Systematic reports of antidepressant use in irritable bowel syndrome (IBS) first appeared in the medical literature three decades ago. Recent meta-analyses of the cumulative controlled experience confirm the efficacy of antidepressants in IBS and other functional gastrointestinal disorders: only 3–4 patients require treatment to demonstrate a benefit over placebo—numbers indicating a solid treatment effect.1–3 Although many of the earlier reports would be considered scientifically flawed by today’s standards, the effects are consistent across studies. Odds ratios of treatment over placebo for primary study outcome, global (or syndromic) response, and pain exceeded 4.0 for each determination in one analysis, and the effect sizes of antidepressant treatment on continuous outcome measures were large.3 These observations in conjunction with reported open label experience and general clinical success have given antidepressants an important position in the therapeutic armamentarium for IBS.4
Most studies have employed tricyclic antidepressants (TCAs), medications that appear to have benefits not necessarily shared across the antidepressant class. Daily dosages of TCAs (25–125 mg/day) that are below the psychiatric range for antidepressant effect typically are effective in IBS, producing at least a moderate response in more than 85% of patients in open label use.5 With the TCAs, onset of action is rapid, effects appear sustained without tachyphylaxis, and the benefits are unrelated to change in measures of anxiety or depression—findings supporting a mechanism of action that is distinct from recognised psychiatric effects of the medications.4,5 Reported experience with contemporary antidepressants, including the selective serotonin reuptake inhibitors, is much less robust.1,6,7 These medications typically are used in full psychiatric dosages, onset of effect on IBS symptoms is not rapid, and the benefits may be related more to a reduction in associated anxiety or depressive symptoms and an indirect effect on IBS symptom reporting.4 The mechanistic difference between TCAs and contemporary antidepressants in IBS symptom management has not been completely determined, but clinical experience (including the benefits of combined treatment in some patients) favours important distinctions between antidepressant types.8
Treatment choices for IBS, in general, depend on symptom pattern (for example, constipation versus diarrhoea predominance) and severity (for example, mild to severe, as characterised by symptom intensity and functional impairment). As severity worsens, pain, other gastrointestinal discomforts (for example, bloating), and perceptions of bowel dysfunction often become dominant; the disorder is accompanied by more psychological distress, higher rates of comorbid psychiatric illness, and less responsiveness to usual treatment.9 Central regulatory control compared with gut factors may be more important in symptom production and perpetuation, and the pattern of bowel dysfunction becomes more important from the standpoint of side effects of therapy than in directing the intervention.4 These patients may be good candidates for antidepressant trials and have symptom severity that justifies the potential adverse effects seen with these agents. TCAs in particular produce unsatisfactory adverse effects in up to 40% of patients receiving open label treatment, such as sedation, other central nervous system complaints, and anticholinergic symptoms.4, 5 When TCAs are used for neuropathic pain management, significant adverse effects compared with placebo are encountered with treatment of as few as 3–4 patients, and a major adverse effect attributable to treatment occurs in slightly fewer than 1 in 20 patients.10 Consequently, antidepressants appear well selected for patients with this off label indication who have at least moderately severe symptoms and in whom these adverse effect profiles are acceptable. Adjunctive treatment with transit altering medications (antidiarrhoeals, laxatives, bulking agents) is required for bowel habit abnormalities that persist or are exacerbated by the antidepressant.
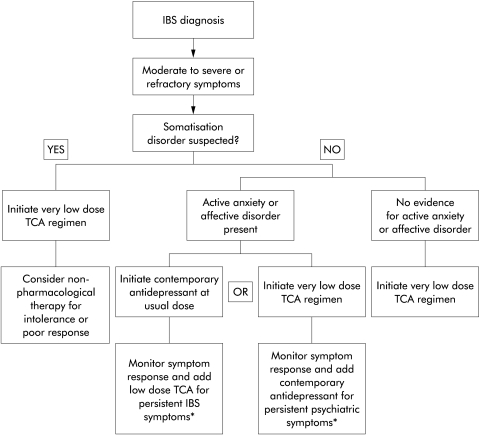
Active anxiety or depression symptoms interfere with treatment, particularly with low dose TCA regimens.5, 11 Some psychological symptoms regress with successful IBS management; those that persist may require direct intervention for global improvement. Patients with many unexplained pain symptoms or syndromes, complicated medical histories beginning at an early age, and other features of somatisation disorder respond less well to antidepressants and often report adverse effects that overshadow drug benefits. These patients should be started at very low daily TCA dosages (for example,10 mg/day) that are increased in similarly small increments. Thus the combination of symptom severity (or at least refractoriness to other interventions), presence of an active anxiety or affective disorder, and features of somatisation disorder weigh into the initial treatment decisions with antidepressants (fig 1).4 Although there is no uniformly accepted approach directing the use of antidepressants for IBS management, the algorithm outlined in fig 1 is successful for many patients.
In the absence of an overt anxiety or affective disorder, TCAs may be preferred over contemporary antidepressants for suitable candidates. Secondary amine TCAs (nortriptyline, desipramine) are better tolerated by many patients than parent tertiary amines (amitriptyline, imipramine, doxepin) because of fewer anticholinergic, sedating antihistaminic, and α- adrenergic adverse effects.4, 5 Starting dosages of 10–25 mg at bedtime are recommended but daily dosages exceeding 30 mg/day are required for sustained benefit in most patients.4, 5 The dosage can be escalated until sustained improvement is observed, adverse effects impair further increment, or the upper limit of conventional psychiatric dosing is reached. Not all patients achieve optimal response in the low dose range. Once a benefit is achieved, months of maintenance treatment may be required before the medication can be withdrawn without recurrence.4, 5 Common long term adverse effects of TCAs that must be considered in the treatment approach include, among others, weight gain, hypertension, and sexual dysfunction. Clinicians using antidepressants in IBS management should be familiar with the adverse effects of these medications during short and long term use.
Summary
Antidepressants are effective in managing IBS symptoms.
TCAs and contemporary antidepressants may reduce IBS symptoms through different mechanisms.
Gradual TCA dosage escalation from a low starting point is appropriate as the initial antidepressant trial for IBS patients in whom the adverse effect profile is considered acceptable for symptom severity.
Presence of an active anxiety or affective disorder or features of somatisation disorder influences the treatment algorithm.
Long term antidepressant treatment may be required to suppress IBS symptoms; vigilance for adverse effects and ongoing weighing of treatment benefits against adverse effects is necessary to optimise chronic management.
Figure 1.
An algorithm for the initiation of antidepressants in irritable bowel syndrome (IBS). *Combined treatment with a tricyclic antidepressant (TCA) and some contemporary antidepressants will reduce hepatic metabolism of the TCA wherein TCA levels must be monitored to avoid toxicity. From Clouse and Lustman.4
REFERENCES
- 1.Jackson JL, O'Malley PG, Tomkins G, et al. Treatment of functional gastrointestinal disorders with antidepressant medications: a meta-analysis. Am J Med 2000;108:65–72. [DOI] [PubMed] [Google Scholar]
- 2.Jailwala J, Imperiale TF, Kroenke K. Pharmacologic treatment of the irritable bowel syndrome: a systematic review of randomized, controlled trials. Ann Intern Med 2000;133:136–47. [DOI] [PubMed] [Google Scholar]
- 3.Clouse RE, Prakash C, Anderson RJ, et al. Antidepressants for functional gastrointestinal symptoms and syndromes: a meta-analysis. Gastroenterology 2001;120(suppl 1):A642. [Google Scholar]
- 4.Clouse RE, Lustman PJ. Antidepressants for irritable bowel syndrome. In: Camilleri M, Spiller RC, eds. Irritable Bowel Syndrome: Diagnosis and Treatment. London: WB Saunders, 2002:161–71.
- 5.Clouse RE, Lustman, PJ, Geisman RA, et al. Antidepressant therapy in 138 patients with irritable bowel syndrome: A five-year clinical experience. Aliment Pharmacol Ther 1994;8:409–16. [DOI] [PubMed] [Google Scholar]
- 6.Creed FH, Fernandes L, Guthrie E, et al. The cost-effectiveness of psychotherapy and SSRI antidepressants for severe irritable bowel syndrome. Gastroenterology 2001;120:A115. [DOI] [PubMed] [Google Scholar]
- 7.Tanum L, Malt UF. A new pharmacologic treatment of functional gastrointestinal disorder. A double-blind placebo-controlled study with mianserin. Scand J Gastroenterol 1996;31:318–25. [DOI] [PubMed] [Google Scholar]
- 8.Nair D, Prakash C, Lustman PJ, et al. Added value of tricyclic antidepressants for functional gastrointestinal symptoms in patients on selective serotonin re-uptake inhibitors (SSRIs). Am J Gastroenterol 2001;96(suppl):S316. [Google Scholar]
- 9.Drossman DA, Whitehead WE, Toner BB, et al. What determines severity among patients with painful functional bowel disorders? Am J Gastroenterol 2000;95:974–80. [DOI] [PubMed] [Google Scholar]
- 10.McQuay HJ, Moore RA. Antidepressants and chronic pain: effective analgesia in neuropathic pain and other syndromes. BMJ 1997;314:763–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lancaster-Smith MJ, Prout BJ, Pinto T, et al. Influence of drug treatment on the irritable bowel syndrome and its interaction with psychoneurotic morbidity. Acta Psychiatr Scand 1982;66:33–41. [DOI] [PubMed] [Google Scholar]