Abstract
Background: Although overall admission rates for peptic ulcer in England declined from the 1950s up until the mid 1980s, perforations among older women increased, possibly due to increasing use of non-steroidal anti-inflammatory drugs (NSAID). Since then, proton pump inhibitors, antibiotic treatment for Helicobacter pylori, low dose aspirin, and selective serotonin reuptake inhibitors (SSRI) have been introduced
Aims: To determine time trends for hospital admissions for peptic ulcer from 1989 to 1999 (England), mortality from 1958 to 1998 (England and Wales), and prescriptions for ulcer healing drugs, aspirin, NSAID, oral anticoagulants, and SSRI from 1990 to 1999 (England).
Methods: Hospital episode statistics for admissions and mortality were obtained from the Office of National Statistics: community prescription data from Statistics Division 1E of the Department of Health.
Results: Between 1989/90 and 1998/99, there was a marked rise in admissions for haemorrhage in older patients, particularly from duodenal ulcer. Perforations from gastric ulcer declined but perforations from duodenal ulcer increased among men at older ages. Since the mid 1980s mortality has declined in all age groups except for older women with duodenal ulcer. The number of prescriptions for histamine H2 receptor antagonists remained constant but those for proton pump inhibitors increased by 5000%, aspirin 75mg by 460%, oral anticoagulants by 200%, and NSAID by 13% between 1990 and 1999. Since the introduction of SSRI in 1991, prescriptions have increased 15-fold.
Conclusions: Admission rates for gastric and duodenal ulcer haemorrhage and duodenal ulcer, but not gastric ulcer perforation, increased among older subjects, over a time when prescriptions for proton pump inhibitors, low dose aspirin, oral anticoagulants, and SSRI increased.
Keywords: peptic ulcer, gastric ulcer, duodenal ulcer, peptic ulcer haemorrhage, peptic ulcer perforation, aspirin
The story of peptic ulcer over the last 200 years has been one of profound changes in frequency and clinical presentation. In 1857, Brinton described gastric ulcer as a disease of young women1: duodenal ulcer seemed to be rare.2 In the beginning of the 20th century however the prevalence of duodenal ulcer increased to several times that of gastric ulcer before starting to fall in the second half of the century.2 Between the 1950s and 1980s, hospital admissions and mortality from peptic ulcer declined in Britain for most age groups.3–5 In contrast with this general trend, admissions for perforated peptic ulcer and mortality from duodenal ulcer increased among older women in the 1970s and 1980s.5–7 Similar patterns have been noted in other Western countries8–10 although a recent Danish study showed that hospitalisation and mortality from peptic ulcer complications have increased, especially among the elderly.11 This general decline in hospital admission rates and mortality from peptic ulcer has been attributed to a reduced prevalence of Helicobacter pylori infection,10 and a recent review stated that: “Peptic ulcer seems to be on the way out”.9 The rise in mortality and admissions among older women in the 1970s and 1980s has been attributed to increased prescribing of non-steroidal anti-inflammatory drugs (NSAID), the other major cause of peptic ulcer, commonly used in older subjects.5,6,12
The introduction of effective antisecretory treatment with histamine H2 receptor antagonists in the mid 1970s was associated with a reduction in elective surgery for peptic ulcer disease.6,7,13 Since then two other major advances in peptic ulcer treatment have been introduced: proton pump inhibitors and antibiotic treatment to eradicate H pylori. A link has also been proposed between serotonin reuptake inhibitors (SSRI) and upper gastrointestinal bleeding.14 We have therefore examined the statistics for mortality, admissions, operations, and drug prescribing relating to peptic ulcer, to determine the latest time trends of these indices of peptic ulcer disease.
METHODS
Hospital admission rates (finished consultant episodes)
Although most patients with uncomplicated peptic ulcer would probably self medicate or be treated by their general practitioner, patients with ulcer complications, in particular perforation and severe haemorrhage, are admitted to hospital. Hospital admission rates can therefore be used as an index of peptic ulcer frequency although it is uncertain if the proportion of ulcers which perforate or bleed is constant while the threshold at which hospital admission occurs may vary according to the prevailing medical practice at the time.2
The Department of Health provided hospital episode statistics for England for 1989/90–1998/9. For the period 1989/90–1994/5, we identified finished consultant episodes with a primary diagnosis of ICD 9 codes 531, 532, 533, and 534. For the period 1995/6–1998/9 when ICD 10 codes were in use, we identified finished consultant episodes with a primary diagnosis of codes K25, K26, K27, and K28. Average annual age standardised rates for 1989/90–1991/2, 1992/3–1995/6, and 1996/7–1998/9 were calculated. These were standardised against the European standard population using the mid year population estimates for each year and 10 year age bands. Trends for finished consultant episodes in the age groups 25–44 years, 45–64 years, 65–74 years, and 75 years and over were examined. Day cases were excluded. Data for peptic ulcer site unspecified (ICD 9 code 533) was combined with gastric ulcer (ICD 9 code 531) to allow comparison with mortality rates. Peptic ulcer site unspecified made up less than 10% of the gastric ulcer total at the beginning of the period and less than 5% at the end, probably reflecting improvement in the accuracy of coding. Gastrojejunal ulcers (ICD 9 534 and ICD 10 K28) make up approximately 1% of all peptic ulcers and are not considered further in this analysis. We also studied admission rates for perforation and haemorrhage. Ulcers which both perforated and haemorrhaged were grouped with those which just perforated.
Finished consultant episodes relating to operations performed for peptic ulcer disease (OPCS 4 codes A27 (extracranial vagotomy), G28 (partial excision of stomach), G35 (operations on ulcer of stomach) and G52 (operations on ulcer of duodenum)) were examined for the period 1990/91–1998/99.
Mortality rates
Peptic ulcer is a disease of low mortality and most deaths occur as a result of complications in elderly patients with significant comorbidity. Mortality for peptic ulcer is therefore influenced not only by the frequency of ulcer disease but also by its severity, as well as the effectiveness of medical treatment.2
Deaths due to ICD 7 codes 540, 541, and 542 (1958–1967) and deaths due to ICD 8 and 9 codes 531, 532, 533, and 534 (1968–1998) were identified for England and Wales. These were standardised against the European standardised population using the mid year population estimates for the year and 10 year age bands. Trends for mortality in the age groups 45–64 years and 65 years and over were examined. Data for peptic ulcer site unspecified (ICD 8 and 9 codes 533) were combined with gastric ulcer (ICD 8 and 9 codes 531) to correspond with gastric ulcer and peptic ulcer site unspecified (ICD 7 code 540).
Prescribing
To explore the possible impact of drug prescribing on mortality and hospital admissions, we analysed information on the number of items dispensed in the community between 1990 and 1999, supplied by Statistics Division 1E of the Department of Health. Values for 1990 are based on fees and on a sample of 1 in 200 prescriptions dispensed by community pharmacists and appliance contractors only. Values from 1991 onwards are from the Prescription Cost Analysis system and are based on a full analysis of all prescriptions dispensed in the community—that is, by community pharmacists and appliance contractors, dispensing doctors, and prescriptions submitted by prescribing doctors for items personally administered in England. The data do not cover drugs dispensed in hospital or private prescriptions but most prescribing for chronic diseases in the UK is carried out by general practitioners and is picked up by the Prescription Cost Analysis system.
Information was provided for the number of items dispensed for ulcer healing drugs (BNF section 1.3), NSAID (BNF section 10.1.1), aspirin (BNF section 2.9 and 4.7.1), oral anticoagulants (BNF section 2.8.2), and SSRI (BNF section 4.3.3).
RESULTS
Hospital admissions
Finished consultant episodes for gastric ulcer and peptic ulcer not otherwise specified (England 1989/90–1998/9)
Overall, there was a slight rise in admission rates over this period (table 1 ▶). For age groups less than 65 years there was little change but admission rates increased among older groups. There was a 29% rise among women and a 40% rise among men in those aged more than 74 years. Similarly, admissions for haemorrhage remained stable for younger patients but increased for older age groups. For those aged 75 and over, admission rates rose by 30% among women and by 41% among men.
Table 1.
Average annual age standardised rate for finished consultant episodes for gastric ulcer and peptic ulcer not otherwise specified, in England from 1989/90 to 1998/9. Age standardised within age bands to European standard population. Finished consultant episodes per 100 000
| Women | Men | ||||||||
| Age group (y) | 1989–91 | 1992–5 | 1996–8 | % Change | 1989–91 | 1992–5 | 1996–8 | % Change | |
| Gastric ulcer and peptic ulcer NOS | 25–44 | 8.4 | 8.3 | 8.6 | 2 | 14.6 | 14.5 | 14.4 | −1 |
| 45–64 | 35.4 | 30.9 | 32.1 | −9 | 50.0 | 49.2 | 47.5 | −5 | |
| 65–74 | 95.5 | 95.2 | 106.8 | 12 | 96.2 | 108.5 | 122.7 | 28 | |
| 75+ | 107.2 | 129.7 | 138.1 | 29 | 95.1 | 116.3 | 133.6 | 40 | |
| All ages | 22.8 | 22.6 | 24.2 | 6 | 28.5 | 30.0 | 31.1 | 9 | |
| Gastric ulcer and peptic ulcer NOS: haemorrhage | 25–44 | 2.0 | 1.9 | 2.2 | 9 | 4.7 | 5.2 | 5.1 | 8 |
| 45–64 | 11.7 | 11.6 | 11.0 | −6 | 19.7 | 21.4 | 18.9 | −4 | |
| 65–74 | 36.0 | 39.6 | 41.0 | 14 | 40.4 | 51.1 | 55.2 | 36 | |
| 75+ | 43.1 | 57.0 | 56.1 | 30 | 41.9 | 54.0 | 59.2 | 41 | |
| All ages | 7.9 | 8.7 | 8.7 | 10 | 11.1 | 13.0 | 12.8 | 15 | |
| Gastric ulcer and peptic ulcer NOS: perforation | 25–44 | 0.7 | 0.5 | 0.6 | −8 | 0.8 | 1.0 | 1.0 | 20 |
| 45–64 | 2.9 | 2.7 | 2.5 | −15 | 3.9 | 3.4 | 3.3 | −17 | |
| 65–74 | 9.0 | 8.5 | 8.7 | −3 | 7.7 | 7.7 | 7.0 | −9 | |
| 75+ | 12.2 | 12.1 | 10.7 | −12 | 10.4 | 9.3 | 7.2 | −31 | |
| All ages | 2.1 | 1.9 | 1.9 | −10 | 2.3 | 2.1 | 2.0 | −13 | |
NOS, Not otherwise specified.
% Change, percentage change from 1989–91 to 1996–8.
There was a general decline in admission rates for gastric ulcer perforation. The decline was up to 31% among elderly men (aged 75 and over) over a period when gastric ulcer admissions overall and admissions for gastric ulcer haemorrhage increased.
Finished consultant episodes for duodenal ulceration (England 1989/90–1998/9)
Although there was little overall change in admission rates for duodenal ulcer, there was a decline for younger patients and a substantial rise for older individuals (table 2 ▶). Admission rates increased by 33% among women aged more than 74 years and by 49% among elderly men. Much of this rise related to admissions for haemorrhage. For the 65–74 year age group there was a 48% rise among women and 45% rise among men. In the age group more than 74 years, rates rose by 50% and 65%, respectively. Overall, hospitalisation rates for haemorrhage increased by 25% among women and by 13% among men.
Table 2.
Average annual age standardised rate for finished consultant episodes for duodenal ulceration in England from 1989/90 to 1998/9. Age standardised within age bands to European standard population. Finished consultant episodes per 100 000
| Women | Men | ||||||||
| Age group (y) | 1989–91 | 1992–5 | 1996–8 | % Change | 1989–91 | 1992–5 | 1996–8 | % Change | |
| Duodenal ulcer | 25–44 | 10.7 | 8.6 | 8.3 | −22 | 33.4 | 29.8 | 26.1 | −22 |
| 45–64 | 29.9 | 26.7 | 24.6 | −18 | 71.9 | 65.9 | 61.7 | −14 | |
| 65–74 | 65.2 | 72.2 | 81.7 | 25 | 118.7 | 133.3 | 150.1 | 26 | |
| 75+ | 84.0 | 105.1 | 111.4 | 33 | 112.4 | 149.6 | 167.1 | 49 | |
| All ages | 19.1 | 19.0 | 19.3 | 1 | 44.1 | 43.3 | 42.6 | −3 | |
| Duodenal ulcer: haemorrhage | 25–44 | 1.9 | 2.1 | 2.0 | 7 | 10.3 | 11.3 | 9.6 | −6 |
| 45–64 | 9.2 | 8.9 | 9.3 | 1 | 27.6 | 28.6 | 26.7 | −3 | |
| 65–74 | 22.2 | 27.9 | 33.0 | 48 | 49.4 | 63.4 | 71.8 | 45 | |
| 75+ | 30.8 | 41.4 | 46.3 | 50 | 48.4 | 71.7 | 80.0 | 65 | |
| All ages | 5.7 | 6.5 | 7.2 | 25 | 16.3 | 18.8 | 18.5 | 13 | |
| Duodenal ulcer: perforation | 25–44 | 2.0 | 1.8 | 2.0 | 1 | 5.3 | 5.2 | 5.1 | −4 |
| 45–64 | 6.9 | 6.5 | 5.9 | −14 | 13.9 | 12.3 | 11.4 | −18 | |
| 65–74 | 18.0 | 20.0 | 20.6 | 14 | 25.6 | 26.5 | 24.2 | −6 | |
| 75+ | 25.5 | 28.8 | 26.2 | 3 | 24.3 | 29.0 | 29.5 | 21 | |
| All ages | 4.7 | 4.8 | 4.7 | 0 | 8.4 | 8.2 | 7.8 | −7 | |
% Change, percentage change from 1989–91 to 1996–8.
Overall perforation rates remained stable among women but declined slightly among men. The latter was due to a decline in admissions for perforation among younger men despite a 21% rise in the 74 years and over age group.
Operations
Finished consultant episodes for operations (England 1989/90–1998/9)
The main indication for vagotomy (A27) is duodenal ulcer. Partial gastrectomy (G28) in contrast is performed both for gastric and duodenal ulcer disease as well as for gastric neoplasms. Vagotomy (A27) rates fell by about 83% between 1990/1–1992/3 and 1996/7–1998/9) (table 3 ▶). Over the same period, partial gastrectomy rates declined by about 30%. The frequency of simpler operations, including oversewing of bleeding or perforated gastric or duodenal ulcers (G35 and G52), increased, particularly for duodenal ulcer in younger ages. Overall operation rates changed little when the four categories were taken together.
Table 3.
Average annual age standardised rate for finished consultant episodes for operations in England from 1989/90 to 1998/9. Age standardised within age bands to European standard population. Finished consultant episodes per 100 000
| Women | Men | ||||||||
| Age group (y) | 90/1–92/3 | 93/4–95/6 | 96/7–98/9 | % Change | 90/1–92/3 | 93/4–95/6 | 96/7–98/9 | % Change | |
| A27 Vagotomy | 25–44 | 1.0 | 0.4 | 0.1 | −87 | 3.0 | 1.1 | 0.4 | −88 |
| 45–64 | 2.3 | 0.9 | 0.4 | −83 | 4.8 | 2.2 | 0.8 | −84 | |
| 65–74 | 3.6 | 2.0 | 0.9 | −76 | 5.9 | 3.3 | 1.6 | −73 | |
| 75+ | 2.8 | 2.0 | 0.5 | −82 | 3.5 | 2.7 | 0.9 | −73 | |
| All ages | 1.3 | 0.6 | 0.2 | −83 | 2.8 | 1.3 | 0.5 | −84 | |
| G28 Partial gastrectomy | 25–44 | 1.1 | 0.9 | 0.8 | −30 | 1.6 | 1.3 | 1.0 | −40 |
| 45–64 | 7.0 | 5.3 | 4.5 | −36 | 12.5 | 9.9 | 7.5 | −40 | |
| 65–74 | 16.4 | 14.6 | 13.3 | −19 | 26.9 | 24.0 | 20.9 | −22 | |
| 75+ | 11.9 | 11.1 | 9.1 | −24 | 16.4 | 15.0 | 13.0 | −21 | |
| All ages | 3.7 | 3.1 | 2.6 | −29 | 6.2 | 5.2 | 4.1 | −33 | |
| G35 Gastric ulcer operations | 25–44 | 0.4 | 0.4 | 0.4 | 24 | 0.8 | 0.8 | 0.9 | 12 |
| 45–64 | 1.7 | 1.6 | 1.8 | 2 | 2.6 | 2.4 | 2.6 | 1 | |
| 65–74 | 5.2 | 5.9 | 6.1 | 17 | 5.4 | 5.8 | 5.7 | 5 | |
| 75+ | 6.2 | 6.9 | 6.7 | 8 | 5.0 | 5.8 | 4.4 | −12 | |
| All ages | 1.2 | 1.2 | 1.3 | 11 | 1.5 | 1.6 | 1.6 | 3 | |
| G58 Duodenal ulcer operations | 25–44 | 0.9 | 1.2 | 1.6 | 73 | 2.5 | 3.7 | 4.1 | 61 |
| 45–64 | 3.5 | 4.3 | 4.3 | 22 | 6.4 | 8.6 | 8.8 | 38 | |
| 65–74 | 9.1 | 11.5 | 14.0 | 55 | 11.8 | 18.0 | 18.6 | 58 | |
| 75+ | 11.2 | 16.6 | 15.9 | 42 | 11.7 | 17.1 | 18.4 | 57 | |
| All ages | 2.3 | 3.0 | 3.2 | 43 | 3.9 | 5.6 | 5.9 | 52 | |
% Change, percentage change between 1990/1–1992/3 and 1996/7–1998/9.
Mortality rates
Mortality from gastric ulcer and peptic ulcer site unspecified (England and Wales)
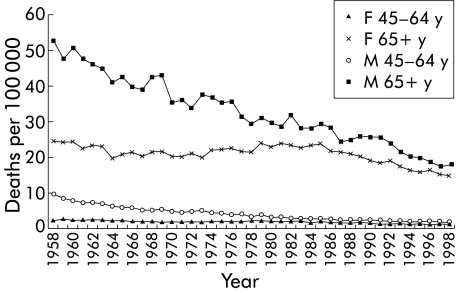
Mortality rates from gastric ulcer were highest in the elderly, being about 20 times greater among patients aged 65 years and over compared with those aged 35–64 years (fig 1 ▶). There was a general decrease in mortality from 1958 among most age groups. A 2:1 male predominance in mortality rates among those aged 65 years and over in 1958 declined to near unity by the mid 1980s.
Figure 1.
Age specific mortality rates for males (M) and females (F) for gastric ulcer and peptic ulcer site unspecified in England and Wales (standardised to European standard population).
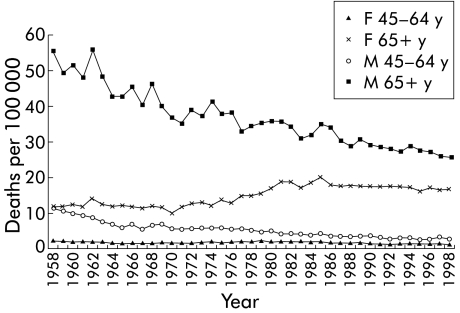
Mortality from duodenal ulcer (England and Wales)
Mortality among women aged 65 years and over doubled between 1970 and 1986 but has since stabilised (fig 2 ▶). For men aged 65 years and over, mortality steadily declined, the decrease slowing after the mid 1980s. Mortality from duodenal ulcer declined by 75% in the younger age groups over this period.
Figure 2.
Age specific mortality rates for males (M) and females (F) for duodenal ulcer in England and Wales (standardised to European standard population).
Prescribing
Number of items prescribed in England from 1990 to 1999
The number of prescriptions for ulcer healing drugs increased two and a half times between 1990 and 1999 (table 4 ▶). Prescriptions for H2 receptor antagonists rose early in the period but subsequently declined to about the same level as in 1990. Proton pump inhibitors started to be prescribed from 1990 and now make up about 60% of drugs prescribed.
Table 4.
Number of items prescribed in England from 1990 to 1999. Prescription Cost Analysis system (Department of Health)
| 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | % Change | |
| Aspirin 75 mg | 1930 | 2851 | 3776 | 4691 | 5896 | 6472 | 7737 | 8638 | 9781 | 10 848 | 462 |
| Aspirin 300 mg | 1219 | 822 | 797 | 764 | 1548 | 1517 | 1501 | 1452 | 1367 | 1203 | −1 |
| Oral anticoagualants | 1153 | 1347 | 1477 | 1665 | 1958 | 2246 | 2589 | 2938 | 3312 | 3698 | 221 |
| Non-steroidal anti-inflammatory drugs | 16 387 | 17 397 | 17 973 | 18 080 | 17 894 | 17 543 | 17 722 | 18 047 | 18 297 | 18 534 | 13 |
| Selective serotonin reuptake inhibitors | — | 510 | 1178 | 1885 | 2681 | 3808 | 5136 | 6556 | 7582 | 8929 | 1651 |
| H2 receptor antagonists | 6201 | 7149 | 7534 | 7765 | 7864 | 7659 | 7547 | 7208 | 6846 | 6455 | 4 |
| Proton pump inhibitors | 182 | 465 | 1163 | 2095 | 3230 | 4484 | 5691 | 6812 | 8143 | 9527 | 5126 |
% Change, percentage change between 1990 and 1999.
Between 1990 and 1999, prescriptions for NSAID increased by about 13%. Prescribing of oral anticoagulants increased by 200% and aspirin 75 mg increased by 460% between 1990 and 1999. In contrast, there has been little change in prescriptions for aspirin 300 mg. SSRI were introduced in 1991 and prescriptions increased 15-fold by 1998.
DISCUSSION
We examined hospital admissions and mortality due to peptic ulcer in England for the period 1989 to 1998 to see if previously described trends had continued. In particular, we were interested to see if there was any change that might be attributable to the introduction of proton pump inhibitors and antibiotic treatment for H pylori. Although there was a continuing general decline in hospital admissions for peptic ulcer among younger individuals, the pattern has changed for the elderly. The rise in perforation in women aged 65 years and over has not continued. Instead there has been a general rise in haemorrhage in both sexes, particularly for duodenal ulcer. In contrast, mortality rates have declined in all groups since 1986 except for women aged 65 years and over with duodenal ulcer, among whom the rates have remained stable. This may reflect improvement in medical treatment.
During this period, there has been a general decline in definitive surgery for peptic ulceration. Partial gastrectomy rates have decreased by 30% and vagotomy rates by 83%. There was a corresponding rise in simpler procedures for haemorrhage and perforation. Presumably, surgeons are now oversewing ulcers but relying on subsequent medical treatment to actually heal the ulcers and cure the ulcer diathesis.
Earlier studies of hospital admissions for peptic ulcer in England and Wales between 1958 and 1982 showed a general decline except among women aged 65 years and over. In this group there was a rise in perforations, especially for duodenal ulcer.3–5 In Scotland between 1975 and 1990, overall admissions for duodenal ulcer declined although again there was an increase in perforated duodenal ulcers among women aged 65 and over.6 There was a general decline across all ages in admissions for duodenal ulcer haemorrhage.
The advent of effective medical treatment for peptic ulcer since the 1970s may have been expected to reduce the frequency of hospital admissions. However, these advances have occurred at a time when drugs which may cause ulcers are increasingly used—for example, NSAID from the 1970s and low dose aspirin in the 1990s. The effect of H2 receptor antagonists, the first effective ulcer healing drugs to be introduced, on hospital admission rates for peptic ulcer is uncertain. In the Trent region in England, there was a reduction in waiting list admissions and operations for uncomplicated duodenal ulcer in the five years following their introduction.7 However, overall emergency admissions for uncomplicated, bleeding, and perforated duodenal ulcer remained unchanged. Indeed, admission rates for bleeding and perforation increased among the elderly.7 In Tayside, Scotland, long term continuous therapy with H2 receptor antagonists for peptic ulcer was used much more widely than in the rest of the country. Hospital admissions for peptic ulcer and for ulcer haemorrhage declined significantly in the 1980s while little change was seen in Scotland as a whole.13 A composite analysis of various indices of peptic ulcer disease in six Western countries in relation to the introduction of histamine H2 antagonists showed an effect on work loss and disability rather than hospitalisation and mortality.15 In Denmark, hospitalisation and mortality rates from peptic ulcer complications increased, especially among the elderly, from 1981 to 1993, even with the introduction of histamine H2 antagonists and proton pump inhibitors.11 We have also demonstrated an increase in hospital admissions for ulcer haemorrhage among older patients in England, despite the introduction of proton pump inhibitors and curative treatment for H pylori, as well as a 2.5-fold increase in prescriptions for ulcer healing drugs between 1990 and 1999. The relationship of acid suppressant drug prescribing to the frequency of peptic ulcer is complex. In addition to healing peptic ulcers, they are also coprescribed with NSAID for ulcer prophylaxis and widely used for functional dyspepsia and for gastro-oesophageal reflux.
This was an ecological study based on aggregate data—that is, using groups rather than individuals as the unit of analysis. Observations of groups may not allow causal inferences to be drawn about the individual, a problem known as the “ecological fallacy”.16 The number of tablets of, for example, an NSAID which are prescribed may not be directly translated into its biological activity because of differences in dosage schedules, patient compliance, patient selection for drug prescription, coprescription of gastroprotective drugs, and so on. On the other hand, a therapeutic modality may have an effect on subjects other than those for whom the drug was prescribed. For example, widespread use of anti-H pylori treatment may reduce the reservoir of disease in the community and secondarily reduce infection rates among those not previously exposed to the pathogen. Although aspirin, anticoagulants, and NSAID drugs are known to promote peptic ulcer disease and its complications, while anti-H pylori treatment is known to have a beneficial effect, our ability to draw inferences regarding cause and effect on temporal trends is necessarily limited in an ecological analysis such as this.
However, our finding of a decrease in hospital admissions for peptic ulcer among younger individuals but an increasing frequency among older individuals would be consistent with the effect of a decline in H pylori infection concurrently with an increase in the use of ulcerogenic drugs. The former may be expected to affect younger subjects while older individuals would be more likely to receive NSAID, aspirin, and antidepressant drugs. The increase in peptic ulcer admissions in the elderly is unlikely to be due to a greater prevalence of H pylori infection in older patients as the birth cohort with the highest prevalence of H pylori infection was those born around 1910.17 H pylori prevalence in cohorts of subjects born after that time would therefore be expected to be progressively lower.
It has been estimated that for every 1000 patients on vascular prophylaxis with aspirin, one or two per year will have a gastrointestinal bleed.18 There were approximately nine million more prescriptions for 75 mg tablets of aspirin in 1999 compared with 1990. If each prescription was for 30 tablets and one 75 mg tablet was taken each day, there would have been 900 000 more person years of exposure in 1999. The 900–1800 more episodes of gastrointestinal bleeding which would be expected approximates the 1000 excess admissions actually observed.
Hospital episode statistics (started in 1987) are based on finished consultant episodes rather than admissions. Rates derived from them cannot therefore be compared directly with earlier studies that were based on the 10% sample of admissions from the hospital inpatient enquiry, the collection of which ended in 1985.3–5 However, these data are robust, including all finished episodes rather than the 10% sample in the hospital inpatient enquiry. Ninety five per cent of admissions generate a single finished consultant episode although a minority generate multiple consultant episodes during an admission. We feel therefore that the trends demonstrated within the period 1989–1999 can be compared with those observed in previous studies based on data from the hospital inpatient enquiry. Furthermore, the diagnoses recorded on hospital episode statistics have been shown to be accurate, thus reducing the risk of misclassification errors.19 Any coding inaccuracies should even out in a study of trends. There has been no major change in diagnostic modalities for peptic ulcer disease over the period under study. According to Rockall and colleagues,20 the incidence of upper gastrointestinal haemorrhage as a reason for admission (not including haemorrhage occurring in hospital) is approximately 103/100 000 adults/year, or 82/100 000 population/year for males. Peptic ulcer accounted for approximately 35% of these, or 29/100 000/year. This is very close to our values of 31.8/100 000/year for 1992–5 (duodenal ulcer 18.8, gastric ulcer 13.0). For women, our values were 15.2/100 000/year compared with 20.0/100 000/year based on Rockall's data. We were unable to assess the impact of changes in lifestyle factors such as alcohol intake and smoking habits, which have been shown to be risk factors for peptic ulcer complications.21 However, these would have changed relatively little during the period of this study.
In conclusion, while peptic ulcer admissions and mortality have declined in frequency among young individuals, admission rates for gastric and duodenal ulcer haemorrhage, and duodenal ulcer perforation, have increased among older patients. Further work is needed to establish the reasons for these different time trends for haemorrhage and perforation, for the young and old, for gastric and duodenal ulcer, and the relative contribution of various drugs, both ulcer causing and ulcer healing, to the pattern of peptic ulcer disease in our population.
Abbreviations
NSAID, non-steroidal anti-inflammatory drugs
SSRI, serotonin reuptake inhibitors
REFERENCES
- 1.Brinton W. On the pathology, symptoms and treatment of ulcer of the stomach. London: John Churchill, 1857.
- 2.Langman MJS. Aetiology of peptic ulcer. In: Murphy M, Rawlins MD, Venebles CW, eds. Diseases of the gut and pancreas. Oxford: Blackwell, 1987:268–81.
- 3.Brown RC, Langman MJ, Lambert PM. Hospital admissions for peptic ulcer during 1958–72. BMJ 1976;1:35–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Coggon D, Lambert P, Langman MJ. 20 years of hospital admissions for peptic ulcer in England and Wales. Lancet 1981;1:1302–4. [DOI] [PubMed] [Google Scholar]
- 5.Walt R, Katschinski B, Logan R, et al. Rising frequency of ulcer perforation in elderly people in the United Kingdom. Lancet 1986;1:489–92. [DOI] [PubMed] [Google Scholar]
- 6.Jibril JA, Redpath A, Macintyre IM. Changing pattern of admission and operation for duodenal ulcer in Scotland. Br J Surg 1994;81:87–9. [DOI] [PubMed] [Google Scholar]
- 7.Bardhan KD, Cust G, Hinchliffe RF, et al. Changing pattern of admissions and operations for duodenal ulcer. Br J Surg 1989;76:230–6. [DOI] [PubMed] [Google Scholar]
- 8.Elashoff JD, Grossman MI. Trends in hospital admissions and death rates for peptic ulcer in the United States from 1970 to 1978. Gastroenterology 1980;78:280–5. [PubMed] [Google Scholar]
- 9.Spiro HM. Peptic ulcer: Moynihan's or Marshall's disease? Lancet 1998;352:645–6. [DOI] [PubMed] [Google Scholar]
- 10.Sonnenberg A, Fritsch A. Changing mortality of peptic ulcer disease in Germany. Gastroenterology 1983;84:1553–7. [PubMed] [Google Scholar]
- 11.Andersen IB, Bonnevie O, Jorgensen T, et al. Time trends for peptic ulcer disease in Denmark, 1981–1993. Analysis of hospitalization register and mortality data. Scand J Gastroenterol 1998;33:260–6. [DOI] [PubMed] [Google Scholar]
- 12.Langman MJ, Weil J, Wainwright P, et al. Risks of bleeding peptic ulcer associated with individual non-steroidal anti-inflammatory drugs. Lancet 1994;343:1075–8. [DOI] [PubMed] [Google Scholar]
- 13.Penston JG, Crombie IK, Waugh NR, et al. Trends in morbidity and mortality from peptic ulcer disease: Tayside versus Scotland. Aliment Pharmacol Ther 1993;7:429–42. [DOI] [PubMed] [Google Scholar]
- 14.de Abajo FJ, Rodriguez LA, Montero D. Association between selective serotonin reuptake inhibitors and upper gastrointestinal bleeding: population based case-control study. BMJ 1999;319:1106–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bloom BS. Cross-national changes in the effects of peptic ulcer disease. Ann Intern Med 1991;114:558–62. [DOI] [PubMed] [Google Scholar]
- 16.Morgenstern H. Ecologic studies in epidemiology: concepts, principles, and methods. Annu Rev Public Health 1995;16:61–81. [DOI] [PubMed] [Google Scholar]
- 17.Banatvala N, Mayo K, Megraud F, et al. The cohort effect and Helicobacter pylori. J Infect Dis 1993;168:219–21. [DOI] [PubMed] [Google Scholar]
- 18.Smith TCG. Lessons from the fifteenth European Aspirin Foundation Scientific Meeting held in the Royal College of Surgeons, Edinburgh, on 26 October 1999. Proc R Coll Physicians Edinb 2000;30:140–4. [Google Scholar]
- 19.Majeed A. Hospital admissions data: why are they collected? Clinician Manage 1998;7:160–6. [Google Scholar]
- 20.Rockall TA, Logan RF, Devlin HB, et al. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom. Steering Committee and members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ 1995;311:222–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Andersen IB, Jorgensen T, Bonnevie O, et al. Smoking and alcohol intake as risk factors for bleeding and perforated peptic ulcers: a population-based cohort study. Epidemiology 2000;11:434–9. [DOI] [PubMed] [Google Scholar]