We read with interest the Gut File report by Dr Ross and colleagues of hypomagnesaemia due to malabsorption, eventually responding to oral magnesium oxide supplementation (Gut 2001;48:857–8). Our experience however has been different. For the past seven years we have managed a 65 year old woman with short bowel syndrome (right hemicolectomy for Duke's C colorectal carcinoma and thereafter a terminal ileal resection for abscess formation).
High ileostomy output was initially difficult to manage (after excluding infection, secreting gut hormone tumours by normal hormone levels, and despite dietary and pharmacological modifications). Clinical signs of hypomagnesaemia and hypocalcaemia ensued. An initial trial with magnesium glycerophosphate (September 1992 to December 1993) was insufficient to sustain her serum magnesium levels requiring frequent “top ups” of intravenous magnesium.1 In December 1993, she was switched to magnesium oxide supplementation but despite this the frequency of intravenous magnesium “top ups” were not reduced. Compliance was not deemed to be an issue with our patient.
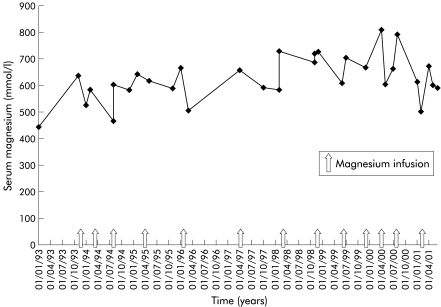
Since then we have managed this woman while still taking magnesium oxide supplements with almost 3–6 monthly (fig 1 ▶) intravenous magnesium replacement through a peripheral line and have avoided insertion of a Hickman line and all its associated complications.2 While we agree that a trial of magnesium oxide is prudent and until the pharmacokinetics are better understood, this preparation may not be sufficient, especially in patients with extensive resection of the small bowel, as demonstrated in our patient.
Figure 1.
Serum magnesium levels in our patient over the course of treatment with magnesium oxide supplements and intravenous magnesium replacement.
References
- 1.British National Formulary, 41st edn. London: BMA and Royal Pharmacological Society of Great Britain, 2001.
- 2.Graham DR, Keldermans MM, Klemm LW, et al. Infectious complications among patients receiving home intravenous therapy with peripheral, central or peripherally placed central venous catheters. Am J Med 1991;91:95–100S. [DOI] [PubMed] [Google Scholar]