Abstract
Background: Biliary decompression with endoscopic sphincterotomy (EPT) is beneficial in patients with biliary obstruction due to common bile duct (CBD) stones. However, it is not known whether EPT with decompression of the bile duct is beneficial in patients with acute cholangitis and gall bladder stones but without evidence of CBD stones.
Aim: A randomised controlled study to assess the effect of EPT on the outcome of patients suffering from acute cholangitis with gall bladder stones but with no CBD stones on initial endoscopic retrograde cholangiopancreatography.
Patients: A total of 111 patients were recruited into the study.
Methods and results: Fifty patients were randomised to receive EPT while 61 patients received no endoscopic intervention. There was a significant difference in the duration of fever in the EPT and non-EPT groups (mean (SD): 3.2 (2.2) days v 4.3 (2.1) days; p<0.001). Duration of hospital stay was also shorter in the EPT group than in the non-EPT group (mean (SD): 8.1 (3.0) v 9.1 (3.2) days; p=0.04). Patients were followed up for a mean (SD) of 42.4 (11.1) months. Twenty three patients (20.3%) developed recurrent acute cholangitis (RAC): 14 patients (12.6%) in the EPT group and nine patients (8.1%) in the non-EPT group (p=0.09).
Conclusion: EPT in patients with acute cholangitis without CBD stones decreased the duration of acute cholangitis and reduced hospital stay but it did not decrease the incidence of RAC.
Keywords: acute cholangitis, recurrent acute cholangitis, endoscopic sphinterotomy
Bacterial cholangitis resulting from benign or malignant obstruction is a life threatening disease, especially in the elderly. Approximately 15–30% of patients with acute cholangitis fail to respond to antibiotic therapy and require urgent biliary drainage.1
Endoscopic sphincterotomy (EPT) was first used for the treatment of choledocholithiasis and cholangitis in 1974.2,3 Early results showed that EPT with or without stone extraction can be an effective treatment for acute cholangitis but is best avoided in critically ill patients with acute suppurative cholangitis as repeated biliary manipulation and/or injection of contrast can increase the chance of cholangiovenous reflux and worsen the ongoing septicaemia in this group of patients.
The current recommendation is that the initial treatment of acute cholangitis should consist of intravenous antibiotic therapy directed against enteric gram negative pathogens followed by elective endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and treatment of biliary obstruction. Patients who do not respond to appropriate antimicrobial therapy within 24–48 hours should undergo emergency ERCP for biliary drainage. If possible, the bile duct should be deeply cannulated and purulent bile aspirated to decompress the biliary system.4
Biliary decompression with or without EPT is beneficial in patients with biliary obstruction due to either common bile duct (CBD) stones or malignant obstruction. However, it is not known if EPT with decompression of the bile duct is beneficial in patients with acute cholangitis and gall stones (GB stones) but without evidence of CBD or intrahepatic stones. Vaira and colleagues5 suggested that EPT was not necessary in younger patients because it is possible to provide close surveillance for such patients. However, for elderly patients follow up is difficult and missed bile duct stones are associated with increased morbidity and mortality and so it is their policy to perform an EPT and trawl the bile duct with a balloon or a basket. To date there has been no controlled study in this particular group of patients with acute cholangitis without CBD stones on ERCP.
Therefore, we conducted a randomised controlled study to assess the effect of EPT on the outcome of patients suffering from acute cholangitis, with GB stones but no CBD stones on initial ERCP. The primary aim of the study was to compare the outcome of patients who received EPT with those who did not. The secondary aim of this study was to determine if EPT can prevent the development of recurrent acute cholangitis (RAC) on long term follow up.
METHODS
Patients admitted to the Department of Medicine, Queen Mary Hospital for acute cholangitis with GB stones between 1 January 1996 and 31 December 1998 were recruited into the study. Those with malignant obstruction, intrahepatic cholelithiasis, and choledocholithiasis on ERCP were excluded. Acute cholangitis was defined as the presence of abdominal pain, fever, jaundice, and dilated CBD on ultrasound (USG).
All patients were commenced on intravenous cefoperazone after blood cultures were taken. Complete blood counts, electrolytes, clotting profile, and liver function tests were monitored daily until discharge. Blood pressure and pulse rate were monitored every hour and temperature was checked every four hours. ERCP with a side viewing duodenoscope (Olympus, Tokyo) was performed within 24–48 hours of admission for all patients. Cefoperazone was switched to another antibiotic if blood culture showed an organism resistant to cefoperazone.
ERCP was carried out in the endoscopy room under fluoroscopic screening (Philips Diagnost 65). For ERCP, patients were given a topical pharyngeal spray with 10% lignocaine, and sedated with intravenous midazolam and pethidine hydrochloride. Duodenal relaxation was induced with intravenous hyoscine butylbromide. Patients were randomised to receive either EPT or no intervention. The CBD was trawled with a Dormia-type basket and balloon catheter after EPT to remove mud and debris in the CBD. Two groups of endoscopists were responsible for performing all ERCPs. Both groups had more than five years of experience in performing ERCP. Patients were randomised to either group according to a list of random numbers generated by a computer booking system. After ERCP, patients were managed by a team of physician who were blinded to the treatment assignment.
Patients were followed up once every three months in the first year and then once every six months in the second year. Thereafter, patients were followed up yearly until the end of the study, in this case the 30 June 2001. A physical examination of the abdomen, cardiovascular and respiratory system, and liver biochemistry were performed for each patient during every follow up.
The primary outcome of this study was RAC. RAC is defined as another episode of abdominal pain, fever, and jaundice with raised alkaline phosphatase and bilirubin levels. The secondary outcomes of this study were hospital stay, duration of fever, and need for inotropic support.
Patients recruited into this study was not referred for a cholecystectomy as some studies have doubted the role of cholecystectomy in the prevention of RAC.6–8 This study was approved by the ethics committee of the Faculty of Medicine of the University of Hong Kong, and informed consent was obtained from each patient.
Statistical analysis
All statistical analyses were performed using the Statistical Program for Social Sciences (SPSS 10.0 for windows, SPSS Inc., Chicago, Illinois, USA). The Student's t test (unpaired, two tailed) was used for single comparison of continuous data, and the χ2 with Yates' correction for continuity or Fisher's exact test for categorical variables. Differences in outcome, fever, hospital stay, subsequent need for inotropic support, and RAC in patients with and without EPT were analysed. An actuarial analysis of risk factors for RAC during follow up was performed with Kaplan-Meier curves, and differences analysed using the log rank test. All statistics were performed on the intention to treat population which included all patients recruited into the study initially. Statistical significance was defined as p<0.05 (two tailed).
RESULTS
During this period, there were 655 patients admitted for acute cholangitis. Of these, 422 patients (64.4%) had CBD stones, 65 (9.9%) had malignant biliary obstruction, 47 (7.7%) had unsuccessful cannulation of the CBD, and 10 patients (1.5%) refused to participate in the study. Therefore, only 111 patients (16.9%) were included in the study.
Fifty patients (45%) were randomised to receive EPT while 61 patients (55%) received no intervention. Mean ages (SD) of the EPT and non-EPT groups were 68.9 (14.8) years and 72.3 (12.2) years, respectively. The male to female ratio in the EPT and non-EPT groups were 27:23 and 32:29, respectively. Demographic data of the two groups are shown in table 1 ▶ and were comparable. None of the patients had internal stenting or nasobiliary drain insertion.
Table 1.
Demographic data for the endoscopic sphincterotomy (EPT) and non-EPT groups
| Variable (normal range) | EPT group (n=50) | Non-EPT group (n=61) | p Value |
| Age (y) | 68.9 (14.8) | 72.3 (12.2) | 0.19 |
| Sex (M:F) | 27:23 | 32:29 | 0.51 |
| Albumin (42–54 g/l) | 38.8 (7.2) | 36.1 (5.5) | 0.07 |
| Bilirubin (7–19 μmol/l) | 41.8 (32.9) | 32.9 (41.1) | 0.07 |
| ALP (51–141 U/l) | 210.3 (111.2) | 198.1 (103.5) | 0.56 |
| ALT (6–53 U/l) | 190.5 (208.8) | 118.1 (164.2) | 0.13 |
| AST (15–40 U/l) | 138.5 (116.1) | 151.4 (266.4) | 0.41 |
| GGT (9–62 U/l) | 309.9 (385.0) | 258.1 (205.1) | 0.86 |
| PT (11.3–13.2 s) | 12.2 (2.4) | 13.2 (16.0) | 0.20 |
| APTT (27.6–37.6 s) | 30.2 (5.1) | 31.7 (10.2) | 0.97 |
| Size of CBD (mm) | 8.9 (2.6) | 9.3 (2.8) | 0.58 |
ALP, alkaline phosphatase; ALT, alanine transaminase; AST, aspartate transaminase; GGT, gamma glutamyl transpeptidase; PT, prothrombin time; APTT, activated partial thromboplastin time; CBD, common bile duct.
There was a significant difference in duration of fever in the EPT and non-EPT groups (mean (SD): 3.2 (2.2) v 4.3 (2.1) days; p<0.001). Duration of hospital stay in the EPT group was also significantly shorter than in the non-EPT group (mean (SD): 8.1 (3.0) v 9.1 (3.2) days; p=0.04). A higher number of patients in the EPT group developed a peak in fever within 24 hours post-ERCP compared with the non-EPT group (17 (34%) v 9 (14.8%) (p=0.02); odds ratio (OR) 2.98, 95% confidence interval (CI) 1.19–7.46).
Two patients (4%) in the EPT group developed post-ERCP complications compared with none in the non-EPT group (p=0.70). The two complications that developed were post-ERCP acute pancreatitis and post-EPT bleeding. Both complications were mild, according to the classification of Cotton and colleagues.9 There was no difference in the subsequent requirement for inotropic support between the EPT and non-EPT groups (0/50 v 1/61; p=0.55). Mortality rate in the EPT group was 2% (1/50) while in the non-EPT group it was 1.6% (1/61) (p=0.25).
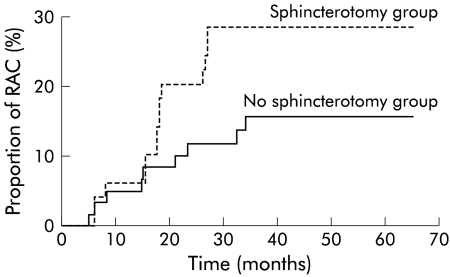
Patients were followed up in our outpatient clinic for a mean (SD) of 42.3 (11.1) months. Eleven patients (9.9%) were lost to follow up. RAC developed in 23 patients (20.7%) with 14 patients (12.6%) in the EPT group and nine (8.1%) in the non-EPT group (p=0.09, OR 2.25, 95% CI 0.88, 5.75). There was no difference in the time to development of RAC between the two groups (p=0.10 by log rank test) (fig 1 ▶). Three patients (6%) in the EPT group developed two episodes of RAC while in the non-EPT group two patients (3.3%) developed two episodes of RAC (p=0.66, OR 1.83, 95% CI 0.29, 11.38). No patient developed more than two episodes of RAC in the follow up period.
Figure 1.
Kaplan-Meier curve showing recurrent acute cholangitis (RAC) in the sphincterotomy and non-sphincterotomy groups.
Liver biochemistry, size of CBD, age, and sex were not found to be associated with the development of RAC (all NS). No patient in either group developed acute cholecystitis or carcinoma of the gall bladder.
DISCUSSION
Endoscopic decompression of the biliary system with either stents or EPT has revolutionised the management of acute cholangitis.10–12 Endoscopic drainage and decompression have been shown to be successful in treating 97% of patients with calculous cholangitis who do not respond to conservative treatment, with a mortality rate of only 4.7%.13 But in these studies 80% of their patients had CBD stones and approximately 20–30%5,11–13 of patients with acute cholangitis did not have CBD stones, probably due to spontaneous passage of CBD stones. The issue of whether or not endoscopic decompression with EPT is beneficial in patients with acute cholangitis who do not have CBD stones has not been addressed.
Our study showed that urgent EPT in this group of patient can shorten the duration of fever and also the duration of hospitalisation. Shortening of hospital stay can be explained by the shorter duration of fever in the EPT group allowing patients in this group to be discharged earlier.
A significant number of patients in the EPT group developed a peak in fever within 24 hours post-EPT compared with the control group. However, this was not shown to affect the outcome nor did it lead to a greater need for inotropic support. The peak in fever and shortened duration of fever in the EPT group was probably related to a rapid decrease in biliary endotoxaemia within 24 hours after biliary decompression, as shown by Lau and colleagues.14 This release in endotoxins by biliary decompression probably resulted in a systemic inflammatory response with a peak in fever within this period. Also, it is this rapid decrease in both biliary and serum endotoxins that led to a shortened duration of fever in this group.
EPT did not improve the primary outcome or mortality rate in this group of patients with acute cholangitis. The mortality rate in this series was low (approximately 2%). This low mortality rate is in contrast with the reported mortality rate of 4–10% for acute cholangitis.13,15 We believe the difference is due to the high percentage of patients with CBD stones in these two previous studies. Whereas in this study all patients recruited had a dilated CBD, none had a CBD stone on cholangiography. Perhaps the prognosis of acute cholangitis in those without a CBD stone is better than in those with a CBD stone in situ. Further studies are needed to confirm this observation.
Even though there was no significant difference in post-ERCP complications between the two groups of patients (p=0.70), the post-ERCP complication rate in the EPT group was higher than that in the non-EPT group (4% v 0%). It may not be advisable to perform an EPT in this specific group of patients as it does not alter mortality rate or outcome. Even though EPT can shorten the duration of acute cholangitis and duration of hospital stay, this has to be balanced by the risk of post-EPT complications.
EPT did not decrease the incidence of RAC on follow up for a mean period of 42 months. The development of RAC was not altered by EPT (p=0.10). The role of EPT in young adults remains controversial because of concerns of the long term consequences of EPT, with issues raised about the effect of chronic bacterial contamination, recurrent stones, and risk of cancer. Some have argued that by damaging the sphincteric mechanism, the CBD is more easily contaminated by duodenal juice. If the duodenum is not sterile, as in most elderly patients, bacteria can pass from the intestine into the bile leading to repeated episodes of acute cholangitis.16–18
Our study had several limitations. Firstly, endoscopic USG was not performed in any patient and we also did not look for crystals or small stones. Hence small stones may have been missed. However, we believe it is unlikely that a significant amount of small stones were missed because the prognosis of acute cholangitis in patients with small CBD stones is thought to be much poorer than those without small CBD stones if a sphincterotomy and clearance of small stones is not performed. Our results showed that the mortality rate and subsequent requirement for inotropic support in both the EPT and non-EPT groups were comparable (1/50 v 1/61 (p=0.25) and 0/50 v 1/61 (p=0.55), respectively).
Secondly, cholecystectomy was not performed in this study which may affect the long term outcome of these patients. When this study was designed initially, our only aim was to define the role of sphincterotomy in this group of patient and as some studies have also questioned the role of cholecystectomy in the prevention of RAC,6–8 we decided not to perform cholecystectomy. Whether cholecystectomy can help to decrease the incidence of RAC in this group of patients is not known and further randomised trials may be needed to clarify the role of cholecystectomy in this group of patient.
In conclusion, EPT in patients with acute cholangitis without CBD stones can help to decrease the duration of acute cholangitis and reduce hospital stay but it does not affect the outcome of acute cholangitis. As EPT does not decrease the development RAC it is therefore not routinely recommended because the short term gains do not justify the increased complications and perhaps death that may result from unnecessary sphincterotomy in the absence of ductal stones.
Abbreviations
RAC, recurrent acute cholangitis
CBD, common bile duct
EPT, endoscopic sphincterotomy
ERCP, endoscopic retrograde cholangiopancreatography
GB stone, gall bladder stone
USG, ultrasound
REFERENCES
- 1.Andrew DJ, Johnson SE. Acute suppurative cholangitis, a medical and surgical emergency. Am J Gastroenterol 1970;54:141–54. [PubMed] [Google Scholar]
- 2.Kawai K, Akasaka Y, Murakami K, et al. Endoscopic sphincterotomy of the ampulla of vater. Gastrointest Endosc 1974;20:148–51. [DOI] [PubMed] [Google Scholar]
- 3.Sohma S, Tatekawa I, Okamoto Y, et al. Endoscopic papillotomy: a new approach for extraction of residual stones. Gastrointest Endosc 1974;164:446–52. [Google Scholar]
- 4.Lee JG. Role of endoscopic therapy in cholangitis. Am J Gastroenterol 1998;93:2016–18. [DOI] [PubMed] [Google Scholar]
- 5.Vaira D, D'Anna L, Ainley C, et al. Endoscopic sphincterotomy in 1000 consecutive patients. Lancet 1989;2:431–4. [DOI] [PubMed] [Google Scholar]
- 6.Martin DF, Tweedle DEF. Endoscopic management of common duct stones without cholecystectomy. Br J Surg 1987;74:209–11. [DOI] [PubMed] [Google Scholar]
- 7.Saito M, Tsuyuguchi T, Yamaguchi T, et al. Long term outcome of endoscopic papillotomy for choledocholithiasis with cholecystolithiasis. Gastrointest Endosc 2000;51:540–5. [DOI] [PubMed] [Google Scholar]
- 8.Tanaka M, Ikeda S, Yoshimoto H, et al. Long term fate of the gallbladder after endoscopic sphincterotomy:complete follow up study of 122 patients. Am J Surg 1987;154:505–9. [DOI] [PubMed] [Google Scholar]
- 9.Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991;37:383–93. [DOI] [PubMed] [Google Scholar]
- 10.Leese T, Neoptolemos JP, Baker AR, et al. Management of acute cholangitis and the impact of endoscopic sphincterotomy. Br J Surg 1986;73:988–92. [DOI] [PubMed] [Google Scholar]
- 11.Popiela T, Karcz D, Marecik J. Endoscopic sphincterotomy as a therapeutic measure in cholangitis and as prophylaxis against recurrent biliary tract stones. Endoscopy 1987;19:14–16. [DOI] [PubMed] [Google Scholar]
- 12.Siegel JH, Rodriquez R, Cohen SA, et al. Endoscopic management of cholangitis: critical review of an alternative technique and report of a large series. Am J Gastroenterology 1994;89:1142–6. [PubMed] [Google Scholar]
- 13.Leung JWC, Chung SCS, Sung JJY, et al. Urgent endoscopic drainage for acute suppurative cholangitis. Lancet 1989;I:1307–9. [DOI] [PubMed] [Google Scholar]
- 14.Lau JYW, Ip SM, Chung SCS, et al. Endoscopic drainage aborts endotoxemia in acute cholangitis. Br J Surg 1996;83:181–4. [PubMed] [Google Scholar]
- 15.Lai ECS, Mok FPT, Tan ESY, et al. Endoscopic biliary drainage for severe acute cholangitis. N Eng J Med 1992;326:1582–6. [DOI] [PubMed] [Google Scholar]
- 16.Cetta F. Bile infection documented as initial event in the pathogenesis of brown pigment biliary stones. Hepatology 1986;6:482–9. [DOI] [PubMed] [Google Scholar]
- 17.Gregg JA, De Girolami P, Carr-Locke DL. Effect of sphincterotomy on the bacteriologic characteristics of common bile duct. Am J Surg 1985;149:666–71. [DOI] [PubMed] [Google Scholar]
- 18.Skar V, Skar AG, Midtvedt T, et al. Bacterial growth in the duodenum and in the bile of patients with gallstone disease treated with endoscopic papillotomy (EPT). Endoscopy 1986;18:10–13. [DOI] [PubMed] [Google Scholar]