Abstract
Background and aim: Accumulation and infiltration by neutrophil granulocytes is a prominent feature in the local inflammatory process in ulcerative colitis (UC). The present study was performed to evaluate human neutrophil lipocalin (HNL) as a specific neutrophil marker in the inflamed lesions of the colon and rectum in patients with colitis and proctitis.
Methods: The activity of intestinal neutrophils with respect to release of granule proteins was studied in 18 patients with UC (10 with colitis and eight with isolated proctitis) and in 18 healthy controls using perfusion fluid and biopsies from the sigmoid colon and rectum. The released amounts of the neutrophil granule proteins HNL and myeloperoxidase (MPO) were determined by radioimmunoassays, and the location of HNL and MPO in biopsies from colonic mucosa was examined by immunohistochemistry.
Results: Mucosal release of HNL and MPO was increased 10–55-fold in patients with colitis and proctitis compared with controls. Their bowel biopsies demonstrated that only neutrophils were stained with anti-HNL. We also found correlations between HNL and levels of granulocyte/macrophage-colony stimulating factor (GM-CSF) and interleukin 8 (IL-8) in perfusion fluids from the sigmoidal segments of patients with proctitis, between HNL and GM-CSF in rectal segments in patients with proctitis, and in sigmoidal segments in patients with colitis.
Conclusion: We conclude that the increased release of HNL and MPO in colorectal perfusion fluids indicates neutrophil involvement in the local inflammatory process, and suggest that HNL may serve as a specific marker of intestinal neutrophil activation in UC. GM-CSF, and to some extent IL-8, may play a role in neutrophil accumulation and priming in this disease.
Keywords: ulcerative colitis, inflammatory bowel disease, neutrophils, immunohistochemistry, cytokines
Epithelial cell damage and infiltration by neutrophil granulocytes is prominent in the local inflammatory process of ulcerative colitis (UC).1 The neutrophil granulocyte is a potent tissue injuring and cytotoxic cell with an undisputed role in the defence against bacteria. It is also believed to be largely responsible for the destructive process and symptoms seen in a variety of inflammatory diseases. Neutrophils contain two major granule populations, primary (azurophil) and secondary (specific) granules, which are formed at different stages of neutrophil maturation. Primary granules contain, as their main constituents, several proteolytic enzymes and a wide range of bactericidal proteins including cathepsin G,2 elastase,3 myeloperoxidase (MPO),4 and lysozyme.5,6 The secondary granules contain a wide variety of different components, including lactoferrin,7 lysozyme, collagenase,8,9 and lipocalins.10,11 On stimulation, the neutrophil can release large amounts of toxic oxygen radicals and a variety of granule proteins and soluble proteins such as calprotectin. It has been suggested that the influx of activated neutrophils at sites of inflammation govern the progress of many inflammatory diseases.
Several of the above mentioned proteins are not unique to the neutrophil granulocyte. MPO,12 elastase,13 and lysozyme are also found in monocytes and lysozyme also in macrophages. Lactoferrin is a neutrophil specific marker when assessed in blood but not in other body fluids as it is produced by many serous glands.7,14 Our group recently described the purification and characterisation of human neutrophil lipocalin (HNL) from secondary granules of human neutrophils. This is a protein unique to the neutrophil.15,16 For this reason, HNL would be the optimal marker for monitoring neutrophil activation. Recently, Kjeldsen et al reported data on a similar lipocalin protein, the neutrophil gelatinase associated lipocalin (NGAL), which can bind bacterial formylpeptides.17 Very high expression of NGAL was seen in colonic epithelium in areas of inflammation, both in inflammatory bowel disease (IBD) and in non-malignant epithelium, investigated by immunohistochemistry and mRNA in situ hybridisation.18 NGAL content in rectal dialysates and in faeces was suggested to be a useful marker for severe disease activity in UC.19
Local accumulation and activation of neutrophils in lamina propria may be related to proinflammatory cytokines such as interleukin 1 (IL-1), IL-6, IL-8, and tumour necrosis factor α (TNF-α). Furthermore, monocytes, activated macrophages, endothelial cells, and epithelial cells are major sources of IL-8, and IL-8 activates neutrophil chemotaxis, diapedesis, degranulation, and respiratory burst.20 IL-8 production is known to be induced by several cytokines such as IL-2, IL-3, TNF-α, and granulocyte/macrophage-colony stimulating factor (GM-CSF).21 Increased mucosal generation of IL-8 in IBD and correlations between disease activity and expression of IL-8 mRNA in active Crohn's disease have been demonstrated recently.22,23 Raab et al found a correlation between intestinal release of IL-8 and MPO, suggesting IL-8 as a possible factor in the local accumulation and activation of neutrophil granulocytes in IBD.24 Platelets from patients with IBD expressed more GM-CSF receptors compared with controls,25 and CD4+ T cells positively stained for GM-CSF were found in immunodeficient (scid) mice with IBD.26
The primary aim of our study was to evaluate HNL as a specific neutrophil marker in the colon and rectum of patients with UC compared with MPO. The secondary aim was to elucidate the location of HNL to neutrophils or epithelial cells in the inflamed mucosa, and compare it with that of MPO. We also evaluated local production of two cytokines, IL-8 and GM-CSF, that may be involved in the recruitment and activation of neutrophils in the local inflammatory process in UC.
MATERIAL AND METHODS
Patients and control group
There were 18 patients with UC (nine women and nine men; median age 38 years (range 21–75)) included in the study. Disease was defined according to the Garland criteria for definitive cases.27 Eight patients had isolated proctitis and 10 colitis; six patients had distal colitis, three left sided, and one patient had total colitis (disease extension proximal to the splenic flexure). The clinical symptoms varied from mild disease with little blood in stools to intermediately active disease with diarrhoea and blood in most stools. Six patients were treated with and two had recently finished oral and/or enema steroids; two patients had received only lidocaine enema or oral sulphasalazine, respectively. Eight patients had received no treatment.
Eighteen healthy controls (11 women and seven men; median age 27 years (range 21–64)) were also included.
The study was approved by the ethics committee of the Medical Faculty, Uppsala University.
Perfusion technique
Subjects were prepared as for routine flexible rectosigmoid endoscopy—that is, two days of diet restriction, an oral purgative in the morning and afternoon of the day before the examination, and a non-irritative rectal enema 1–2 hours before the examination, as previously reported.28 Meperidine (25–50 mg) and diazepam (2.5–5 mg) were given intravenously as routine premedication.
The perfusion technique has been described in detail elsewhere.28 The perfusions were performed with a specially constructed tube with five latex balloons attached to its wall. The procedure started with endoscopy of the rectum and sigmoid colon with the tube inserted over the endoscope. Then the tube, with the endoscope acting as a guide, was introduced into the rectum and advanced into the colon to the predetermined position and the balloons were inflated with air. Two balloons, one on each side of the anal canal, were used to stabilise the position of the tube. The other balloons created two segments, one distal rectal segment and one proximal sigmoid segment. After withdrawal of the endoscope, the position of the tube was checked fluoroscopically. Channels in the wall of the tube were used either to inflate the balloons with air, to perfuse and drain the segments, or to administer dye marker at the tip of the tube. The open main channel of the tube allowed passage of gas and fluids from the intestine above to the tube during perfusion.
The segments were perfused with a buffer (120 mM NaCl, 5.4 mM KCl, 2 mM Na2HPO4, 10 mM glucose, 35 mM mannitol, and 1 g/l polyethylene glycol (molecular weight 4 kDa), pH 7.20–7.25, osmolality 290 mosmol/l) at 37°C and at a speed of 3 ml/minute. After 70 minutes of continuous rinsing/perfusion, the perfusate was collected for 20 minutes by gravity drainage. Aprotinin 10 ml (10 000 KIU/ml) was added to every litre of perfusion buffer to inhibit proteolytic activity.
Preparation of samples
All samples were collected on ice and frozen at −70°C. Because some of the radioimmunoassays (RIA) and immunoassays used could be influenced by even small amounts of proteases in the perfusate, on the day of analysis all samples were thawed on ice and the protease inhibitor phenylmethylsulphonyl fluoride (Sigma Chemical Co., St. Louis, Missouri, USA) was added immediately to a final concentration of 2 mM before the analyses were undertaken.
RIA of MPO and HNL
The concentration of MPO in perfusion fluids was assayed using a specific RIA (Pharmacia & Upjohn, Diagnostic AB, Uppsala, Sweden) and HNL was assayed by a double antibody RIA described in detail elsewhere.29 The inter- and intra-assay coefficients of variations were <10% for all tests. The lower detection limits of each mediator were MPO 7.9 μg/l and HNL 1.9 μg/l.
Processing of biopsy specimens
Biopsies were taken from the rectal segment in five patients and five healthy controls when the perfusions had been completed, and rapidly frozen in liquid propane and stored in liquid nitrogen until sectioning. Frozen sections of a thickness of 4 μm were cut in a cryostat (Microm, HM500M, Germany) and collected on silanised microscope slides. The sections were air dried, packaged in aluminium foil, and stored at −70°C.
Immunohistochemistry
After a slow thawing of the sections, the microscope slides were placed in a humid chamber and the tissue sections were fixed and permeabilised in undiluted Ortho Permeafix (Ortho Diagnostics, UK) for 40 minutes. After a short rinse in phosphate buffered saline (PBS) and wiping of the microscope glass around the sections, a drop of PBS with 0.1% bovine serum albumin (BSA) was placed on the sections. Six different primary monoclonal anti-HNL antibodies and one monoclonal anti-MPO antibody were obtained from Pharmacia & Upjohn, Diagnostic (Uppsala, Sweden). The specificity of these antibodies had been tested by ELISA and confirmed using BIAcore (Pharmacia & Upjohn, Biosensors, Uppsala, Sweden). Sections were then incubated with a cocktail of anti-HNL antibodies in a final concentration of 0.02 mg/ml or in anti-MPO in a concentration of 0.02 mg/ml for 30 minutes at room temperature. Incubation with primary antibody was terminated by washing in PBS containing 0.2% BSA. The antigen-antibody complex was visualised using a commercial APAAP kit (K671; Dako, Glostrup, Denmark) and a Fast Red substrate, according to the instructions given in the manual. In the negative controls, the primary antibody was omitted. The samples were then counterstained with Mayers haematoxylin (Merck D-6071, Darmstadt, Germany) for six minutes. The cover glasses were mounted with Dako fluorescence mounting medium (S3023; Dakopatts, Glostrup, Denmark). Immunostained biopsy specimens were examined microscopically, and two independent observers counted the number of positively stained (anti-HNL or anti-MPO) neutrophils in 10 crypts and tissue in high power fields. The samples were observed with a Leica DRMB microscope. Fuji 200 film was used for the colour prints.
Statistical evaluation
The Mann-Whitney U test, Wilcoxon's signed rank test, and Spearman's rank correlation test were used. All statistical calculations were performed on a personal computer using the statistical package Statistica (Stafsoft, Inc., Tulsa, Oklahoma, USA).
RESULTS
Concentrations of HNL and MPO in colorectal perfusion fluid
Control group
In healthy controls, released amounts of MPO during colorectal perfusion were below the detection limit (table 1 ▶) whereas concentrations of HNL in the sigmoidal segments were below and in the rectal segments about 4.5 times above the detection limit (table 1 ▶).
Table 1.
Concentrations of human neutrophil lipocalin (HNL) and myeloperoxidase (MPO) (median, lower and upper quartiles) in perfusion fluids from sigmoidal/rectal segments of patients with proctitis and colitis, and of controls
| Segment | HNL (μg/l) | MPO (μg/l) | |||
| Proctitis | Sigmoidal (n=8) | 13.4 (7.8–21.4)*** | † | 17.6 (<8–76.2)* | † |
| Rectal (n=7) | 245 (149–557)*** | 179 (139–581)** | |||
| Colitis | Sigmoidal (n=9) | 105 (19.6–586)*** | NS | 83.4 (20.1–414)*** | NS |
| Rectal (n=10) | 358 (55.2–430)*** | 270 (102–492)*** | |||
| Controls | Sigmoidal (n=18) | <2 | †† | <8 | |
| Rectal (n=18) | 9.2 (3.3–13.2) | <8 (<8–21.3) |
Statistical differences between the control group and patients with colitis and proctitis, as determined by the Mann-Whitney U test are indicated: *p<0.05, **p<0.01, ***p<0.001.
Statistical differences between the sigmoidal and rectal segments within the colitis and proctitis groups, as determined by Wilcoxon's signed rank test, are also indicated: †p<0.05,††p<0.01.
NS, not significant.
Patients with proctitis
In patients with proctitis, there were increased median concentrations of HNL (p<0.001) and MPO (p<0.01) in the perfusion fluid obtained from the rectal segments compared with controls (table 1 ▶). In the sigmoidal segments both HNL and MPO were increased compared with controls (p<0.001 and p<0.05, respectively).
There was a significant correlation between released amounts of HNL and MPO (r=0.83, p<0.01, n=8) in the sigmoidal segments, and a similar trend was observed in the rectal segments (r=0.75, p=0.052, n=7).
Patients with colitis
In patients with colitis, median release of HNL and MPO in the rectal segment was significantly higher (p<0.001) than median concentrations in the control group (table 1 ▶). Increased concentrations of HNL and MPO (p<0.001) were also found in perfusion fluids obtained from the sigmoidal segments compared with controls (table 1 ▶). In patients with colitis there were no significant differences between the two segments for concentrations of HNL and MPO (table 1 ▶). Significant correlations were found between released amounts of HNL and MPO (r=0.96, p<0.0001, n=9) in the sigmoidal segments but no discernible relationships were observed in the rectal segments in patients with colitis (r=0.56, p=0.090, n=10).
Localisation of HNL and MPO in biopsies from patients with colitis and proctitis by immunohistochemistry
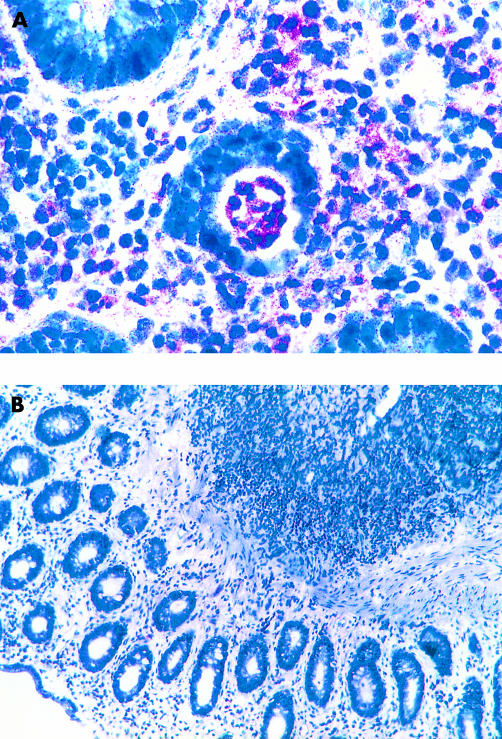
Biopsy specimens obtained from patients with proctitis and colitis undergoing colorectal perfusion showed strongly stained HNL positive neutrophils in the lamina propria, between crypt cells, and in the lumen of crypts of inflamed rectal or sigmoid tissue. In sigmoid biopsies from patients with proctitis and in biopsies from controls, very few HNL stained neutrophils were seen (fig 1A, B ▶). There was no staining of other leucocytes, or of the colonic surface epithelium cells or crypt epithelium cells.
Figure 1.
Cryosections from biopsy specimens from a patient with proctitis (A) and a healthy control (B) undergoing colorectal perfusion. (A) Neutrophils in the lamina propria and in the crypt lumen were strongly stained with anti-human neutrophil lipocalin (HNL). The colonic surface epithelium cells and crypt epithelium cells were not stained. Magnification ×470. (B) In healthy controls very few anti-HNL stained neutrophils were seen. Magnification ×120.
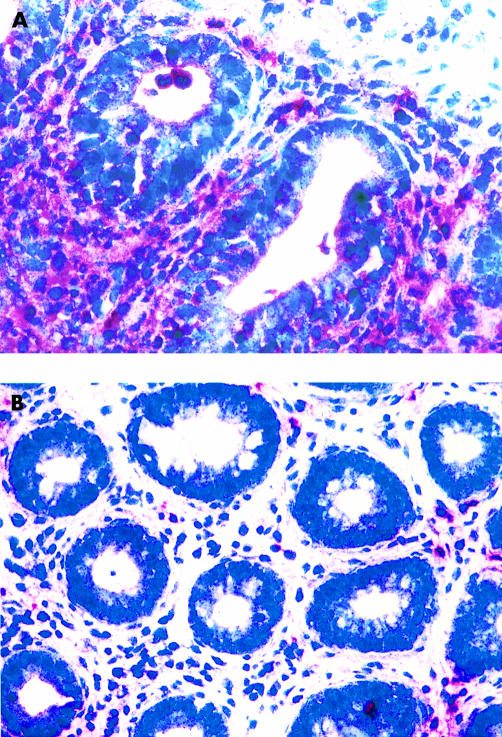
Figure 2A and B ▶ show stained MPO positive neutrophils mainly in the lamina propria but also between crypt cells and in the lumen of crypts of inflamed rectal and sigmoid tissue from patients with proctitis and colitis. In biopsies from controls and in sigmoid biopsies from patients with proctitis, only a small number of MPO stained neutrophils were observed. There was no staining of other cells in the biopsy specimens.
Figure 2.
Cryosections from biopsy specimens from a patient with colitis (A) and a healthy control (B) undergoing colorectal perfusion. (A) Neutrophils in the lamina propria and in the crypt lumen were strongly stained with anti-myeloperoxidase (MPO). The colonic surface epithelium cells and crypt epithelium cells were not stained. Magnification ×470. (B) In healthy controls very few anti-MPO stained neutrophils were seen. Magnification ×240.
Quantification of the immunohistochemistry data for HNL or MPO stained neutrophils was carried out on biopsy specimens from patients and controls undergoing colorectal perfusion. Two independent observers counted the number of positively stained (anti-HNL or anti-MPO) neutrophils in 10 crypts and tissue in high power fields. In biopsies from colitis (n=3), the range for MPO stained neutrophils was 1.2–29.1/mm and for HNL 0.7–7.0/mm whereas in patients with isolated proctitis (n=2) the range for MPO stained neutrophils was 1.2–3.9/mm and for HNL 0–3.2/mm. In specimens from controls (n=5), less than 1 neutrophil/mm was stained with MPO or HNL.
Relationship between released amounts of HNL and the cytokines GM-CSF and IL-8
Perfusion fluid concentrations of GM-CSF from patients with colitis were significantly increased in sigmoidal and rectal segments, and in rectal segments in patients with isolated proctitis, as described by Carlson and colleagues.30 Perfusion fluid concentrations of IL-8 were significantly increased in both segments in colitis and in rectal segments in patients with proctitis, as described by Raab and colleagues.24 In the perfusion fluid from sigmoidal segments obtained from patients with proctitis, released amounts of HNL were significantly correlated with released amounts of GM-CSF and IL-8 whereas in rectal segments there was only a relationship between HNL and GM-CSF (table 2 ▶). In patients with colitis there was a correlation between released amounts of HNL and GM-CSF in perfusion fluids from sigmoidal segments. In perfusion fluid from rectal segments, no discernible relationships were observed.
Table 2.
Correlations between the amounts of human neutrophil lipocalin (HNL) and the cytokines granulocyte/macrophage-colony stimulating factor (GM-CSF) and interleukin 8 (IL-8) in perfusion fluids from rectal and sigmoidal segments of patients with ulcerative proctitis and colitis
| Segment | Protein | Cytokine | Spearman's R | p Value | n | |
| Proctitis | Rectal | HNL | GM-CSF | 0.9286 | 0.0025 | 7 |
| HNL | IL-8 | 0.6786 | 0.0938 | 7 | ||
| Proctitis | Sigmoidal | HNL | GM-CSF | 0.7711 | 0.0250 | 8 |
| HNL | IL-8 | 0.8571 | 0.0065 | 8 | ||
| Colitis | Rectal | HNL | GM-CSF | 0.4303 | 0.2145 | 10 |
| HNL | IL-8 | 0.1905 | 0.6514 | 8 | ||
| Colitis | Sigmoidal | HNL | GM-CSF | 0.9160 | 0.0005 | 9 |
| HNL | IL-8 | 0.6071 | 0.1482 | 7 |
The coefficient of correlation and the significance of the correlations were calculated by Spearman's rank correlation test.
Relationship between clinical condition scores and concentrations of HNL in perfusion fluid
The amount of HNL in perfusion fluid in rectal and sigmoid segments was evaluated in relation to patient clinical scores. Significant correlations were found between released amounts of HNL and clinical score (r=0.79, p<0.03, n=7) in the rectal segments in patients with proctitis. In patients with colitis, significant correlations were found between released amounts of HNL and clinical score in both the sigmoidal (r=0.76, p<0.02, n=9) and rectal (r=0.75, p<0.01, n=10) segments, respectively.
DISCUSSION
The perfusion system used in this study is well established and standardised, allowing collection of soluble substances under steady state conditions from two physiologically closed segments of the colon and rectum.28 The technique allows monitoring of the local inflammatory process in UC. The present investigation demonstrated increased mucosal release of HNL, a new neutrophil marker protein, and MPO, during colorectal perfusion in patients with this disease.
In healthy controls, perfusion fluid concentrations of HNL and MPO in the sigmoid segments were below the limit of detection whereas HNL in rectal segments was about four times above the detection limit. Levels of HNL in rectal segments were unexpected but may be due to a higher degree of release of HNL compared with MPO, a marker of primary neutrophil granules.15
During colorectal perfusion in patients with colitis, mucosal release of HNL was, on average, increased by nearly 40-fold in rectal segments and by 55-fold in sigmoidal segments compared with controls. In patients with isolated proctitis, released amounts of HNL were about 27 times higher than in healthy controls whereas in sigmoidal segments about sevenfold higher levels were found. Our data suggest that local release of HNL in patients reflects accumulation and activation of neutrophils which are signs of ongoing inflammation. In sigmoidal segments in patients with isolated proctitis, increased release of HNL may be a sign of subclinical activation of these cells. Previous investigators have shown several fold increases in local release of MPO in rectal and sigmoidal segments in patients with colitis and in rectal segments in patients with isolated proctitis.24 These results were confirmed by us. MPO, a constituent of the primary granules of neutrophils, has been widely used as a marker for the presence and activation of neutrophil granulocytes. MPO is not unique to neutrophil granulocytes as the protein is also found in monocytes.12 However, during transformation of monocytes into macrophages in tissue, production of MPO is downregulated.31,32 Previous results indicated that HNL is a protein unique to the neutrophil.15,33 For this reason, HNL would be the optimal marker for monitoring neutrophil activity. Our studies showed that perfusate levels of HNL were significantly increased in rectal and sigmoidal segments in both colitis and proctitis. Moreover, our results demonstrated strong correlations between HNL and MPO in sigmoidal segments in patients with colitis as well as in patients with isolated proctitis, indicating the same sources of these proteins. However, the lack of correlation between HNL and MPO in rectal segments in patients with colitis may indicate that these proteins are differentially handled in this part of the inflamed gut mucosa. In biopsy specimens obtained from patients with proctitis and colitis undergoing colorectal perfusion, strongly stained HNL positive neutrophils were shown in the lamina propria, between crypt cells, and in the lumen of crypts in inflamed rectal and sigmoidal tissue. There was no staining of other cells although some released material could be seen in the specimens. These data support the nature of HNL as being a unique marker for neutrophils. This is in keeping with recent findings where HNL was shown to be a unique marker for secondary granules of the neutrophil granulocyte, demonstrated in peripheral blood cells and lung tissue by the use of flow cytometry and immunocytochemistry.16
The N terminal and four tryptic fragment amino acid sequence analysis of HNL indicated a sequence identity with NGAL.15 The cellular specificity of NGAL has recently been investigated, and northern blotting (mRNA) of a variety of tissues revealed that NGAL is mainly expressed in neutrophil precursors in bone marrow34 and in the trachea.35 Nielsen and colleagues18 also detected NGAL in epithelial cells of inflamed colon whereas a very weak signal was found in healthy colonic epithelium. These findings are in contrast with those of the present study where only neutrophils were positively stained with HNL in biopsy specimens from patients with colitis and proctitis undergoing colorectal perfusion. One reason could be that NGAL was detected using polyclonal antibodies in immunohistochemistry staining whereas we used a cocktail of six monoclonal antibodies. If colonic epithelial cells produce HNL, as well as NGAL, one would expect a higher degree of local mucosal release of HNL compared with MPO. In our study, the magnitude of local mucosal release of HNL was almost equal to that of MPO in rectal and sigmoidal segments in both proctitis and colitis. This finding corresponds to the theoretical amount of released proteins. Thus the amount of HNL has been shown to be 0.59 μg/106 neutrophils, of which 51.4±9% was released on stimulation with serum opsonised particles15 whereas MPO has been shown to be 2.83 μg/106 neutrophils36 of which only 12.7±3.5% was released after stimulation.15 These estimates suggest that equal amounts of HNL and MPO are released to the extracellular environment on stimulation despite considerable differences in their cellular contents. Hence HNL may serve as the most specific marker of neutrophil activation in UC. Nevertheless, further studies of mRNA expression of HNL, for example, in colonic epithelium would be of great interest.
The mechanism behind local accumulation and activation of neutrophils in the lamina propria may be related to neutrophil activating cytokines such as GM-CSF and IL-8. In our study, increased concentrations of both GM-CSF and IL-830 were obtained in both segments in patients with colitis, and in rectal segments in patients with proctitis. Furthermore, increased concentrations of IL-8 were obtained in sigmoidal segments in patients with proctitis. A correlation between intestinal release of IL-8 and MPO was shown, suggesting IL-8 as a possible factor in local activation and accumulation of neutrophils in UC.24 We found a significant correlation between levels of HNL and GM-CSF and IL-8, respectively, in sigmoidal segments and between HNL and GM-CSF in rectal segments in patients with proctitis. Moreover, there was a significant relationship between HNL and GM-CSF in sigmoidal segments in patients with colitis. In contrast, there was no correlation between HNL and GM-CSF or IL-8 in rectal segments in patients with colitis. These findings suggest that accumulation and activation of neutrophil granulocytes may be dependent on cytokines and chemokines such as GM-CSF and IL-8 in proctitis while other factors may be more important in this process in colitis. Possible mechanisms for tissue accumulation of neutrophils in IBD could be delay of neutrophil apoptosis under the influence of soluble mediators such as GM-CSF and G-CSF.37
We also demonstrated a correlation between clinical score and rectal and sigmoidal release of HNL in patients with colitis, and rectal release of HNL and clinical score in proctitis. These data suggest the validity of the assay regarding clinical status.
We conclude that intestinal neutrophils during colorectal perfusion in patients with UC have an increased propensity to release their granule proteins. This phenomenon reflects the fact that these cells have been primed by cytokines such as IL-8 and GM-CSF as part of the inflammatory process in the bowel. Our data suggest that GM-CSF, and to some extent IL-8, may play a role in neutrophil priming and activation in both UC and proctitis. We propose that HNL may serve as a specific marker of intestinal neutrophil activation in UC.
Acknowledgments
We are grateful to Anders Ahlander for excellent technical assistance in preparing the microscope slides. This study was supported by grants from the Swedish Medical Research Council and the Medical Faculty of Uppsala University.
Abbreviations
HNL, human neutrophil lipocalin
UC, ulcerative colitis
MPO, myeloperoxidase
GM-CSF, granulocyte/macrophage-colony stimulating factor
IL, interleukin
NGAL, neutrophil gelatinase associated lipocalin
IBD, inflammatory bowel disease
TNF-α, tumour necrosis factor α
RIA, radioimmunoassay
PBS, phosphate buffered saline
BSA, bovine serum albumin
REFERENCES
- 1.Nixon J, Ridell R. Histopathology in ulcerative colitis. In: Allan R, Keighley M, Alexander-Williams C, et al, eds. Inflammatory bowel disease. Edingburgh: Churchill Livingstone, 1990:247–85.
- 2.Olsson I, Venge P. The role of the human neutrophil in the inflammatory reaction. Allergy 1988;35:1–13. [DOI] [PubMed] [Google Scholar]
- 3.Ohlsson K, Olsson I. The neutral proteases of human granulocytes. Isolation and partial characterization of granulocyte elastase. Eur J Biochem 1974;42:519–27. [DOI] [PubMed] [Google Scholar]
- 4.Schultz J II. Biochemistry and metabolism. In: Sbarra AJ, Strauss RR, eds. In the reticuloendothelial system. A comprehensive treatise. New York: Plenum Press, 1980:231–53.
- 5.Hansen NE, Karle H, Andersen V, et al. Neutrophilic granulocytes in acute bacterial infection: Sequential studies on lysozyme, myeloperoxidase and lactoferrin. Clin Exp Immunol 1976;26:463–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Gordon LL, Douglas SD, Kay NE, et al. Modulation of neutrophil function by lysozyme potential negative feedback system of inflammation. J Clin Invest 1979;64:226–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reiter B. The biological significance of lactoferrin. Int J Tissue React 1983;5:87–96. [PubMed] [Google Scholar]
- 8.Ohlsson K, Olsson I. The neutral proteases of human granulocytes. Isolation and partial characterization of two granulocyte collagenases. Eur J Biochem 1973;36:473–81. [DOI] [PubMed] [Google Scholar]
- 9.Murphy G, Reynolds JJ, Bretz U, et al. Collagenase is component of the specific granules of human neutrophil leukocytes. Biochem J 1977;162:195–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godavac-Zimmermann J. The structural motif of beta-lactoglobulin and retinol-binding protein: a basic framework for binding and transport of small lipophilic molecules? Trends Biochem Sci 1988;13:64–6. [DOI] [PubMed] [Google Scholar]
- 11.Hraba-Renevey S, Turler H, Kress H, et al. SV 40-induced expression of mouse gene 24p3 involves a post-transcriptional mechanism. Oncogene 1989;4:601–8. [PubMed] [Google Scholar]
- 12.Olofsson T, Olsson I, Venge P, et al. Serum myeloperoxidase and lactoferrin in neutropenia. Scand J Haematol 1977;18:73–80. [DOI] [PubMed] [Google Scholar]
- 13.Kargi HA, Campbell EJ, Kuhn CD. Elastase and cathepsin G of human monocytes: Heterogeneity and subcellular localization to peroxidase-positive granules. J Histochem Cytochem 1990;38:1179–86. [DOI] [PubMed] [Google Scholar]
- 14.Venge P, Hällgren R, Stålenheim G, et al. Effects of serum and cations on the selective release of granule proteins from human neutrophils during phagocytosis. Scand J Haematol 1979;22:317–26. [DOI] [PubMed] [Google Scholar]
- 15.Xu S, Carlson M, Engström Å, et al. Purification and characterization of a human neutrophil liopcalin (HNL) from secondary granules of human neutrophils. Scand J Clin Lab Invest 1994;54:365–76. [DOI] [PubMed] [Google Scholar]
- 16.Sevéus L, Amin K, Peterson CGB, et al. Human neutrophil lipocalin (HNL) is a specific granule constituent of the neutrophil granulocytes. Studies in bronchial and lung parenchymal tissue and peripheral blood cells. Histochem Cell Biol 1997;107:423–32. [DOI] [PubMed] [Google Scholar]
- 17.Kjeldsen L, Johnsen AH, Sengelov H, et al. Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J Biol Chem 1993;268:10425–32. [PubMed] [Google Scholar]
- 18.Nielsen BS, Borregaard N, Bundgaard JR, et al. Induction of NGAL synthesis in epithelial cells of human colorectal neoplasia and inflammatory disease. Gut 1996;38:414–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nielsen OH, Gionchetti P, Ainsworth M, et al. Rectal dialysate and fecal concentrations of neutrophil gelatinase-associated lipocalin, interleukin-8, and tumor necrosis factor-α in ulcerative colitis. Am J Gastroenterol 2000;94:2923–8. [DOI] [PubMed] [Google Scholar]
- 20.Baggiolini M, Walz A, Kunkel SL. Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J Clin Invest 1989;84:1045–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seitz M, Dewald B, Gerber N, et al. Enhanced production of neutrophil-activating peptide-1/interleukin-8 in rheumatoid arthritis. J Clin Invest 1991;87:463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ina K, Kusugami K, Yamaguchi T, et al. Mucosal interleukin-8 is involved in neutrophil migration and binding to extracellular matrix in inflammatory bowel disease. Am J Gastroenterol 1997;92:1342–6. [PubMed] [Google Scholar]
- 23.Nielsen OH, Rudiger N, Gaustadnes M, et al. Intestinal interleukin-8 concentrations and gene expressen in inflammatory bowel disease. Scand J Gastroenterol 1997;32:1028–34. [DOI] [PubMed] [Google Scholar]
- 24.Raab Y, Gerdin B, Ahlstedt S, et al. Neutrophil mucosal involvement is accompained by enhanced local production of interleukin-8 in ulcerative colitis. Gut 1993;34:1203–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uhr MR, Schaufelberger HD, Hildebrand P, et al. Thrombocytes express functional cytokine receptors in patients with Crohn's disease and ulcerative colitis. Schweiz Med Wochenschr 1995;125:970–4. [PubMed] [Google Scholar]
- 26.Bergenholt S, Claesson MH. Splenic T helper cell type 1 cytokine profile and extramedullary haematopoiesis in severe combined immunodeficient (scid) mice with inflammatory bowel disease (IBD). Clin Exp Immunol 1998;111:166–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garland C, Lilienfeld A, Mendeloff A, et al. Incidence rates of ulcerative colitis and Crohn's disease in fifteen areas of the United States. Gastroenterology 1981;81:1115–24. [PubMed] [Google Scholar]
- 28.Raab Y, Hällgren R, Knutson L, et al. A technique for segmental rectal and colonic perfusion in humans. Am J Gastroenterol 1992;87:1453–9. [PubMed] [Google Scholar]
- 29.Xu S, Peterson CGB, Carlson M, et al. The development of an assay for human neutrophil lipocalin (HNL)—to be used as a specific marker of neutrophil activity in vivo and vitro. J Immunol Methods 1994;171:245–52. [DOI] [PubMed] [Google Scholar]
- 30.Carlson M, Raab Y, Peterson C, et al. Increased intraluminal release of eosinophil granule proteins EPO, ECP, EPX and cytokines in ulcerative colitis and proctitis in segmental perfusion. Am J Gastroenterol 1999;94:1876–83. [DOI] [PubMed] [Google Scholar]
- 31.Nichols BA, Ford Bainton D, Farquhar MG. Differentiation of monocytes. Origin, nature, and fate of their azurophil granules. J Cell Biol 1971;50:498–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sugiyama S, Okada Y, Sukhova GK, et al. Macrophage myeloperoxidase regulation by granulocyte macrophage colony-stimulating factor in human atherosclerosis and implications in acute coronary syndromes. Am J Pathol 2001;158:879–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xu S, Pauksens K, Venge P. Serum measurements of human neutrophil lipocalin (HNL) discriminate between acute bacterial and viral infections. Scand J Clin Lab Invest 1995;55:125–31. [DOI] [PubMed] [Google Scholar]
- 34.Bundgaard JR, Sengelov H, Borregaard N, et al. Molecular cloning and expression of a cDNA encoding NGAL: a lipcalin expressed in human neutrophils. Biochem Biophys Res Commun 1994;202:1468–75. [DOI] [PubMed] [Google Scholar]
- 35.Cowland JB, Borregaard N. Molecular characterization and pattern of tissue expression of the gene for neutrophil gelatinase-associated lipocalin from humans. Genomics 1997;45:17–23. [DOI] [PubMed] [Google Scholar]
- 36.Öberg G, Lindmark G, Moberg L, et al. The peroxidase activity and cellular content of granule proteins in PMN during pregnancy. Br J Haematol 1983;55:701–8. [DOI] [PubMed] [Google Scholar]
- 37.Ina K, Kusugami K, Hosokawa T, et al. Increased mucosal production of granulocyte colony-stimulating factors is related to a delay in neutrophil apoptosis in inflammatory bowel disease. J Gastroenterol Hepatol 1999;14:46–53. [DOI] [PubMed] [Google Scholar]