Abstract
Background: Irritable bowel syndrome developing following infective gastroenteritis accounts for approximately 1 in 10 of unselected IBS patients.
Aims: To define the long term natural history of post-infective IBS (PI-IBS).
Methods: A total of 436 individuals, who had previously responded to a questionnaire on their bowel habits following an acute episode of gastroenteritis, were sent a questionnaire about their current bowel habits and physical and mental health six years after their initial illness.
Results: Complete data on original bowel habit, episodes of gastroenteritis, mental health history, and subsequent bowel habit at six years were obtained in 192 individuals. Of these, there were 14 cases of “post-infective IBS” (PI-IBS) and 13 who had IBS prior to infection (previous IBS). Over the six year follow up period there were 20 “new non-infective IBS cases” (new IBS). The strongest risk factor for developing any type of IBS was female sex (relative risk 2.2, p<0.05). Compared with new IBS, those with PI-IBS had significantly more days with loose stools (p<0.05) but a similar number of days with pain, urgency, and bloating. Six of 14 (43%) PI-IBS and four of 13 (31%) previous IBS patients recovered by six years (NS). Of 27 IBS patients followed for six years, only 1/8 with a history of anxiety or depression recovered compared with 9/19 without such a history (p=0.19).
Conclusion: PI-IBS differs from non-infective IBS by having more diarrhoeal features. Less than half of both PI-IBS and non-infective IBS cases recover over six years. A history of anxiety and depression severe enough to warrant treatment may impair recovery but larger numbers are needed to prove this.
Keywords: irritable bowel syndrome, infection, mental health, prognosis
Irritable bowel syndrome (IBS) accounts for 2% of general practice consultations1 and perhaps 30–40% of gastroenterological outpatient visits2 but our understanding of its pathophysiology is poor. Although those seeing doctors appear over anxious, the apparent relationship between anxiety and symptoms may be an artefact of selective self referral as non-anxious individuals with similar symptoms may never consult a doctor.3 The precise role of anxiety is thus uncertain and as only half of IBS patients are overtly anxious, it is clear that there must be other causes. Recent surveys have indicated that, depending on the country and whether they are in primary or secondary care, 6–17% of unselected IBS patients report that their IBS began with a bout of gastroenteritis.4 Several prospective studies reported in the last few years have indicated that a substantial proportion of patients (7–33%)5,6 with acute bacterial gastroenteritis develop IBS symptoms that persist for many months. Although there are obviously many possible causes of IBS, two prospective studies using non-infected controls indicate that bacterial gastroenteritis is one of the strongest risk factors for developing IBS.7,8 Risk factors for developing such “post-infective IBS” (PI-IBS) include: (1) duration of initial illness,6 (2) female sex, (3) hypochondriasis,5 and (4) adverse life events in the previous one year.
One of the difficulties in studying the pathogenesis of IBS is its heterogeneous nature and therefore PI-IBS is attractive because patients appear to have a uniform initial insult and a more homogeneous clinical pattern. Furthermore, as infection is a near random process, the initial infected group should be representative of the general population. Studying the outcome should therefore allow demonstration of a causal role of factors such as mental health, which might otherwise be regarded as confounders. We present here the results of a further survey of patients originally studied in 1994–19956 and examine factors which predicted their prognosis. We have compared these “post-infective IBS” patients with new cases of “non-infective IBS” which developed in the cohort over the six year study period, and with patients with “pre-existing IBS” who had IBS before their bout of gastroenteritis.
PARTICIPANTS AND METHODS
Participants
The statutory notifications of infectious diseases record system was used to identify a cohort of 544 residents of Nottingham with a food poisoning illness in 1994–1995. This cohort was investigated by questionnaire in a previous study of the effects of food poisoning at six months.6 The 436 people who returned the original questionnaire and who were known to have had a positive stool culture were contacted at six years to determine the long term consequences of their initial infection.
Methods
Ethics approval was obtained from the University of Nottingham Medical School Ethics Committee. A self completion questionnaire was designed and piloted. This included questions covering socioeconomic circumstances, current bowel symptoms, current and past treatment for general and mental health, visits to doctors and other alternative health practitioners, and any investigations as a consequence of bowel problems. The questionnaire was mailed to the old address used in the 1995 study enclosing a prepaid reply envelope. Owing to data protection problems we were unable to check for changes of address. A reminder was sent at one month.
The presence of IBS was determined at three time points—namely, prior to infection, six months, and six years after infection using the Rome I criteria.9 These require the presence of abdominal pain or discomfort relieved by defecation or associated with change in stool form or frequency together with at least two of the following symptoms: (1) altered stool frequency (>3×/day or <3×per week), (2) altered stool form (hard/loose), (3) altered stool passage (straining/urgency), (4) passage of mucus per rectum, or (5) bloating or abdominal distension. These symptoms had to be present >25% of the time (in practice two or more days per week). Classification was based on a consensus of two experienced physicians (KRN, RCS). IBS patients were divided according to their bowel symptoms into diarrhoea predominant (D-IBS), alternating (Alt-IBS), and constipation predominant (C-IBS) IBS using recently published criteria.10 These data were linked to the previous questionnaire on bowel habit before and after the index episode of food poisoning. All patients were asked about past or current treatment for anxiety or depression, which was used as a surrogate measure of previous mental health. There were no reports of psychotic mental illness.
Statistics
Data were entered into Access 97 and analysed using SPS for Windows V10. Data are presented for the most part as median and ranges and differences between groups assessed using the non-parametric Mann-Whitney U test. Associations between categorical data were assessed using the χ2 statistic.
RESULTS
Response rate
Twenty four of the original 436 had died during the six year follow up, leaving 412, of whom 206 replied (response rate 50%). This low response rate is in part accounted for by the poor response rate in the younger age groups, especially 17–29 year olds. Many of these were university students in 1994–1995 who almost certainly had moved over the six years of follow up. We examined non-responders to look for bias in replies using the known risk factors for developing IBS—namely, sex, duration of original illness, and per cent in whom bowels had returned to normal by six months (table 1 ▶). There was no bias in the main prognostic factors except for age, which was slightly lower in non-responders.
Table 1.
Comparison of responders and non-responders
| Responders (n=206) | Non-responders (n=194) | |
| Sex (M/F) | 84/122 | 94/100 |
| Age (y) (median (range)) | 52 (82–19) | 38 (41–45)*** |
| Duration of original illness (days) | 8 (1–75) | 8 (1–90) |
| % reporting changed bowel habit | 25 | 24 |
| No with PI-IBS | 14 | 11 |
PI-IBS, post-infective irritable bowel syndrome.
***p<0.001.
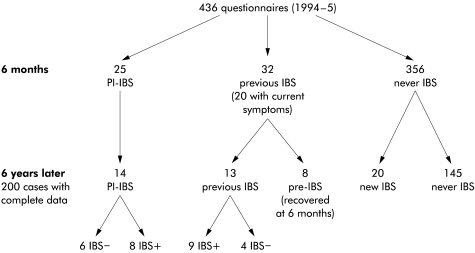
Defining the subgroups (fig 1 ▶)
Figure 1.
Patients were subdivided according to the type of irritable bowel syndrome (IBS) at six months after the original infection and at six years of follow up. Twelve cases of pre-existing IBS who lost their IBS symptoms at six months (eight of whom returned the second questionnaire) are omitted from the analysis.
When the questionnaires were scored, complete data were available for 192 subjects. Four distinct groups were defined. Fourteen individuals had IBS at six months after infection having not had it before (group 1, PI-IBS); 13 had IBS at six months but also had it before their infection (group 2, previous IBS); 20 developed IBS during the six year follow up having never had it before (group 3, new IBS); while 145 never had IBS at any time (group 4, never IBS). There were also five replies from individuals who had lost their IBS symptoms permanently at six months and three who got better transiently but were again symptomatic at six years. These small subgroups are not considered further.
Post-infectious IBS (group 1)
At six months the majority had either D-IBS (five) or Alt-IBS (eight) with only one case of C-IBS. After six years eight had persistent IBS, largely with the same symptoms as before, only two individuals changing their categorisation, shifting from Alt-IBS to C-IBS.
Prognostic factors
Examining possible risk factors for persistent IBS in group 1 (table 2 ▶) showed that both female sex and a past history of treatment for anxiety or depression tended to be associated with worse outcome, although owing to the small numbers these findings did not reach statistical significance. Comparing outcome after six years, six of 14 (43%) subjects in group 1 recovered, a proportion which did not differ significantly from those in group 2, of whom four of 13 (33%) recovered (table 3 ▶).
Table 2.
Prognostic factors for post-infective irritable bowel syndrome (PI-IBS) after six years of follow up
| Recovered | Persistent IBS | p Value* | |
| History of anxiety/depression | |||
| Yes | 0 | 3 | |
| No | 6 | 5 | 0.20 |
| Sex | |||
| Female | 4 | 8 | |
| Male | 2 | 0 | 0.16 |
*Fisher's exact test.
Table 3.
Features of the various irritable bowel syndrome (IBS) groups
| Group 1 PI-IBS | Group 2 previous IBS | Group 3 new IBS | Group 4 never IBS | χ2 test | p Value | |
| n | 14 | 13 | 20 | 145 | ||
| History of anxiety/depression | ||||||
| Yes | 3 | 5 | 5 | 31 | 2.0 | 0.6 |
| No | 11 | 8 | 15 | 113 | ||
| Sex | ||||||
| Female | 12 | 10 | 14 | 76 | 9.4 | 0.02 |
| Male | 2 | 3 | 6 | 69 | ||
| Current HRT females only | ||||||
| Yes | 3 | 2 | 1 | 11 | 1.8 | 0.6 |
| No | 9 | 8 | 13 | 63 | ||
| Recovery at 6 years | ||||||
| Yes | 6 | 4 | F test* | 0.7 | ||
| No | 8 | 9 | ||||
PI-IBS, post-infective irritable bowel syndrome.
*Fisher's exact test.
Given the similarity of groups 1 and 2, we can combine them to consider the prognosis in 27 IBS patients who were followed for six years. Only one of eight with a past history of anxiety and depression recovered compared with nine of 19 without such a history (Fisher's exact test, p=0.19).
Investigations and health care resource utilisation in PI-IBS
Further bowel investigations in the six years after the initial illness were reported by 11 of 14 patients in group 1 (outpatient referral two, barium enema two, flexible sigmoidoscopy two, and colonoscopy two). This was broadly similar to group 4 (n=145) (outpatient referral 13, barium enema six, flexible sigmoidoscopy three, colonoscopy two) with only flexible sigmoidoscopy and colonoscopy being used significantly more often in the PI-IBS group (p<0.05 and p<0.01, respectively).
Comparison of PI-IBS with new cases of IBS developing over six years of follow up: group 1 versus group 3
Table 4 ▶ compares the features in these two groups. PI-IBS patients had a significantly greater number of days per week with loose stools. Consequently, there were proportionately more patients categorised as D-IBS and also a tendency for PI-IBS patients to have more days of pain, although both of these differences failed to reach statistical significance. Other parameters such as days with urgency, mucus, and bloating were almost identical. There were 15 new cases of apparently infective diarrhoea of whom one appeared to develop new IBS. However, as there were no stool cultures we have not analysed this further.
Table 4.
Comparison of features of groups 1 and 3 during five years of follow up
| Group 1 PI-IBS | Group 3 new IBS | |
| n | 14 | 20 |
| IBS subtype | ||
| Diarrhoea predominant IBS | 5 | 3 |
| Alternating IBS | 8 | 12 |
| Constipation predominant IBS | 1 | 5 |
| Days with abdominal pain (mean (SEM)) | 3.2 (0.4) | 2.8 (0.3) |
| Loose stool (days/week) | 3.4 (0.7)* | 2.0 (0.2) |
| Urgency (days/week) | 2.6 (0.6) | 2.6 (0.3) |
PI-IBS, post infective irritable bowel syndrome.
*p<0.05, PI-IBS versus new IBS.
Risk factors for IBS in all subtypes
Considering all IBS patients, female sex was associated with IBS (p<0.05) while a history of treatment for anxiety and depression was not (table 3 ▶). Being on hormone replacement therapy (HRT) did not alter the risk of IBS.
DISCUSSION
Although experienced clinicians have seen many patients who claim that their bowel habit was perfectly normal until a bout of gastroenteritis, it is only recently that prospective studies using modern criteria for IBS have definitively established this as a real clinical syndrome rather than an artefact of selective recall.5,6,11 Earlier studies using less precise criteria have studied prognosis in PI-IBS,12 but the present study is the largest and longest prospective study of PI-IBS to be reported using modern diagnostic criteria. The length of follow up (six years) is a strength but also a weakness as inevitably individuals move away and become untraceable. However, we detected no difference between responders and non-responders with regard to other known risk factors for IBS, apart from age, which has minimal effect.
We believe therefore that our results are applicable to most PI-IBS cases. Our main finding was that about half of patients with PI-IBS recover over a six year period, a prognosis which was similar to those who had IBS before they experienced their infection.
In spite of a similar prognosis, PI-IBS appears to be a distinct subgroup of IBS which may have a different pathogenesis. As we have previously reported, patients who developed PI-IBS after Campylobacter enteritis have increased enteroendocrine and chronic inflammatory cells in the rectal mucosa.13 Furthermore, PI-IBS patients attending outpatient clinics have significantly elevated enteroendocrine cells compared with IBS patients without a history of infection at onset.14 As our study shows, PI-IBS should not be confused with painless functional diarrhoea since when compared with our non-infective IBS group, those with PI-IBS had slightly more days of pain. We found PI-IBS to have more diarrhoeal features than other subtypes of IBS with significantly more days per week with loose stools. There was also a tendency for PI-IBS to be more likely to be classified as D-IBS than other non-infective IBS types, although owing to small numbers this difference was not significant.
We did not find anxiety to be a risk factor for developing PI-IBS although with such small numbers one should be cautious about dismissing any role as others have found that neuroticism predisposes to PI-IBS.5 However, we did find that it tended to impair recovery as none of the three PI-IBS cases with a history of treatment for anxiety or depression recovered. Considering both groups 1 and 2 together, only one of eight patients with a past history of anxiety and depression recovered compared with nine of 19 without such a history, but owing to the small numbers this association did not reach statistical significance. This concept is however supported by other recent data showing that chronic stress impairs recovery from a range of functional gastrointestinal disorders.15
The increased risk of females in developing all types of IBS is confirmed in our study. In attempting to dissect this further, we also examined the use of HRT as a surrogate measure of hormonal deficiency but found that this was unrelated to outcome.
General practitioners do not appear to overreact to PI-IBS and only a small number of tests were ordered, the only difference compared with the non-IBS population being a small increase in the rate of flexible sigmoidoscopy and colonoscopy.
We conclude that physicians looking after patients who develop IBS following bacterial gastroenteritis can reassure their patients that this is a well recognised problem. The illness may be prolonged but approximately half will recover within six years. Practitioners should however be alert to the coexistence of anxiety or depression as this may impair recovery.
Abbreviations
IBS, irritable bowel syndrome
PI-IBS, post infective IBS
D-IBS, diarrhoea predominant IBS
Alt-IBS, alternating IBS
C-IBS, constipation predominant IBS
HRT, hormone replacement therapy
Footnotes
Presented in abstract form at the United European Digestive Diseases Week, Amsterdam, October 2001–12–06
REFERENCES
- 1.Thompson WG, Heaton KW, Smyth GT, et al. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut 2000;46:78–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wells NE, Hahn BA, Whorwell PJ. Clinical economics review: irritable bowel syndrome. Aliment Pharmacol Ther 1997;11:1019–30. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Sandler RS, Broom CM, et al. Urgency and fecal soiling in people with bowel dysfunction. Dig Dis Sci 1986;31:1221–5. [DOI] [PubMed] [Google Scholar]
- 4.Longstreth GF, Hawkey CJ, Ham J, et al. Demographic and clinical characteristics of patients with irritable bowel syndrome (IBS) from three practice settings. Gastroenterology 2000;118:A146. [Google Scholar]
- 5.Gwee KA, Leong YL, Graham C, et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut 1999;44:400–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neal KR, Hebden J, Spiller R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ 1997;314:779–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez LA, Ruigomez A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. BMJ 1999;318:565–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ilnyckyj A, Choudri SH, Duerksen D. Association of travel related diarrhoea (TD) with irritable bowel syndrome (IBS): Is post-infectious IBS a true entity? Gastroenterology 1999;116:A1011. [Google Scholar]
- 9.Drossman DA, Thompson WG, Talley NJ, et al. Identification of sub-groups of functional gastrointestinal disorders. Gastroent Int 1990;3:159–72. [Google Scholar]
- 10.Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. Gut 1999;45(suppl 2):II43–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKendrick MW, Read NW. Irritable bowel syndrome—Post salmonella infection. J Infect 1994;29:1–3. [DOI] [PubMed] [Google Scholar]
- 12.Chaudary NA, Truelove SC. The irritable colon syndrome. Q J Med 1962;123:307–22. [PubMed] [Google Scholar]
- 13.Spiller RC, Jenkins D, Thornley JP, et al. Increased rectal mucosal enteroendocrine cells, T lymphocytes and increased gut permeability following acute Campylobacter enteritis and in post-dysenteric irritable bowel syndrome. Gut 2000;47:804–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dunlop SP, Wyke H, Jenkins D, et al. Entero-endocrine cells are elevated in diarrhoea predominant IBS. Gut 2001;48 (Suppl I):A44. [Google Scholar]
- 15.Bennett EJ, Tennant CC, Piesse C, et al. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut 1998;43:256–61. [DOI] [PMC free article] [PubMed] [Google Scholar]