Wallace et al (Gut 2001;49:29–34) clearly describe the difficulties with AGA guidelines for endoscopy in the light of their study in identifying young oesophagogastric pathology. They concluded that better clinical prediction strategies are needed. In the UK we have found similar failings in our own guidelines for endoscopy1 for identification of young patients with oesophagogastric carcinoma. The national data suggesting oesophagogastric carcinoma is rare in patients under 55 years seemed at odds with the large number of patients we had seen in this age group in recent years.
We reviewed our oesophagogastric cancers over three years and found 76 patients under the age of 55 years between January 1997 and December 1999. The hospital records of these patients were examined with the general practice records where possible. A detailed review was undertaken in patients under 50 years old, looking at their presenting symptoms, stage, location, nature, and size of tumour. Timings were noted from the date symptoms first developed, referral date, date of diagnosis, and date of death. Kaplan-Meier methods were used to estimate survival.
Of the 460 patients with oesophagogastric carcinoma, 74 (16%) were found to be less than 55 years of age at diagnosis. Thirty eight patients (8.3%) were less than 50 years of age, and 19 (4.1%) were less than 45 years. Detailed analysis of patients under 50 years revealed that 29 (76%) of 38 patients had dysphagia at the time of presentation (mean duration four months (range 1–9)). Three patients recalled food occasionally sticking after swallowing for 2, 14, and 20 years, respectively. Reflux or heartburn was recalled prior to presentation by 57%, with a mean duration of 6.8 years (3 weeks to 20 years). Seventeen patients (45%) had been prescribed acid suppression or antacid therapy prior to referral. Seventy one per cent were adenocarcinomas, 16% squamous, and 13% others, and average length was 6.8 cm (range 1–16). Fourteen involved the oesophagogastric junction, 15 the oesophagus, and nine the stomach alone. Staging of 37 patients revealed: one T1 tumour, nine T2, 12 T3, and 15 T4 tumours. Forty per cent had metastasis at presentation and 34% were tertiary referrals.
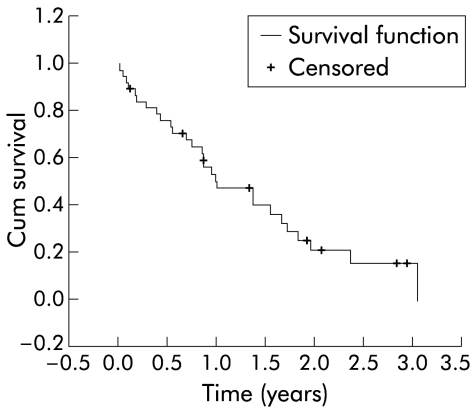
Twenty three patients had a resection, nine of whom had adjuvant chemotherapy and two had radiotherapy. There were 11 palliative, nine chemotherapy, and two radiotherapy treatments. Nine patients were stented. Only four of 23 resections had no lymph node spread. There was no perioperative mortality but median survival was only one year (fig 1 ▶). Currently, only eight patients are alive.
Figure 1.
Kaplan-Meier curve of survival of oesophagogastric cancer patients in those less than 50 years of age.
The current UK government guidelines specifically state that “The chance of a dyspeptic patient under the age of 55 having gastric cancer is one in a million”. This cannot be true given that one unit saw 38 cases of carcinoma in the oesophagus and stomach under the age of 50 years over a three year period. Twenty three had disease involving the stomach; almost all had some prodromal dyspepsia and a high proportion had reflux disease.
Gastro-oesophageal cancer presents late; reliable indicators for the presence of disease are still to be found, although the association with reflux disease has been confirmed recently.2 The young present with advanced disease and, as reported by Bowry and colleagues,3 quickly progress to end stage disease. Our referral bias does not explain this effect. We chose to look at patients under 50 years in detail, particularly as this is the proposed increase to the BSG guidelines. The BSG guidelines use 45 years to restrict access, suggesting endoscopy in those patients older than 45 years with new onset dyspepsia and only in younger patients with alarm symptoms. Guidelines issued by the UK Department of Health4 state that 55 years of age is the cut off for referral, with at least one high risk factor or new onset dyspepsia. Local Cancer Networks can allow 50 or 45 years as a cut off. In our unit, increasing the age to 50 years for patients with new dyspepsia will clearly disadvantage patients when the potential life saving window is made even smaller.
Reflux often precedes the development of oesophageal carcinoma. Is relief of symptoms using medical treatment enough to prevent malignant change or may it even mask a developing tumour? Access to endoscopy needs to be improved in young patients who present with intermittent dyspepsia if early diagnosis is to be made. The development of more sophisticated endoscopic modalities will also make inroads into achieving earlier diagnosis. Without prevention or early diagnosis in this group there is unlikely to be any progress made to extending the lives of these patients.
Our data do not prove that early endoscopy would actually save these patients from a certain death. What it clearly demonstrates is that using the current guidelines, our small region allows 30 of 38 patients under 50 years in a three year period to die of oesophageal or gastric carcinoma. Nationally, this translates into a major failure to adequately diagnose and treat oesophagogastric cancer in young people. The guidelines of diagnosis fail. A screening method is urgently needed for this rapidly increasing cancer problem. Standard endoscopy is too cumbersome and expensive; new technologies may change our whole approach.
Acknowledgments
We would like to thank our colleagues, Mr John Bancewicz and Ms Laura Formela, Consultant Upper GI Surgeons, for allowing us to include their patients in this report.
References
- 1.British Society of Gastroenterology. Dyspepsia Management Guidelines. London: BSG, 1996.
- 2.Lagergren, J, Bergstrom R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med 1999;340:825–31. [DOI] [PubMed] [Google Scholar]
- 3.Bowry DJ, Clark GWB, Rees BI, et al. Outcome of oesophagogastric carcinoma in young patients. Postgrad Med J 1999;75:22–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Health. Referral Guidelines for Suspected Cancer. London: Department of Health, April 2000 (http://www.doh.gov.uk/pub/docs/doh/guidelines.pdf-taken Nov 2000).