Abstract
Background: Prevalence studies of faecal incontinence in the general population are rare and the impact of faecal incontinence on quality of life has not been previously addressed.
Aims: To establish the prevalence of faecal incontinence in adults in terms of frequency of leakage, degree of soiling, and level of impact on quality of life.
Methods: In a cross sectional postal survey, 15 904 adults aged 40 years or more (excluding residents of nursing and residential homes) were selected randomly by household from the Leicestershire Health Authority patient register. Participants were asked to complete a confidential health questionnaire. Major faecal incontinence was defined as soiling of underwear or worse with a frequency of several times a month or more. Respondents were also asked if bowel symptoms had an impact on their quality of life.
Results: From a total sample of 10 116 respondents, 1.4% reported major faecal incontinence and 0.7% major faecal incontinence with bowel symptoms that had an impact on quality of life. Major faecal incontinence was significantly associated with a lot of impact on quality of life (odds ratio 12.4, 95% confidence interval 7.5–20.6). Incontinence was more prevalent and more severe in older people but there was no significant difference between men and women.
Conclusions: This study has confirmed that faecal incontinence is a fairly common symptom, particularly in older people. Faecal incontinence in men has received little attention in the past and the results from this study indicate that it is as much of a problem in men as it is in women while the level of unmet need in this group is high. Estimates of need for health care for this symptom should be multidimensional and assess both the severity of symptoms and the impact it has on quality of life.
Keywords: faecal incontinence, quality of life, epidemiology
Prevalence studies of faecal incontinence in the general population are rare.1 Among younger age groups (<65 years), the prevalence of faecal incontinence has been estimated at 0.7%2 and 0.9%.3 In older people (≥60 years), where most of the research in this area has concentrated, prevalence estimates are much higher, ranging between 3.1% and 8.2%, although most studies have been based on small sample sizes.4–8 There is a strong association between increasing age and faecal incontinence, with the very elderly (85 years or more) particularly at risk, as are frail older people living in long term care institutions.9
Recently, published work has suggested that females are at greater risk of faecal incontinence and that the cause of this is primarily related to childbirth.10,11 Supportive data are inconclusive however. Three studies in older subjects (65 years or more) reported no difference between men and women,4,8,12 one a higher prevalence in men,5 and another a higher prevalence in women.7 General population surveys have either assessed the prevalence of anal incontinence (that is, incontinence of solid or liquid stool or flatulence) or faecal incontinence only (that is, incontinence of solid or liquid stools only). Thus Nelson and colleagues2 found that female sex was an independent risk factor for anal incontinence whereas Thomas and colleagues3 found a preponderance of faecal incontinence in men as opposed to women aged 15–64 years.
Faecal incontinence may not be life threatening and people may only seek help when the symptoms become disabling or bothersome. Although faecal incontinence must be one of the most potentially embarrassing symptoms to experience, its impact on well being, daily activities, and relationships has not been addressed in epidemiological studies. Investigations of the prevalence of disabling faecal incontinence may provide better estimates of the need for services than studies limited to symptoms only.
The aim of this study was to estimate the prevalence of faecal incontinence in adults living in the community in terms of frequency of leakage and degree of soiling, and the level of impact on quality of life.
METHOD
A postal questionnaire was sent to 15 904 subjects aged 40 years or more. The sample was selected randomly by household from the Leicestershire Health Authority patient register, with 137 (90%) general practices in Leicestershire and Rutland taking part in the study. Non-responders were sent a second questionnaire two weeks after the first mailing. Letters of approach were from the individual's general practitioner or a member of the research team, depending on the preference of each participating general practice. Those living in institutional settings (that is, residential or nursing homes) were excluded from the sampling frame. The postal questionnaire included questions on general health, urinary and bowel symptoms, impact of symptoms on quality of life, and demographic characteristics. Respondents were asked to report on symptoms they had experienced in the past 12 months.
A variety of indicators have been used to measure the severity of faecal incontinence (that is, the frequency of leakage,3 degree of soiling,12 consistency of stools leaked,2 and use of pads4). The specific questions on faecal incontinence in the questionnaire related to the frequency of leakage and degree of soiling (see table 1 ▶). These two measures have been identified as essential to any grading system to assess the severity of faecal incontinence.13 There is no agreed threshold to identify clinically significant faecal incontinence. Leakage, self reported as any,5,6,14 yearly,2,7 monthly,3,15 and weekly,4,8 have all been set as thresholds for case definition. Thomas and colleagues3 found that a definition of faecal incontinence as leakage occurring twice a month or more led to an overestimate of prevalence from a postal survey because many respondents were referring to minor staining associated with constipation or haemorrhoids. Consequently, in this study, major faecal incontinence was defined as soiling of underwear, outer clothing, furnishing, or bedding several times a month or more often. Minor incontinence was defined as staining of underwear several times a month or more often. It is possible that the definition of minor incontinence includes those subjects less fastidious about their personal hygiene. Our definition of rare or no incontinence will include those who leak several times a year or less, regardless of the extent of soiling. Infrequent leakage is suggestive of bouts of illness rather than a chronic condition.
Table 1.
Questions on faecal incontinence and impact of bowel symptoms in the postal questionnaire
| Do you ever leak from your bowels when you don't mean to? (During the day or night) | |
| Continuously | □ |
| Several times a day | □ |
| Several times a week | □ |
| Several times a month | □ |
| Several times a year | □ |
| Never/rarely | □ |
| When you leak from your bowels when you don't mean to is there usually: | |
| Soiling of furnishing or bedding | □ |
| Soiling of outer clothing | □ |
| Soiling of underwear | □ |
| Minor staining of underwear | □ |
| Not applicable (NA) | □ |
| Do your bowel symptoms: | |||
| A lot | A little | Not at all/NA | |
| Bother you? | □ | □ | □ |
| Cause you any physical discomfort? | □ | □ | □ |
| Interfere with your daily activities? | □ | □ | □ |
| Interfere with your social life? | □ | □ | □ |
| Affect your relationships with other people? | □ | □ | □ |
| Upset or distress you? | □ | □ | □ |
| Affect your sleep? | □ | □ | □ |
| Affect your overall quality of life? | □ | □ | □ |
Respondents were also asked about how much of an impact their bowel symptoms had on a number of aspects of quality of life (see table 1 ▶). The questions refer to “bowel symptoms” generally rather than specific symptoms because the questionnaire included questions on a number of bowel symptoms and not just incontinence. If respondents indicated “a lot” of impact on any one of these items, their bowel symptoms were regarded as having a lot of impact on their life. If respondents reported “a little” impact on these items it is unlikely they would perceive themselves to have a serious problem and it would be difficult to assess improvements in quality of life as a result of treatment. Our approach to the measurement of need is based on the concepts of professionally defined need and personally defined or felt need. The former is commonly related to specified symptoms thought to be significant for health. Felt need is a concept we define in three main ways, (i) generally, using words such as “bothersome”, “problematic”, “troublesome”, and “overall quality of life”, (ii) specifically, using the effects on important domains of life including activities, feelings, well being, and relationships, and (iii) practically, in terms of feeling a desire for help or treatment.
In recent years the term “impact” has been used to summarise the general and specific elements. “Impact” suggests disability (meaning a symptom that restricts function). Thus in this study we refer interchangeably to impact and disability as indicators of felt need. Multivariate logistic regression analyses were used to assess the contribution of faecal incontinence to the overall impact of respondent's bowel symptoms while adjusting for all other bowel symptoms, age, and sex. Respondents were also asked if they felt they needed help for their bowel symptoms.
RESULTS
Of the 15 904 questionnaires posted, 1304 (8.2%) were excluded because the subject no longer lived at the address, had moved to a residential or nursing home, or was deceased. Of the remaining 14 600 questionnaires mailed, 10 226 were returned (70%) and of these 10 116 (99%) could be analysed. Response rates were generally lower in men (67.8%) than in women (73.1%). The age, sex, and ethnic group structure of the sample was similar to the population of Leicestershire as a whole (table 2 ▶).16
Table 2.
Demographic and health characteristics of the sample and the Leicestershire population
| Variable | Respondents (%) | Population (%) |
| Age (y) | ||
| 40–49 | 2781 (27.5) | 119 003 (31.2) |
| 50–59 | 2564 (25.3) | 90 044 (23.6) |
| 60–69 | 2226 (22.0) | 83 784 (22.0) |
| 70–79 | 1755 (17.3) | 58 273 (15.3) |
| 80+ | 790 (7.8) | 30 276 (7.9) |
| Total | 10 116 (100) | 381 380 (100) |
| Sex | ||
| Female | 5483 (54.2) | 201 394 (52.8) |
| Male | 4633 (45.8) | 179 986 (47.2) |
| Total | 10 116 (100) | 381 380 (100) |
| Ethnicity (>39years) | ||
| White | 9363 (93.2) | 356 850 (93.6) |
| South Asian | 569 (5.7) | 20 247 ( 5.3) |
| Other | 115 (1.1) | 4283 ( 1.1) |
| Total | 10 047 (100) | 381 380 (100) |
Values are given as n (%).
Missing data are not included in column totals. Population estimates for Leicestershire are taken from the 1991 Census.
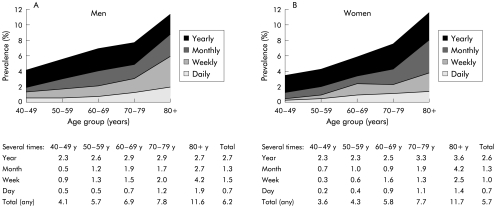
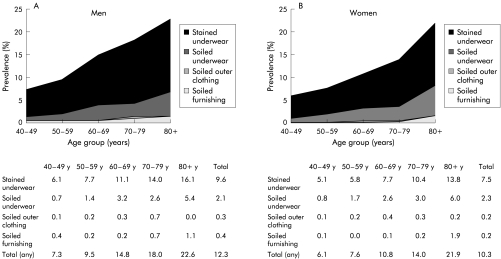
The prevalence of faecal incontinence, in terms of the frequency of leakage and degree of soiling, are shown in figs 1 and 2 ▶ ▶. Overall, the prevalence of monthly or more leakage was 3.3% and the prevalence of soiling was 2.7%. The prevalence of incontinence increased with age and the oldest age group (80+ years) reported more frequent leakage and greater soiling than younger age groups. The frequency of leakage did not differ between men and women at any level of severity (3.6% and 3.1% reported monthly or more frequent leakage, respectively). The proportions reporting soiling of underwear or worse was the same (2.7%) but more men than women reported staining of underwear (9.6% and 7.5%, respectively). In total, 1.4% of the sample reported major faecal incontinence and 1.7% minor. Major incontinence was reported by 0.9% of adults aged 40–64 years and by 2.3% of adults aged 65 years.
Figure 1.
Prevalence (%) of faecal incontinence by frequency of leakage (yearly, monthly, weekly, or daily) in men (A) and women (B).
Figure 2.
Prevalence (%) of faecal incontinence by degree of soiling (stained underwear, soiled underwear, soiled outer clothing, or soiled furnishing) in men (A) and women (B).
Just over half of those with major faecal incontinence (51.7%) reported that their bowel symptoms had a lot of impact on their life (table 3 ▶). Those with minor faecal incontinence were less likely to report a lot of impact (16.0%), and only 2.9% of those with rare or no incontinence reported an impact on quality of life. Faecal incontinence was still significantly associated with a lot of impact on life even after adjusting for other bowel symptoms (table 4 ▶). Reporting of a lot of impact was significantly greater in both those with major (odds ratio 12.4, 95% confidence interval 7.5–20.6) and minor (2.5, 1.4–4.6) faecal incontinence compared with those with rare or no faecal incontinence. The only bowel symptom not significantly associated with a lot of impact in the multivariate model was having to strain when having a bowel movement.
Table 3.
Prevalence of faecal incontinence and impact on life in adults
| A lot of impact (%) | None or a little impact only (%) | Total (%) | |
| Major faecal incontinence | 60 (51.7) | 56 (48.3) | 116 (100.0) |
| Minor faecal incontinence | 23 (16.0) | 121 (84.0) | 144 (100.0) |
| No faecal incontinence | 244 (2.9) | 8059 (97.1) | 8303 (100.0) |
| Total | 327 (3.8) | 8236 (96.2) | 8563 (100.0) |
Table 4.
Bowel symptoms associated with a lot of impact on life (adjusting for age and sex)
| Odds ratio (95% confidence interval) | ||
| Univariate | Multivariate | |
| Faecal incontinence | ||
| No/rare incontinence | 1.00 | 1.00 |
| Minor incontinence | 6.35 (3.97–10.15) | 2.55 (1.41–4.59) |
| Major incontinence | 34.37 (23.06–51.21) | 12.41 (7.46–20.65) |
| Pain in bladder or lower abdomen | ||
| Never | 1.00 | 1.00 |
| Most of the time/sometimes/occasionally | 21.63 (15.19–30.80) | 5.87 (3.90–8.83) |
| Difficulty in delaying a bowel movement | ||
| Never | 1.00 | 1.00 |
| Most of the time/sometimes/occasionally | 6.23 (4.71–8.25) | 2.18 (1.56–3.04) |
| Has to strain when having a bowel movement | ||
| Never | 1.00 | |
| Most of the time/sometimes/occasionally | 3.17 (2.42–4.16) | |
| Feels pain when having a bowel movement | ||
| Never | 1.00 | 1.00 |
| Most of the time/sometimes/occasionally | 11.57 (8.93–14.99) | 2.70 (1.94–3.76) |
| Consistency of stools | ||
| Firm or soft | 1.00 | 1.00 |
| Hard | 6.72 (5.23–8.63) | 4.39 (3.15–6.13) |
| Watery | 18.79 (13.20–26.75) | 5.06 (3.15–8.15) |
| Frequency of bowel movement | ||
| More than 3 times a day | 20.56 (14.71–28.76) | 6.30 (4.07–9.78) |
| 1–3 times a day | 1.00 | 1.00 |
| Once or more a week | 2.06 (1.55–2.73) | 1.14 (0.80–1.63) |
| Less than once a week | 8.23 (4.79–14.13) | 3.17 (1.48–6.77) |
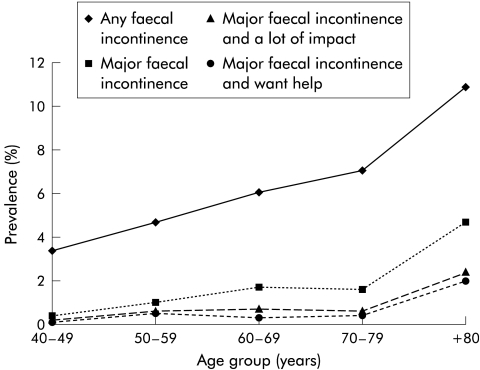
The prevalence of major faecal incontinence with a lot of impact on quality of life in the total sample was 0.7% and nearly two thirds (64.9%) of this group said they wanted help with symptoms (0.4% of the total sample). There appears to be reasonable comparability between the prevalence of major faecal incontinence with a lot of impact and those with major incontinence requesting help for their symptoms (fig 3 ▶). The level of major incontinence and request for help was low at 0.1% for adults in their 40s, fairly stable between the ages of 50 and 79 years at 0.4%, and increased significantly to 2.0% for the older age group (80 years or more).
Figure 3.
Prevalence (%) of faecal incontinence by severity, disability, and request for help.
DISCUSSION
In total, 1.4% of the sample reported major faecal incontinence (0.9% of adults aged 40–64 years and 2.3% of adults aged 65 years). Faecal incontinence was found to be a considerable problem for older people in that it was more prevalent and severe and more likely to have an impact on quality of life. Our estimates were lower than those found in previous studies. This is probably due to the use of a more strict definition of faecal incontinence which takes into account both frequency and amount of leakage. Setting thresholds to identify clinically significant faecal incontinence is somewhat arbitrary. Standardised scales and agreed thresholds are needed to allow comparison between studies and more accurate estimates of the need for health care. Symptom based estimates probably overestimate the level of need for services in the community. It may be more efficient to focus services on those who report clinically significant symptoms that have an impact on quality of life.
We found no sex difference in the prevalence of faecal incontinence. Although faecal incontinence is often presented as a women's problem, the extent to which it persists or deteriorates in later life is unclear.17–19 Although women may predominate in specialist clinics, this may reflect differences in consultation behaviour and referral patterns rather than the actual prevalence of faecal incontinence in the general population. Faecal incontinence in men in the general population has received little attention and the results from the study indicate that the level of unmet need for this group is high.
Most of the epidemiological research on faecal incontinence has focused on symptoms and little is known about the impact of these on an individual's life. Just over one half of those with major incontinence said bowel symptoms had “a lot” of impact on their life (0.7% of the sample). However, impact refers to a number of bowel symptoms of which faecal incontinence is just one, and it is possible that the reported levels of impact may be due to a combination of symptoms, such as irritable bowel, constipation, or diarrhoea. In future work, it may be advisable to investigate symptoms groups and their impact on quality of life rather than symptoms in isolation.
It is important that the personal and social consequences of incontinence are addressed during treatment and that patients are advised on how best to manage these symptoms when a cure is not always achieved. Indeed, the development of quality of life measures specific to faecal incontinence has been reported more recently.20,21 Patients attending specialist clinics may represent those with the most severe forms of faecal incontinence. Alternatively, they may represent those experiencing difficulties managing their symptoms or those with better access to health care services. Prevalence data are useful for assessing how representative clinical samples are of the general population as a whole with these types of symptoms and where high levels of unmet need exist.
Incontinence is often cited as one of the main causes of admission to residential care although the evidence to substantiate this claim is limited.22–24 Major faecal incontinence and its associated impact increased in those aged 70 years and over, although there were smaller numbers in this age group. Promotion of continence in primary care settings could prevent disability in later life and extend the period of life that is free of illness and incapacity. Recent Department of Health guidelines on continence services for faecal and urinary incontinence reiterate the importance of raising awareness in this area of clinical practice so that those with incontinence receive a prompt high quality and comprehensive service.25 We estimate that 0.7% of adults aged 40 years or more living at home in the UK experience major faecal incontinence and other bowel symptoms which have a lot of impact on quality of life. These values could be used to help develop local targets to ensure that those with continence problems are properly identified, assessed, and given the treatment they need.
The content validity of the questionnaire appeared appropriate, as pilot work suggested that respondents found the questions clear and easy to complete and in the main study there were only 3% missing data on the faecal incontinence questions. A postal questionnaire, completed in the privacy of the respondent's own home and in confidence, may be a more acceptable approach to assess the prevalence of these types of symptoms than structured interviews where subjects are more likely to complain about the more acceptable symptom of diarrhoea.26
In conclusion, this study has shown that faecal incontinence is a common symptom in men as well as in women and particularly so in older subjects. Just over one half of those with major faecal incontinence reported that bowel symptoms had a lot of impact on quality of life and about a third felt that they needed help with these symptoms.
Acknowledgments
We thank the general practitioners of Leicestershire and Rutland who gave their support to the study; all members of the Leicestershire MRC Incontinence Study Team, in particular Peter Marsh, Chris Sanders, and Toby Richmond, who provided computer support and Lesley Harris and Jennie Lucus who supervised administration of the postal survey; Fiona Mensah (statistician), Nigel Smith (researcher), and Jeremy Jones (investigator) who have since left the study but were involved in earlier drafts of the paper; and respondents to the survey who returned completed postal questionnaires. Mr PJ Lunniss, Dr SM Scott, and Dr James Barrett read drafts of this paper and advised on definitions of faecal incontinence and their comments were gratefully received. We would like to thank the Medical Research Council for funding this project.
REFERENCES
- 1.Enck P, Bielefeldt K, Rathmann W, et al. Epidemiology of faecal incontinence in selected patient groups. Int J Colorect Dis 1991;6:143–6. [DOI] [PubMed] [Google Scholar]
- 2.Nelson R, Norton N, Cautley E, et al. Community-based prevalence of anal incontinence. JAMA 1995;274:559–61. [PubMed] [Google Scholar]
- 3.Thomas TM, Egan M, Walgrove A, et al. The prevalence of faecal and double incontinence. Community Med 1984;6:216–20. [DOI] [PubMed] [Google Scholar]
- 4.Talley NJ, O'Keefe EA, Zinsmeister AR, et al. Prevalence of gastrointestinal symptoms in the elderly: a population-based study. Gastroenterolgy 1992;102:895–901. [DOI] [PubMed] [Google Scholar]
- 5.Campbell AJ, Reinken J, McCosh L. Incontinence in the elderly: prevalence and prognosis. Age Ageing 1985;14:65–70. [DOI] [PubMed] [Google Scholar]
- 6.Kok ALM, Voorhorst FJ, Burger CW, et al. Urinary and faecal incontinence in community-residing elderly women. Age Ageing 1992;21:211–15. [DOI] [PubMed] [Google Scholar]
- 7.Hellstom L, Ekelund P, Milsom I, et al. The influence of dementia on the prevalence of urinary and faecal incontinence in 85-year-old men and women. Arch Gerontol Geriatr 1994;91:11–20. [DOI] [PubMed] [Google Scholar]
- 8.O'Keefe EA, Talley NJ, Zinsmeister AR, et al. Bowel disorders impair functional status and quality of life in the elderly: a population-based study. J Gerontol 1995;50A:M184–9. [DOI] [PubMed] [Google Scholar]
- 9.Peet S, Castleden CM, McGrother CW. Prevalence of urinary and faecal incontinence in hospitals and residential and nursing homes for older people. BMJ 1995;311:1063–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rieger N, Wattchow D. The effect of vaginal delivery on anal function. Aust N Z J Surg 1999;69:172–7. [DOI] [PubMed] [Google Scholar]
- 11.Fynes M, Donnelly V, Behan M, et al. Effect of second vaginal delivery on anorectal physiology and faecal continence: a prospective study. Lancet 1999;354:983–6. [DOI] [PubMed] [Google Scholar]
- 12.Nakanishi N. Urinary and faecal incontinence in a community-residing older population in Japan. J Am Geriatr Soc 1997;45:215–19. [DOI] [PubMed] [Google Scholar]
- 13.Vaizey CJ, Carapeti E, Cahill JA, et al. Prospective comparison of faecal incontinence grading systems. Gut 1999;44:77–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lagaay AM, Van Asperen IA, Hijmans W. The prevalence of morbidity in the oldest old, aged 85 and over: a population-based survey in Leiden, the Netherlands. Arch Gerontol Geriatr 1992;15:115–31. [DOI] [PubMed] [Google Scholar]
- 15.Wetle T, Scherr P, Branch LG, et al. Difficulty with holding urine among older persons in a geographically defined community: prevalence and correlates. J Am Geriatr Soc 1995;43:349–55. [DOI] [PubMed] [Google Scholar]
- 16.Office of Population Censuses and Surveys. 1991 Census County Report: Leicestershire (Part 1). London: HMSO, 1992.
- 17.MacArthur C, Bick DE, Keighley MRB. Faecal incontinence after childbirth. Br J Obstet Gynaecol 1997;104:46–50. [DOI] [PubMed] [Google Scholar]
- 18.Groutz A, Fait G, Lessing JB, et al. Incidence and obstetric risk factors of post partum anal incontinence. Scand J Gastroenterol 1999;3:315–18. [DOI] [PubMed] [Google Scholar]
- 19.Zetterstrom JP, Lopez A, Anzen B, et al. Anal incontinence after vaginal delivery: a prospective study in primiparous women. B J Obstet Gynaecol 1999;106:324–30. [DOI] [PubMed] [Google Scholar]
- 20.Rockwood TH, Church JM, Fleshman JW, et al. Fecal incontinence quality of life scale: quality of life instrument for patients with fecal incontinence. Dis Colon Rectum 2000;43:9–17. [DOI] [PubMed] [Google Scholar]
- 21.Bugg G, Hosker G, Kiff E. Prevalence of faecal incontinence among women with urinary incontinence. Br J Obstet Gynaecol 1999; 106;1233–4. [DOI] [PubMed] [Google Scholar]
- 22.Tilvis RS, Hakala S, Valvanne J, et al. Urinary incontinence as a predictor of death and institutionalisation in a general aged population. Arch Gerontol Geriatr 1995;21:307–15. [DOI] [PubMed] [Google Scholar]
- 23.Tsuji I, Whalen S, Finucane TE. Predictors of nursing home placement in community-based long-term care. J Am Geriatr Soc 1995;43:761–6. [DOI] [PubMed] [Google Scholar]
- 24.Sanford JRA. Tolerance of debility in elderly dependents by supporters at home: its significance for hospital practice. BMJ 1975;3:471–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Department of Health. Good practice in continence services. London: Department of Health, 2000.
- 26.Leigh RJ, Turnberg LA. Faecal incontinence: the unvoiced symptom. Lancet 1982;1:1349–51. [DOI] [PubMed] [Google Scholar]