogenesis of IBD. In bowel mucosa of IBD patients, mRNA levels of TNF-α are increased4 as well as concentrations of the protein in blood and stool.5, 6 Moreover, TNF-α secretion from infiltrated inflammatory cells is enhanced in biopsies from these patients.3 Antibodies against this cytokine appear to be successful in the therapy of patients with Crohn's disease resulting in diminished symptoms of the disease.7 These data imply that TNF-α plays an important role in the pathogenesis of diarrhoea in these patients.
Chloride secretion across the intestinal epithelium plays an important role in water secretion into the lumen of the intestine. Increased chloride secretion can result in severe diarrhoea due to excessive water secretion into the lumen. In several models it was shown that histamine increased chloride secretion. Histamine is thought to stimulate ion secretion in colonic epithelium via increased prostaglandin release or via the augmenting effects of endogenously released neurotransmitter.8–11 In the intestinal epithelial cell line T84, histamine increases chloride secretion via increased intracellular calcium levels due to activation of the phospholipase C pathway by the histamine receptor.12 This pathway resembles that of muscarinic receptor activation and in HT29cl.19A cells intracellular electrophysiological effects of histamine resemble those of carbachol (see below).
Recently, we showed that TNF-α potentiated carbachol induced chloride secretion in HT29cl.19A cells in a protein synthesis dependent manner. We deduced that the potentiation could be a result of increased protein kinase C (PKC) activity as a consequence of increased 1,2-diacylglycerol (DAG) levels due to upregulation of the phospholipase D (PLD) pathway.13 This proposition was corroborated by analysis of membrane phospholipids.14 To our knowledge, this was the first time a potentiating effect of TNF-α on epithelial ion secretion had been shown.
Based on the similarities between activation of muscarinic receptors and histamine receptors, our aim was to study if TNF-α could also potentiate the effect of the mast cell mediator histamine. Because it is important to validate the results obtained in cell lines in native tissue, we also studied the effect of TNF-α and histamine on ion secretion in mouse isolated distal colon.
The present data showed that TNF-α potentiates ion secretion induced by histamine in HT29cl.19A cells via de novo protein synthesis and most probably by upregulating the PLD pathway, thereby generating enhanced DAG levels and subsequent PKC activation. Furthermore, we demonstrated that TNF-α also augments the secretory response to histamine in mouse distal colon indicating the generality of the observed effect in the human cell line.
The present results suggest a synergy between the mast cell products histamine and TNF-α in stimulating ion secretion in intestinal epithelium, and this may contribute to symptoms in patients with IBD.
MATERIAL AND METHODS
Cell culture
HT29cl.19A cells were cultured as described previously.15 Briefly, the human intestinal epithelial cell line HT29cl.19A, passages 17–29, was grown in Dulbecco's modified Eagle's medium, supplemented with 10% fetal bovine serum, 8 mg/l ampicillin, and 10 mg/l streptomycin. Cells were seeded in 25 cm2 flasks at 37°C in 5% CO2–95% O2 and passaged weekly. For the experiments, cells were subcultured on Falcon filters (25 mm Ø), and medium was replaced every other day. Confluency was reached seven days after seeding, and filters with cells were used between 13 and 19 days post seeding. TNF-α incubations were performed in culture media during the indicated times.
Electrophysiological experiments with HT29cl.19A cells
The filter was cut from the ring, divided into four pieces, and rinsed with mannitol-Ringer. One piece was mounted in a small horizontal Ussing chamber, leaving an oblong area of 0.35 cm2. The apical and basolateral compartments were continuously perfused with mannitol-Ringer buffer at a temperature of 37°C and gassed with 5% CO2–95% O2. The composition of Ringer's solution was (in mM): NaCl 117.5, KCl 5.7, NaHCO3 25.0, NaH2PO4 1.2, CaCl2 2.5, MgSO4 1.2, and mannitol 28. Agar bridges were placed in apical and basolateral compartments and were connected to Ag-AgCl electrodes for monitoring the transepithelial potential difference (Vt). An extra Ag-AgCl electrode was placed in the apical bath, serving as a common ground. Apical membrane potential (Va) was measured by impalement with a glass microelectrode, pulled from capillaries (1 mm od; Clark Electromedical, Reading, UK) with a Flaming Brown P-87 micropipette puller. The microelectrode was filled with 0.5 M KCl solution. Tip resistance was 100–200 MΩ and tip potential 2–5 mV. Current electrodes (Ag-AgCl) were placed in the walls of both compartments; these were used to apply bipolar current pulses from a floating current source of 10 and 50 μA at 30 second intervals to calculate transepithelial resistance (Rt) and fractional resistance fRa (fRa=Ra/(Ra+Rb)). The equivalent short circuit current (Isc) was calculated from Vt and Rt.
The potentials were measured differentially with M-4A electrometer probes (W-P-Instruments, New Haven, USA). Potential differences were continuously recorded on a multipen recorder and on a computer using custom made software.
Measurements were corrected for the offset of the electrodes and for the resistances of the fluid and filter without cells.
Phospholipid analysis in HT29cl.19A cells
Cells were labelled for 24 hours with 1.85×106–3.7×106 Bq 32Pi at the mucosal side and were washed with Ringer's solution to remove unincorporated 32Pi. Cells were stimulated for 30 minutes with 100 μM histamine in the presence of 0.05% 1-butanol (v/v). The concentration of 1-butanol and the time of incubation were chosen based on results described in a previous study.14 Reactions were stopped with 0.1 N HCl. Cells are frozen for 30 minutes (−20°C) and scraped off the filters, and lipids were extracted as described previously.16
Extracted lipids were separated on heat activated TLC plates using an ethyl acetate solvent system (ethyl acetate/iso-octane/formic acid/water (13:2:3:10, by vol)).17 The TLC plate was exposed to a photographic film overnight and levels of 32P labelled phosphatidic acid (PA) and phosphatidylbutanol (PBut) were quantified by phosphoimaging (Storm, Molecular Dynamics).
Tissue preparation
Female Balb/C mice were used. They had access to food and water ad libitum. The animals were killed by cervical dislocation. The intestine was cut proximal from the caecum and proximal from the rectum. The colon was rinsed with inosine-Ringer to remove any faeces and placed over a thin plastic rod. The distal colon was taken 2 cm distal from the caecum and cut along the mesenteric border across a length of 1 cm. The excised segments were mounted on a sledge18 and placed in a modified Ussing chamber kept at a temperature of 37°C. The exposed area was 0.2 cm2 and the volume of the serosal and mucosal bath was 2 ml each. The composition of the Ringer's solution was (in mM): NaCl 117.5, KCl 5.7, NaHCO3 25.0, NaH2PO4 1.2, CaCl2 2.5, MgSO4 1.2, inosine 5, β-OH-butyrate 0.5, glutamine 2.5+50 mg/l azlocillin (modified from Grotjohann and colleagues19). Ringer's solution in the two compartments was refreshed every 30 minutes to avoid bacterial overflow. The solution was circulated by a gas lift using 5% CO2/95% O2.
Electrophysiological measurements in distal mouse colon
Agar bridges were placed in apical and basolateral compartments and were connected to Ag-AgCl electrodes for monitoring Vt. Platina electrodes were placed in serosal and mucosal chambers and current injections of +10 μA and −10 μA were given to measure Rt of the epithelia. From Vt and Rt the short circuit current Isc was calculated.
Potential difference was continuously recorded on a notebook using custom made software. Measurements were corrected for the offset of the electrodes and for the resistance of the fluid.
Materials
TNF-α and (San Diego, California, USA) GF109203X (bisindolylmaleimide I) were from Calbiochem. Propranolol, histamine, cycloheximide, azlocillin, tetrodotoxin (TTX), β-OH-butyrate, indomethacin, and amiloride were purchased from Sigma (St Louis, Missouri, USA), and 1-butanol from Brocades (Delft, the Netherlands). Silica 60 TLC plates and reagents for lipid extraction were from Merck (Darmstadt, Germany). [32P] Orthophosphate (32Pi; carrier free) was from Amersham International (Uppsala, Sweden). All drugs were dissolved in water except for indomethacin and cycloheximide which were dissolved in ethanol with a maximal concentration of 0.1% ethanol in the Ussing chamber. Concentrations of GF109203X, TNF-α, cycloheximide, and 1-butanol were chosen based on earlier studies with this cell line.13 Concentrations were taken from the literature for histamine, propranolol, indomethacin, and amiloride.20–22
Statistics
Data are presented as means (SEM). Statistical significance was evaluated using a Student's t test or a non-parametric test. In the corresponding text, p values are given and in the legends the test is indicated.
RESULTS
Electrophysiology in HT29.cl19A cells
TNF-α potentiates ion secretion induced by histamine in HT29cl.19A cells
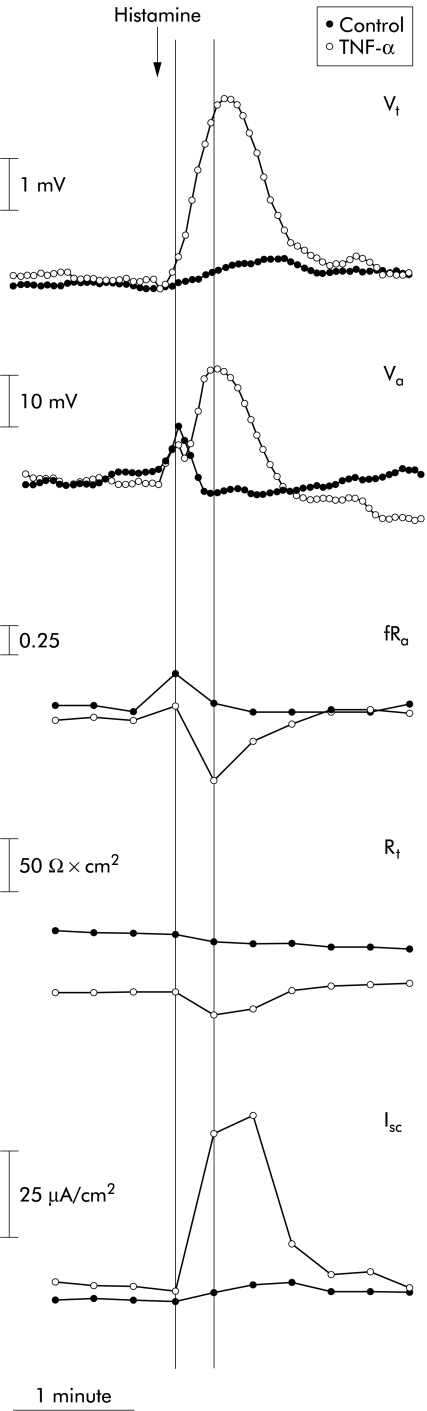
A typical electrical response to 100 μM histamine in HT29cl.19A cells is shown in fig 1 ▶. The response is divided into two phases: the first from the time of histamine application to the first vertical thin line (fig 1 ▶) and the second as the period thereafter. In table 1 ▶, the electrophysiological parameters for the control responses are summarised. They were taken at the two thin vertical lines indicated in fig 1 ▶. Application of 100 μM histamine to the serosal side of the cells resulted in fast depolarisation of the apical membrane potential (Va) together with an increase in fRa during phase 1 without a significant change in Isc or Vt. In phase 2, depolarisation of Va was followed by repolarisation leading to hyperpolarisation, concomitantly with an increase in Vt, decrease in Rt, and increase in Isc. fRa returned to basal values. To our knowledge, this response has not been described previously in detail. Muscarinic receptor activation by carbachol triggers the same intracellular response (although usually larger) and thus based on earlier studies with carbachol23 we explain the changes in the parameters as follows. The first phase—depolarisation without a change in Vt—is attributed to opening of the chloride channels located in both membranes of the cells which are activated by increased intracellular calcium levels, primarily from the inositol 1,4,5-trisphosphate (IP3) sensitive intracellular pool. The following hyperpolarisation of Va and increase in Vt and Isc is ascribed to increased calcium dependent potassium conductance located in the basolateral membrane. This increases the driving force for chloride efflux through the apical membrane through chloride channels, which are believed to be activated by PKC-α.24
Figure 1.
Changes in the electrophysiological parameters of HT29cl.19A cells after addition of 100 μM histamine in the absence or presence of 10 ng/ml tumour necrosis factor α (TNF-α). Two tracings (control and TNF-α treated groups) represent experiments in which intracellular recordings were obtained. Two thin lines divide the response into phases 1 and 2, as described in the results. Vt, transepithelial potential; Va, intracellular potential; fRa, fractional apical resistance (fRa= Ra/(Ra+ Rb)); Rt, transepithelial resistance; Isc, short circuit current. (For statistics see table 1 ▶.)
Table 1.
Electrophysiological parameters of HT29cl.19A cells before and after application of histamine
| Vt (mV) | Rt (Ω×cm2) | Va (mV) | fRa | Isc (μA/cm2) | |
| Control | |||||
| Baseline | 1.7 (0.7) | 195 (10) | −62 (6) | 0.67 (0.02) | 9.5 (5) |
| Histamine phase 1 | 1.6 (0.7) | 195 (10) | −58 (3) | 0.73 (0.05) | 8.9 (5) |
| Histamine phase 2 | 2.5 (0.8) | 190 (11) | −66 (7) | 0.65 (0.02) | 14 (6) |
| ΔHistamine | 0.8 (0.1) | −5 (2) | −4 (0.4) | −0.02 (0.01) | 5 (1) |
| TNF-α | |||||
| Baseline | 2.2 (0.7) | 173 (12) | −57 (2) | 0.70 (0.06) | 13 (4) |
| Histamine phase 1 | 2.1 (0.7) | 173 (12) | −54 (3) | 0.73 (0.05) | 12 (4) |
| Histamine phase 2 | 8.4 (1)** | 154 (11)** | −38 (2)** | 0.47 (0.07)** | 58 (11)** |
| ΔHistamine | 6.2 (0.8)** | −20 (5)** | 19 (3)** | −0.24 (0.05)** | 45 (10)** |
TNF-α, tumour necrosis factor α; Vt, transepithelial potential; Va, intracellular potential; Isc, short circuit current; Rt, transepithelial resistance; fRa, fractional resistance.
Effects of addition of 100 μM histamine to the serosal side of the cells. ΔHistamine represents the difference between phase 2 and baseline.
n=5 for control experiments; n=7 for TNF-α exposed monolayers except for Va and fRa (n=5).
Mean incubation time for TNFα (10 ng/ml) was 6–24 hours.
Statistical significance was evaluated using the Students t test: **p<0.01 compared with control histamine.
Incubation for 24 hours with 10 ng/ml TNF-α (bilaterally) did not change basal electrophysiological parameters. The parameters, representing seven experiments, are presented in table 1 ▶. In fig 1 ▶ a typical electrophysiological response to histamine after exposure to TNF-α is shown. After exposure of cells to TNF-α, the first phase depolarisation was not affected. However, instead of repolarisation in the second phase, a prolonged depolarisation of Va occurred in TNF-α exposed cells. The decrease in fRa was significantly larger. The change in Vt was increased and the change in Rt was also significantly larger. The histamine induced increase in Isc was ninefold larger after exposure to TNF-α. The effects of exposure to TNF-α on the response to histamine are similar to its potentiating effect on the response to carbachol where we argued that this must be due to increased apical chloride conductance.13
Cycloheximide prevents the potentiating effect of TNF-α
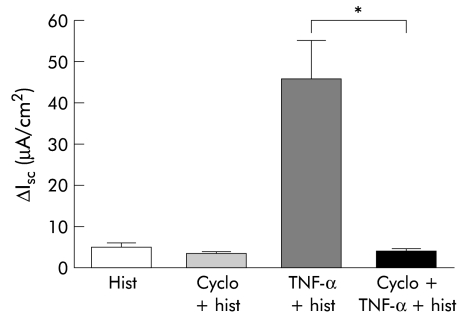
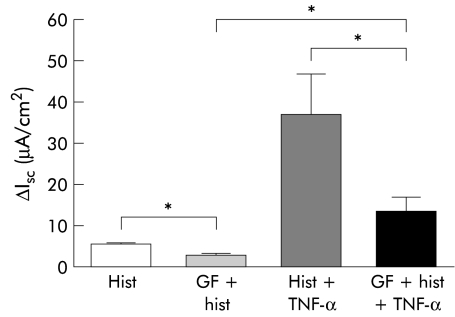
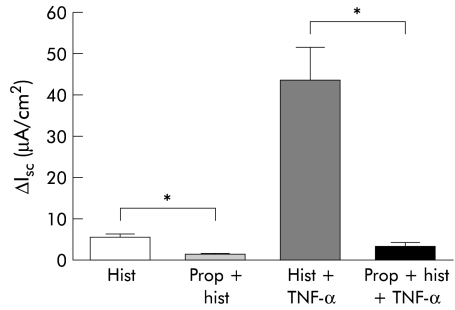
To examine whether the action of TNF-α was dependent on protein synthesis, we incubated cells with the protein synthesis inhibitor cycloheximide one hour prior to TNF-α application and measured Isc induced by histamine. Addition of 10 μg/ml cycloheximide did not affect basal parameters (not shown). Figure 2 ▶ shows that Isc induced by histamine was not significantly affected after application of cycloheximide over one hour (5.0 (1) μA/cm2 for controls v 3.5 (0.4) μA/cm2 for cycloheximide; n=3). However, in the presence of cycloheximide the potentiating effect of TNF-α on histamine-induced Isc was completely inhibited (45 (9.6) μA/cm2 for TNF-α v 3.7 (0.7) μA/cm2 for cycloheximide+TNF-α; p<0.001; n=4), as shown in fig 2 ▶. These results show that the effect of TNF-α is dependent on de novo protein synthesis.
Figure 2.
Effect of cycloheximide on maximal change in short circuit current (Isc) induced by histamine (hist) with or without exposure to tumour necrosis factor α (TNF-α). Cells were incubated with 10 μg/ml cycloheximide (cyclo) bilaterally for one hour before TNF-α exposure (4–5 hours). Data are presented as means (SEM) from 3–7 monolayers. Statistical significance was evaluated using the non-parametric Mann-Whitney test: *p<0.05.
Involvement of PKC in the histamine response
To investigate the role of PKC in the secretory response to histamine and in the potentiating effect of TNF-α, cells were preincubated with 1 μM GF109203X on both sides of the cells over 30 minutes. We demonstrated previously that at this concentration GF109203X can be used as an inhibitor of PKC.13 In fig 3 ▶ it is shown that incubating cells with GF109203X prior to addition of histamine decreased histamine induced Isc from 5.6 (0.3) to 3.1 (0.3) μA/cm2 (n=5; p<0.005), suggesting a role for PKC in histaminic receptor activation. Pre-exposure with GF109203X decreased the TNF-α potentiated histamine response from 37.3 (9.7) to 13.7 (3.6) μA/cm2 (n=6; p<0.05) but the potentiating effect of TNF-α was still present. These results indicate that PKC activation is involved in the secretory response to histamine as well as in the TNF-α potentiated response.
Figure 3.
Effect of GF109203X on the maximal change in short circuit current (Isc) induced by histamine with or without exposure to tumour necrosis factor α (TNF-α). Cells were incubated with 1 μM GF109203X (GF) 30 minutes prior to addition of histamine (hist). Data are presented as means (SEM) from 5–6 monolayers. Cells were exposed to TNF-α for 5–24 hours. Statistical significance was evaluated using the Student's t test: *p<0.05.
Involvement of PLD in the histamine response
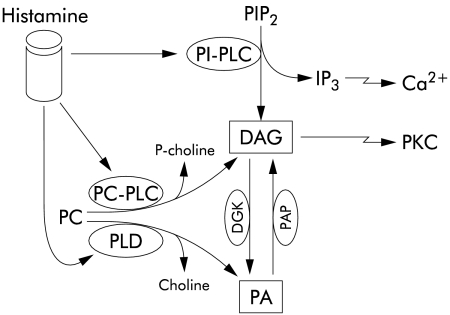
In our previous study13 we argued that exposure of cells to TNF-α would make them more susceptible to PKC activation by muscarinic receptor related intracellular messengers—for example, via increased DAG production. DAG can be generated via different pathways. The phosphatidylinositol-PLC pathway has been identified as necessary for histamine receptor activation in intestinal epithelial cells and hydrolyses the membrane lipid phosphatidylinositol 4,5-bisphospate (PIP2) into DAG and IP3.25 IP3 is related to increased intracellular calcium which determines the first phase of the electrophysiological response. Because this phase was unchanged, we excluded activation of this pathway by TNF-α. Furthermore, DAG can be generated by hydrolysis of structural phospholipids, such as phosphatidylcholine by PLD via the intermediate product PA. PA is subsequently hydrolysed by phosphatidic acid phosphatase (PAP) to DAG. A schematic presentation of the second messenger pathways involved in histaminic receptor activation is presented in fig 4 ▶.
Figure 4.
Schematic representation of the signalling mechanisms involved in histaminic receptor activation. PC, phosphatidylcholine; PIP2, phosphatidylinositol 4,5-bisphosphate; PI-PLC, phosphatidylinositol phospholipase C; PLD, phospholipase D; DAG, 1,2-diacylglycerol; PA, phosphatidic acid; IP3, inositol 1,4,5-trisphosphate; DGK, DAG kinase; PAP, phosphatidic acid phosphatase.
To investigate the role of the PLD/PAP pathway in the histamine response, we used propranolol to inhibit PAP.21 In a previous study we have shown that in these cells levels of PA increase twofold after treatment with propranolol, which confirms the inhibitory action of the substance in these cells.14 Cells were incubated with 100 μM propranolol on the apical side of the cells for 10 minutes prior to histamine application. The change in Isc induced by histamine is shown in fig 5 ▶. In the presence of propranolol the increase in Isc by histamine was reduced from 5.7 (0.6) to 1.6 (0.6) μA/cm2 (n=3; p<0.05). After exposure to TNF-α, Isc induced by histamine was reduced by propranolol from 43.7 (7.7) to 3.3 (1.3) μA/cm2 (n=4; p<0.05). Thus the potentiating effect of TNF-α was completely abolished. These results suggest that the PAP/PLD pathway is involved in the histamine response in these cells and that TNF-α possibly exerts its potentiating effect on histamine induced secretion via upregulation of the PAP/PLD pathway.
Figure 5.
Effect of propranolol on the maximal change in short circuit current (Isc) induced by histamine with or without exposure to tumour necrosis factor α (TNF-α). Cells were incubated with 100 μM propranolol (prop) 10 minutes prior to addition of histamine (hist). Data are presented as means (SEM) from 3–4 monolayers. Cells were exposed to TNF-α for 5–24 hours. Statistical significance of the differences in change in Isc was evaluated using the non-parametric Mann-Whitney test: *p<0.05.
Phospholipid analysis
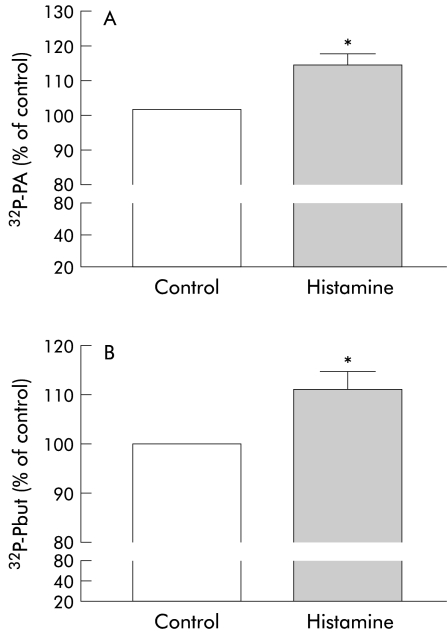
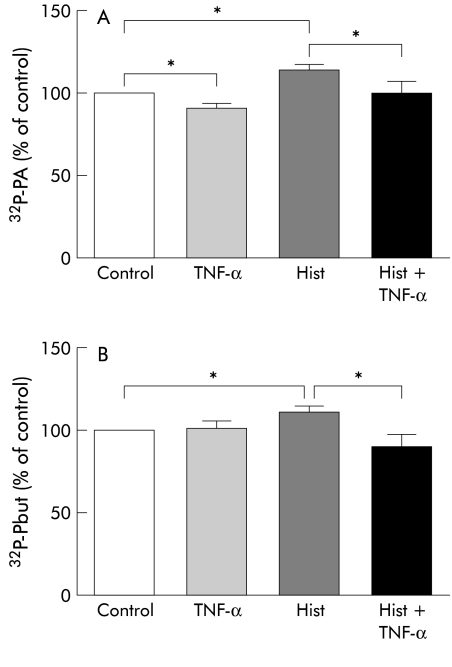
PBut and PA formation by histamine
Previous results suggested that the PAP/PLD pathway is involved in histaminic receptor activation and that TNF-α exerts its potentiating effect via this pathway. To investigate this we measured PLD activity. The enzyme PLD has the unique ability to transfer the phosphatidyl group of its substrate to a primary alcohol such as 1-butanol instead of water, forming phosphatidylbutanol (Pbut).26 Unlike PA, this is a stable product and therefore the relative amount of PBut formed is a measure of PLD activation. After labelling the cells with 32Pi, cells were stimulated with histamine for 30 minutes in the presence of 0.05 % 1-butanol. Incubation time and concentration were chosen based on results described in a previous study.14 Incubation with 100 μM histamine resulted in an increase in PA and PBut levels to 114 (3)% and 111 (3)%, respectively (n=5; p<0.05) compared with cells not exposed to histamine (100%) (fig 6A and 6B ▶, respectively). Figure 7A ▶ shows that levels of 32P-PA decreased after 24 hours of exposure to 10 ng/ml TNF-α to 91 (3)% compared with cells without TNF-α (100%; p<0.005; n=5). Also, the increase in 32P-PA level by histamine was decreased to 88 (6)% (n=5; p<0.01) with respect to histamine alone. Exposure to TNF-α did not affect the level of 32P-PBut (101 (4)% compared with control 100%; n=5) (fig 7B ▶). However, the presence of TNF-α significantly decreased 32P-PBut levels to 81 (7)% compared with cells exposed to histamine alone (100%; n=5; p<0.005).
Figure 6.
Effect of histamine on levels of 32P-phosphatidic acid (PA) (A) and 32P-phosphatidylbutanol (PBut) (B) in HT29cl.19A cells. Cells were stimulated for 30 minutes with 100 μM histamine in the presence of 0.05% 1-butanol. Data are shown as percentage of control monolayers (100%). The basal 32P-PA level was 2.32 (0.28)% of total labelled phospholipids and basal 32P-PBut was 0.38 (0.06)% of total labelled phospholipids. About 20% of the total label was incorporated into phosphatidylcholine. The other labelled phospholipids cannot be distinguished on this system. Data are presented as means (SEM) of five monolayers. Statistical significance was evaluated using the Student's t test: *p<0.05.
Figure 7.
Effect of tumour necrosis factor α (TNF-α) on basal and histamine induced levels of 32P-phosphatidic acid (PA) (A) and 32P-phosphatidylbutanol (PBut) (B). Cells were exposed to 10 ng/ml TNF-α over the 24 hour labelling period. Cells were stimulated with 100 μM histamine (hist). Application of histamine resulted in significantly increased levels of 32P-PA and 32P-PBut, as indicated in fig 5 ▶. Data are shown as percentage change from control experiments. Data are presented as means (SEM) of five monolayers. Statistical significance was evaluated using the Student's t test: *p<0.05.
These results suggest that histaminic receptor activation results in activation of the PAP/PLD pathway and that TNF-α upregulates expression or activity of PAP, resulting in decreased PA levels. Reduction in the stable 32P-PBut levels seems anomalous. A possible explanation will be given in the discussion.
Electrophysiology of distal colon of the mouse
TNF-α potentiates the histamine induced secretory response in mouse distal colon
It is important to know whether the previous results can be extrapolated to native tissues. Therefore, the effect of TNF-α on ion secretion induced by histamine in mouse distal colon was studied. We chose the mouse colon as the cell line we used represents colonic epithelia and because mouse recombinant TNF-α was available.
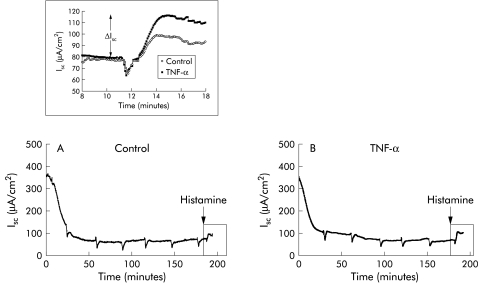
One piece of distal colon was removed from each mouse and mounted in an Ussing chamber, as described in the materials and methods section. To diminish Isc, which may be induced by subepithelial and neuronal factors in distal colon, we used the following agents. Amiloride (100 μM) was added immediately after mounting to block mucosal Na+ influx. On the serosal side, TTX 0.3 μM was added to block neuronal activity and indomethacin 1 μM to block ion secretion induced by release of prostaglandins. Figure 8A and B ▶ show two typical recordings, each representing four experiments for control and TNF-α exposed epithelia (50 ng/ml; three hours), respectively. Every 30 minutes Ringer's solution containing antibiotics was replaced to remove possible accumulated bacteria in the chambers. After changing Ringer's solution, Isc recovers, which can be seen in figure 8A and 8B ▶. In the first hour, Isc decreases rapidly after which it remains at a steady level. No differences in transepithelial potential or resistance were observed between control epithelia and epithelia exposed for three hours to 50 ng/ml TNF-α. In table 2 ▶ changes in electrophysiological parameters on histamine application are presented. In the inset in fig 8 ▶, enlargement of the frames indicated are presented. Addition of histamine resulted in an increase in Vt, preceded by a small decrease in Vt. Rt slightly decreased after addition of histamine (−4 (1) Ω/cm2) and Isc increased to 21 (5) μA/cm2 with respect to baseline values. After exposure to TNF-α, the change in Vt was increased compared with control epithelia (n=4; p<0.01) and the change in Rt was larger than that in control experiments (n=4; p<0.01). Isc induced by histamine was 2.6-fold larger than in control epithelia (n=4; p<0.01).
Figure 8.
Changes in short circuit current (Isc) across mouse distal colon over a three hour period of measurements for two typical experiments of control (A) and tumour necrosis factor α (TNF-α) exposed tissues (B). At t=0 tissues were mounted and transepithelial potential and transepithelial resistance were continuously recorded. Every 30 minutes Ringer's solution was replaced which shows as a drop in Isc during the recording. Histamine was added at the time point indicated by the arrow. The frames are enlarged in the inset. Two typical recordings of Isc from mouse distal colon of control and TNF-α exposed tissues are presented in the inset. The change in current with respect to baseline levels is indicated by ΔIsc. The recordings represent four experiments for each group. The corresponding electrophysiological data are presented in table 2 ▶. Statistical significance was evaluated using the Student's t test.
Table 2.
Electrophysiological parameters of mouse distal colon before and after application of 100 μM histamine
| Vt (mV) | Rt (Ω×cm2) | Isc (μA/cm2) | |
| Control | |||
| Baseline | 2.4 (0.6) | 35 (5) | 67 (8) |
| Histamine | 2.8 (0.7) | 31 (4) | 88 (13) |
| ΔHistamine | 0.4 (0.1) | −4 (1) | 21 (5) |
| TNF-α | |||
| Baseline | 3.6 (0.6) | 51 (11) | 77 (12) |
| Histamine | 4.8 (1.0) | 38 (7) | 130 (16)** |
| ΔHistamine | 1.1 (0.2)** | −13 (5)** | 54 (7)** |
TNF-α, tumour necrosis factor α; Vt, transepithelial potential; Isc, short circuit current; Rt, transepithelial resistance.
Effects of addition of 100 μM histamine to the serosal side of the tissues with or without exposure to 50 ng/ml TNF-α over three hours (n=4 for the two groups).
Statistical significance was evaluated using the Student's t test: **p<0.01 compared with control histamine.
These results confirm that TNF-α also potentiates histamine induced ion secretion in mouse native tissue.
DISCUSSION
In the present study we have shown that exposure to 10 ng/ml TNF-α potentiated ion secretion induced by histamine in the colonic epithelial cell line HT29cl.19A. The effect of TNF-α was completely blocked by cycloheximide, which indicates that de novo synthesis of a protein is involved in the action of TNF-α. TNF-α did not affect basal electrophysiological parameters. This, together with our previous finding that TNF-α potentiates ion secretion induced by carbachol,13 suggests that TNF-α exerts its effect downstream of the histamine receptor. The intracellular recordings show that after exposure to TNF-α activation of chloride conductance, located in the apical membrane, is enhanced. It is unlikely that this chloride conductance is activated by increased calcium levels as the first phase depolarisation is not affected by TNF-α. Moreover, earlier results showed that the response to the calcium ionophore ionomycin was not affected by TNF-α exposure.13 Apical chloride conductance can also be increased by PKC activation.27 The present results indicate that PKC activation is involved in the histamine response in these cells and in TNF-α potentiated ion secretion. Because even in the presence of GF109203X (which only partially inhibits PKC28) TNF-α exerts its potentiating effect and because we found previously that TNF-α does not affect 4β-phorbol-12,13-dibutyrate induced ion secretion,13 we hypothesise that TNF-α stimulates the synthesis of a protein involved in the second messenger pathway between histaminic receptor activation and PKC activation.
The diminished electrophysiological response to histamine after propranolol exposure implicates PLD/PAP activation in histaminic receptor activation in these cells. The marked suppression (over 70%) suggests that PLD activation plays a major role in ion secretion induced by histamine. Furthermore, blocking PAP with propranolol completely prevented the potentiating effect of TNF-α, implying that TNF-α acts via this pathway. Measurement of levels of PA and the stable PLD product PBut established that application of histamine leads to activation of PLD in these cells. Activation of the PAP/PLD pathway by histamine has been described previously. In oligodendroglioma cells and pulmonary endothelium, it was shown that histamine application resulted in PLD activation.29, 30 Interestingly, levels of PA are decreased in the presence of TNF-α. This suggests that TNF-α exerts its effect on the PAP/PLD pathway by upregulation of expression or activity of the protein PAP, thereby increasing turnover from PA to DAG. The increased formation of DAG may activate PKC. Exposure to TNF-α also results in decreased PBut levels induced by histamine. PLD activity can be enhanced by PA31 and by PIP2, which is formed by the PA dependent PIP kinase.32 Thus when PA levels are decreased due to TNF-α-induced PAP activity, histamine may stimulate PLD to a lesser extent after TNF-α exposure, resulting in less elevated PBut levels.
Interestingly, in mouse distal colon the histamine response was also potentiated by TNF-α, which indicates the generality of the observed effect in the cell line. Apparently, TNF-α and histamine synergistically stimulate ion secretion in the distal colon also. To our knowledge this is the first study in which a direct effect of TNF-α on ion transport in intestinal tissue has been demonstrated. In porcine ileum and human distal colon, TNF-α was shown to increase basal Isc via increased synthesis of subepithelial prostaglandins.33, 34 We exclude this possibility in the present study as we performed our experiments in the presence of indomethacin, an inhibitor of prostaglandin synthesis.
The effect of histamine on chloride secretion in the colon has been extensively studied in different species. In mouse caecum, rat colon, guinea pig colon, porcine distal colon, and human colon histamine induces a transient increase in Isc.8–11, 20 In the guinea pig, histamine acts via augmenting the effects of endogenously released neurotransmitters.10 Hardcastle and Hardcastle were the first to show that histamine in rat colon induces chloride secretion partly via release of prostaglandins.9 Also, in mouse caecum histamine causes the majority of its effect through stimulating arachidonic acid metabolism.20 The increase in histamine related Isc in our study was not due to indirect neuronal stimulation or prostaglandin release as we measured the histamine response after blocking both pathways by TTX and indomethacin, respectively. The response of HT29cl.19A cells and of T84 cells12 shows that the cell lines express histamine receptors and from our intracellular observations we conclude that histamine triggers a similar intracellular messenger system as carbachol. It remains to be established whether histamine induced ion secretion in mouse distal colon is dependent on the same intracellular messengers. We showed previously that TNF-α also potentiated ion secretion induced by carbachol in HT29cl.19A cells. This would imply that the effects of other mediators, such as bradykinin which uses the same intracellular system, can be potentiated by TNF-α via the PLD pathway.
The role of histamine and TNF-α in patients suffering from IBD has been widely studied but the precise contribution of the inflammatory mediators remains uncertain. Human intestinal mast cells are a major source of histamine and TNF-α.35 Biopsies from IBD patients show increased levels of histamine and TNF-α.1, 3 The present study revealed that these inflammatory modulators augment synergistically ion secretion in the studied models but the precise contribution to the pathogenesis of the disease remains unknown. Crowe et al showed that in inflamed tissue from IBD patients, the secretory response to mast cell activation by anti-IgE was diminished.36 They postulated that prior activation of mast cell with release of histamine may account for the reduced secretory response to anti-IgE observed in IBD colonic tissue. Others have also shown hyporesponsiveness to other secretagogues in the intestine of animal models for IBD.37, 38 It has been suggested previously that epithelial damage due to cytokines might be the underlying reason for the hyporesponsiveness but under conditions used in the present experiments we found no evidence of damage.13 According to our data, we hypothesise that hyporesponsiveness may be due to downregulation of one or more steps in the secretory pathway because of prolonged activity of PKC. Prolonged activation of PKC is known to inhibit basolateral K+ conductance, resulting in an inability to reveal a secretory response to secretagogues. This suggests that the synergistic effect of TNF-α and histamine on ion secretion is more likely involved in an early initiating phase of the disease than longer term. Then, the synergistic effect of histamine and TNF-α on activation of PKC may account for the reduced ion transport in models of IBD.
It has been described previously that TNF-α can also act synergistically with another immunomodulator interferon γ (IFN-γ) in altering epithelial physiology in intestinal epithelial cells (T84 cells).39, 40 This is probably attributed to induction of TNF-α receptors by IFN-γ.41 Thus it may be that in the presence of both cytokines the effect of secretagogues is even more potentiated. Recently, it has been shown that TNF-α is a stimulus for mast cells to release histamine42 and because the release process of TNF-α is regulated differentially from degranulation,43 it may be that TNF-α activates histamine release in an autocrine way.
In summary, TNF-α potentiates ion secretion induced by histamine in HT29cl.19A cells via a protein synthesis dependent mechanism. We hypothesise that TNF-α upregulates expression or the activity of PAP, thereby increasing DAG formation and subsequent PKC activation. This augments ion secretion induced by histamine. Interestingly, in mouse distal colon, TNF-α also potentiated histamine induced ion secretion. It remains to be seen whether the PKC and PAP/PLD pathway are involved in the secretory response to histamine in mouse distal colon and whether this mechanism is involved in the pathogenesis of IBD related phenomena.
Abbreviations
TNF-α, tumour necrosis factor α
PKC, protein kinase C
DAG, 1,2-diacylglycerol
PLD, phospholipase D
PA, phosphatidic acid
PAP, PA phosphatase
PBut, phosphatidylbutanol
IBD, inflammatory bowel disease
Vt, transepithelial potential
Va, intracellular potential
Isc, short circuit current
Rt, transepithelial resistance
fRa, fractional resistance
PIP2, phosphatidylinositol 4,5-bisphospate
TTX, tetrodotoxin
IFN-γ, interferon γ
IP3, inositol 1,4,5-trisphosphate
REFERENCES
- 1.Rampton DS, Murdoch RD, Sladen GE. Rectal mucosal histamine release in ulcerative colitis. Clin Sci 1980;59:389–91. [DOI] [PubMed] [Google Scholar]
- 2.Knutson L, Ahrenstedt O, Odlind B, et al. The jejunal secretion of histamine is increased in active Crohn's disease. Gastroenterology 1990;98:849–54. [DOI] [PubMed] [Google Scholar]
- 3.Reinecker HC, Steffen M, Witthoeft T, et al. Enhanced secretion of tumour necrosis factor-alpha, IL-6, and IL-1 beta by isolated lamina propria mononuclear cells from patients with ulcerative colitis and Crohn's disease. Clin Exp Immunol 1993;94:174–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cappello M, Keshav S, Prince C, et al. Detection of mRNAs for macrophage products in inflammatory bowel disease by in situ hybridisation. Gut 1992;33:1214–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murch SH, Braegger CP, Walker-Smith JA, et al. Location of tumour necrosis factor alpha by immunohistochemistry in chronic inflammatory bowel disease. Gut 1993;34:1705–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braegger CP, Nicholls S, Murch SH, et al. Tumour necrosis factor alpha in stool as a marker of intestinal inflammation. Lancet 1992;339:89–91. [DOI] [PubMed] [Google Scholar]
- 7.Targan SR, Hanauer SB, van Deventer SJ, et al. A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn's disease. N Engl J Med 1997;337:1029–35. [DOI] [PubMed] [Google Scholar]
- 8.Traynor TR, Brown DR, O'Grady SM. Effects of inflammatory mediators on electrolyte transport across the porcine distal colon epithelium. J Pharmacol Exp Ther 1993;264:61–6. [PubMed] [Google Scholar]
- 9.Hardcastle J, Hardcastle PT. Involvement of prostaglandins in histamine-induced fluid and electrolyte secretion by rat colon. J Pharm Pharmacol 1988;40:106–10. [DOI] [PubMed] [Google Scholar]
- 10.Wang YZ, Cooke HJ, Su HC, et al. Histamine augments colonic secretion in guinea pig distal colon. Am J Physiol 1990;258:G432–9. [DOI] [PubMed] [Google Scholar]
- 11.Keely SJ, Stack WA, O'Donoghue DP, et al. Regulation of ion transport by histamine in human colon. Eur J Pharmacol 1995;279:203–9. [DOI] [PubMed] [Google Scholar]
- 12.Wasserman SI, Barrett KE, Huott PA, et al. Immune-related intestinal Cl-secretion. I. Effect of histamine on the T84 cell line. Am J Physiol 1988;254:C53–62. [DOI] [PubMed] [Google Scholar]
- 13.Oprins JCJ, Meijer HP, Groot JA. TNF-alpha potentiates the ion secretion induced by muscarinic receptor activation in HT29cl.19A cells. Am J Physiol Cell Physiol 2000;278:C463–72. [DOI] [PubMed] [Google Scholar]
- 14.Oprins JCJ, van der Burg C, Meijer HP, et al. PLD pathway involved in carbachol-induced Cl- secretion; possible role for TNF-{alpha}. Am J Physiol Cell Physiol 2001;280:C789–95. [DOI] [PubMed] [Google Scholar]
- 15.Bajnath RB, Augeron C, Laboisse CL, et al. Electrophysiological studies of forskolin-induced changes in ion transport in the human colon carcinoma cell line HT-29 cl.19A: lack of evidence for a cAMP-activated basolateral K+ conductance. J Membr Biol 1991;122:239–50. [DOI] [PubMed] [Google Scholar]
- 16.Munnik T, de Vrije T, Irvine RF, et al. Identification of diacylglycerol pyrophosphate as a novel metabolic product of phosphatidic acid during G-protein activation in plants. J Biol Chem 1996;271:15708–15. [DOI] [PubMed] [Google Scholar]
- 17.Munnik T, van Himbergen JAJ, ter Riet B, et al. Detailed analysis of the turnover of polyphosphoinositides and phosphatidic acid upon activation of phospholipases C and D in Chlamydomonas cells treated with non-permeabilizing concentrations of mastoparan. Planta 1998;207:133–45. [Google Scholar]
- 18.Groot JA, Albus H, Siegenbeek vH. A mechanistic explanation of the effect of potassium on goldfish intestinal transport. Pflugers Arch 1979;379:1–9. [DOI] [PubMed] [Google Scholar]
- 19.Grotjohann I, Schulzke JD, Fromm M. Electrogenic Na+ transport in rat late distal colon by natural and synthetic glucocorticosteroids. Am J Physiol 1999;276:G491–8. [DOI] [PubMed] [Google Scholar]
- 20.Homaidan FR, Tripodi J, Zhao L, et al. Regulation of ion transport by histamine in mouse cecum. Eur J Pharmacol 1997;331:199–204. [DOI] [PubMed] [Google Scholar]
- 21.Thompson NT, Bonser RW, Garland LG. Receptor-coupled phospholipase D and its inhibition. Trends Pharmacol Sci 1991;12:404–8. [DOI] [PubMed] [Google Scholar]
- 22.Grubb BR. Ion transport across the normal and CF neonatal murine intestine. Am J Physiol 1999;277:G167–74. [DOI] [PubMed] [Google Scholar]
- 23.Bajnath RB, Dekker K, Vaandrager AB, et al. Biphasic increase of apical Cl-conductance by muscarinic stimulation of HT-29cl.19A human colon carcinoma cell line: evidence for activation of different Cl-conductances by carbachol and forskolin. J Membr Biol 1992;127:81–94. [DOI] [PubMed] [Google Scholar]
- 24.van den Berghe N, Vaandrager AB, Bot AG, et al. Dual role for protein kinase C alpha as a regulator of ion secretion in the HT29cl.19A human colonic cell line. Biochem J 1992;285:673–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kachintorn U, Vajanaphanich M, Barrett KE, et al. Elevation of inositol tetrakisphosphate parallels inhibition of Ca(2+)- dependent Cl-secretion in T84 cells. Am J Physiol 1993;264:C671–6. [DOI] [PubMed] [Google Scholar]
- 26.Yu CH, Liu SY, Panagia V. The transphosphatidylation activity of phospholipase D. Mol Cell Biochem 1996;157:101–5. [DOI] [PubMed] [Google Scholar]
- 27.Bajnath RB, Dekker K, De Jonge HR, et al. Chloride secretion induced by phorbol dibutyrate and forskolin in the human colonic carcinoma cell line HT-29Cl.19A is regulated by different mechanisms. Pflugers Arch 1995;430:705–12. [DOI] [PubMed] [Google Scholar]
- 28.Toullec D, Pianetti P, Coste H, et al. The bisindolylmaleimide GF 109203X is a potent and selective inhibitor of protein kinase C. J Biol Chem 1991;266:15771–81. [PubMed] [Google Scholar]
- 29.Dawson G, Dawson SA, Post GR. Regulation of phospholipase D activity in a human oligodendroglioma cell line (HOG). J Neurosci Res 1993;34:324–30. [DOI] [PubMed] [Google Scholar]
- 30.Natarajan V, Garcia JG. Agonist-induced activation of phospholipase D in bovine pulmonary artery endothelial cells: regulation by protein kinase C and calcium. J Lab Clin Med 1993;121:337–47. [PubMed] [Google Scholar]
- 31.Pertile P, Liscovitch M, Chalifa V, et al. Phosphatidylinositol 4,5-bisphosphate synthesis is required for activation of phospholipase D in U937 cells. J Biol Chem 1995;270:5130–5. [DOI] [PubMed] [Google Scholar]
- 32.Geng D, Chura J, Roberts MF. Activation of phospholipase D by phosphatidic acid. Enhanced vesicle binding, phosphatidic acid-Ca2+ interaction, or an allosteric effect? J Biol Chem 1998;273:12195–202. [DOI] [PubMed] [Google Scholar]
- 33.Kandil HM, Berschneider HM, Argenzio RA. Tumour necrosis factor alpha changes porcine intestinal ion transport through a paracrine mechanism involving prostaglandins. Gut 1994;35:934–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schmitz H, Fromm M, Bode H, et al. Tumor necrosis factor-alpha induces Cl- and K+ secretion in human distal colon driven by prostaglandin E2. Am J Physiol 1996;271:G669–74. [DOI] [PubMed] [Google Scholar]
- 35.Bischoff SC, Lorentz A, Schwengberg S, et al. Mast cells are an important cellular source of tumour necrosis factor alpha in human intestinal tissue. Gut 1999;44:643–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crowe SE, Luthra GK, Perdue MH. Mast cell mediated ion transport in intestine from patients with and without inflammatory bowel disease. Gut 1997;41:785–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bell CJ, Gall DG, Wallace JL. Disruption of colonic electrolyte transport in experimental colitis. Am J Physiol 1995;268:G622–630. [DOI] [PubMed] [Google Scholar]
- 38.Asfaha S, Bell CJ, Wallace JL, et al. Prolonged colonic epithelial hyporesponsiveness after colitis: role of inducible nitric oxide synthase. Am J Physiol 1999;276:G703–10. [DOI] [PubMed] [Google Scholar]
- 39.Taylor CT, Dzus AL, Colgan SP. Autocrine regulation of epithelial permeability by hypoxia: role for polarized release of tumor necrosis factor alpha. Gastroenterology 1998;114:657–68. [DOI] [PubMed] [Google Scholar]
- 40.Fish SM, Proujansky R, Reenstra WW. Synergistic effects of interferon gamma and tumour necrosis factor alpha on T84 cell function. Gut 1999;45:191–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rodriguez P, Heyman M, Candalh C, et al. Tumour necrosis factor-alpha induces morphological and functional alterations of intestinal HT29 cl.19A cell monolayers. Cytokine 1995;7:441–8. [DOI] [PubMed] [Google Scholar]
- 42.Brzezinska-Blaszczyk E, Forczmanski M, Pietrzak A. The action of tumor necrosis factor-alpha on rat mast cells. J Interferon Cytokine Res 2000;20:377–82. [DOI] [PubMed] [Google Scholar]
- 43.Hide I, Toriu N, Nuibe T,et al. Suppression of TNF-alpha secretion by azelastine in a rat mast (RBL-2H3) cell line: evidence for differential regulation of TNF-alpha release, transcription, and degranulation. J Immunol 1997;159:2932–40. [PubMed] [Google Scholar]