BACKGROUND
Although choledochoduodenostomy was widely performed for choledocholithiasis in the 1960s and 1970s, Roux-en-Y hepaticojejunostomy is currently the preferred biliary-enteric anastomosis for benign and malignant disease and is generally considered a low risk procedure, aside from the potential for cholangitis.
AIMS
We report three cases referred over a 12 month period in which cholangiocarcinoma developed after previous biliary-enteric anastomosis, and review the literature to determine the likelihood of an association.
PATIENTS
Case No 1
A 51 year old female developed obstructive jaundice 26 years after choledochoduodenostomy for a biliary stricture after iatrogenic bile duct injury. Endoscopic retrograde cholangiopancreatography (ERCP) showed neoplastic infiltration at the level of the anastomosis, biopsy of which revealed cholangiocarcinoma (fig 1 ▶). Percutaneous transhepatic cholangiography (PTC) demonstrated diffuse biliary strictures and biliary endoprostheses were inserted. Death occurred two months later.
Figure 1.
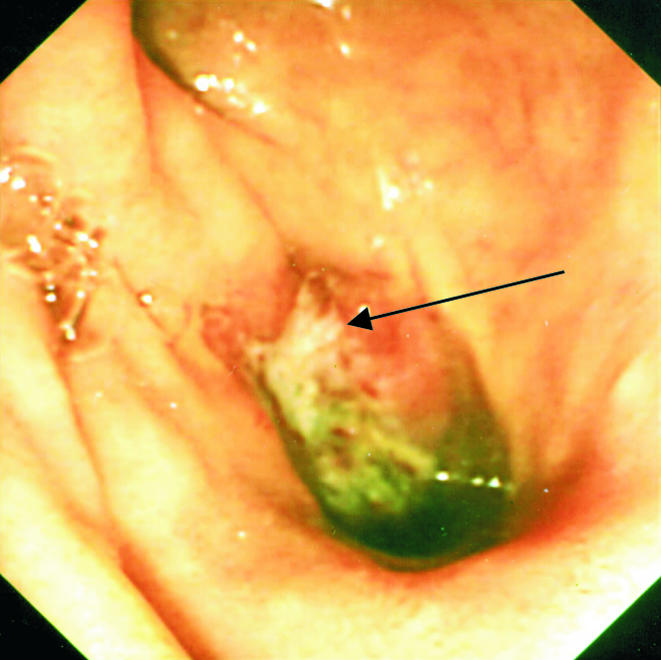
Adenocarcinoma (arrow) on the biliary side of a choledochoduodenal anastomosis, as seen at endoscopic retrograde cholangiopancreatography.
Case No 2
A 73 year old female presented with obstructive jaundice 39 years after biliary-enteric anastomosis for iatrogenic bile duct injury. Computed tomography scanning and PTC revealed cirrhosis and focal strictures of the biliary confluence and common bile duct, which were stented. The patient died two weeks later. Autopsy confirmed cirrhosis and multifocal cholangiocarcinoma.
Case No 3
A 72 year old male renal allograft recipient developed obstructive jaundice 15 years after choledochoduodenostomy for choledocholithiasis. ERCP and PTC demonstrated hilar stenosis and biopsy confirmed cholangiocarcinoma. A palliative surgical bypass was undertaken. The patient died four months after diagnosis.
DISCUSSION
The occurrence of cholangiocarcinoma many years following surgical biliary-enteric bypass may be coincidental but it raises the possibility of an aetiological link. An alarming incidence of cholangiocarcinoma among a cohort 1003 patients has recently been reported,1 while another study reported a 7.4% incidence of cholangiocarcinoma after sphinctero -plasty.2 Twelve other cases of cholangiocarcinoma occurring late (average 20 years) after biliary-enteric drainage have also been reported.3–9 Mean survival was 3.3 months. This dismal outcome may be due to the multifocal nature of the tumours, supporting the hypothesis of toxic carcinogenesis affecting the biliary epithelium, causing a field change.
As for choledochal cysts where there is an abnormal pancreaticocholedochal junction, an activated mixture of pancreatic secretions and bile may contain cytotoxic components, and may result in chronic inflammation.10, 11 Bacterial infection is a further factor contributing to the chronic irritation of the mucosa. All three patients in this report demonstrated the known association between choledochoduodenostomy and cholan -gitis.12 This strong relationship is supported in two previous reports.1, 2 Mucosal changes have been documented in humans late after choledochoduo -denostomy,13 and in two animal models biliary drainage procedures have induced premalignant or malignant changes to the biliary epithelium.14, 15
It remains to be verified whether the recent epidemiological data which have shown a steady increase in the incidence of cholangiocarcinoma in England and Wales since the early 1980s16 corresponds to the popularity of choledochoduodenostomy two decades previously.
CONCLUSION
Experimental, clinical, and epidemiological data are available to support the hypothesis of a link between cholangiocarcinoma and biliary drainage procedures. We believe that the evidence is strong enough to prompt a reappraisal of policies regarding these procedures.
Acknowledgments
V Bettschart was supported by the “Sicpa Foundation” and the “Fondation du 450ème Anniversaire de l'Université de Lausanne”.
REFERENCES
- 1.Tocchi A, Mazzoni G, Liotta G, et al. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients. Ann Surg 2001;234:210–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hakamada K, Sasaki M, Endoh M, et al. Late development of bile duct cancer after sphincteroplasty: a ten- to twenty-two-year follow-up study. Surgery 1997;121:488–92. [DOI] [PubMed] [Google Scholar]
- 3.Shields HM. Occurrence of an adenocarcinoma at the choledochoenteric anastomosis 14 years after pancreatoduodenectomy for benign disease. Gastroenterology 1977;72:322–4. [PubMed] [Google Scholar]
- 4.Haratake J, Horie A, Takeda N. (Cancer of the intra-pancreatic common bile duct observed 9 years after choledochojejunostomy). Gan No Rinsho 1983;29:1367–70. [PubMed] [Google Scholar]
- 5.Leborgne J, Heloury Y, Lavignolle A, et al. (Cancer of the bile ducts above the anastomosis following choledocoduodenal anastomosis for common bile duct lithiasis. 2 cases). Ann Chir 1984;38:369–73. [PubMed] [Google Scholar]
- 6.Herba MJ, Casola G, Bret PM, et al. Cholangiocarcinoma as a late complication of choledochoenteric anastomoses. AJR Am J Roentgenol 1986;147:513–15. [DOI] [PubMed] [Google Scholar]
- 7.Perez RL, Gabarrell OA, Vinas SJ, et al. (Biliary tract cancer following bilioenteric anastomosis). Rev Esp Enferm Dig 1994;86:853–5. [PubMed] [Google Scholar]
- 8.Schumacher G, Bechstein WO, Kling N, et al. (Bile duct carcinoma in an adenoma in the anastomotic area after hepaticojejunostomy—a case report). Z Gastroenterol 1997;35:1081–6. [PubMed] [Google Scholar]
- 9.Strong RW. Late bile duct cancer complicating biliary-enteric anastomosis for benign disease. Am J Surg 1999;177:472–4. [DOI] [PubMed] [Google Scholar]
- 10.Kobayashi S, Asano T, Yamasaki M, et al. Risk of bile duct carcinogenesis after excision of extrahepatic bile ducts in pancreaticobiliary maljunction. Surgery 1999;126:939–44. [DOI] [PubMed] [Google Scholar]
- 11.Shimada K, Yanagisawa J, Nakayama F. Increased lysophosphatidylcholine and pancreatic enzyme content in bile of patients with anomalous pancreaticobiliary ductal junction. Hepatology 1991;13:438–44. [PubMed] [Google Scholar]
- 12.Madden JL, Chun JY, Kandalaft S, et al. Choledochoduodenostomy: an unjustly maligned surgical procedure? Am J Surg 1970;119:45–54. [DOI] [PubMed] [Google Scholar]
- 13.Eleftheriadis E, Tzioufa V, Kotzampassi K, et al. Common bile-duct mucosa in choledochoduodenostomy patients—histological and histochemical study. HPB Surg 1988;1:15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurumado K, Nagai T, Kondo Y, et al . Long-term observations on morphological changes of choledochal epithelium after choledochoenterostomy in rats. Dig Dis Sci 1994;39:809–20. [DOI] [PubMed] [Google Scholar]
- 15.Tajima Y, Eto T, Tsunoda T, et al. Induction of extrahepatic biliary carcinoma by N-nitrosobis(2-oxopropyl)amine in hamsters given cholecystoduodenostomy with dissection of the common duct. Jpn J Cancer Res 1994;85:780–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor-Robinson SD, Toledano MB, Arora S, et al. Increase in mortality rates from intrahepatic cholangiocarcinoma in England and Wales 1968–1998. Gut 2001;48:816–20. [DOI] [PMC free article] [PubMed] [Google Scholar]


