Abstract
Background and aims: A subset of patients with gastro-oesophageal reflux disease (GORD) with refractory symptoms during therapy with proton pump inhibitors (PPIs), have persistent non-acid duodeno-gastro-oesophageal reflux (duodenal reflux). The aim of the present study was to investigate the effect of the GABAB receptor agonist baclofen, which was shown to inhibit the occurrence of transient lower oesophageal sphincter relaxations (TLOSRs) in patients with persistent non-acid duodenal reflux during PPI therapy.
Methods: Patients were eligible for the study if they had persistent reflux symptoms, normal pH monitoring, and pathological Bilitec monitoring during PPI treatment. Upper gastrointestinal endoscopy and reflux symptom score were performed at the beginning of the study. Baclofen 5 mg three times daily was associated with treatment, and was increased by 5 mg every fourth day until a maintenance dose of 20 mg three times daily was reached. A reflux symptom questionnaire, ambulatory pH monitoring, and Bilitec monitoring were repeated four days later while PPI and baclofen were continued. All data are given as mean (SEM) or median (interquartile range) and were compared using the Student’s t test or the Mann-Whitney U test.
Results: Sixteen patients (11 women, mean age 46 (3) years) with persistent heartburn or regurgitation for at least three months, in spite of PPI therapy, were included in the study. Erosive oesophagitis was present in seven patients (five with grade 1, two with grade 2). Under PPI therapy alone, all patients had normal acid exposure (0.3 (0.05; 2.2)% of the time) but pathological duodenal reflux exposure (13.8 (11.8; 15.5)% of the time). After addition of baclofen 20 mg three times daily, acid exposure was similar (0.4 (0.15; 2.3)% of the time; NS) but duodenal reflux had significantly decreased (6.1 (0.8; 10.3)% of the time; p<0.05). The number of duodenal reflux episodes and the number of longlasting duodenal reflux episodes (>5 minutes) was decreased, respectively, from 23 (14.5; 34) to 12 (5; 21) (p = 0.06) and from 5 (3; 8) to 2 (0.5;4.5) (p<0.05). The cumulative severity score for 14 reflux symptoms decreased from 10.3 (1.7) to 5.8 (1.3) (p<0.01). Four patients reported mild side effects of nausea or drowsiness.
Conclusions: The GABAB receptor agonist baclofen improves duodenal reflux and associated reflux symptoms that persist during PPI therapy.
Keywords: gastro-oesophageal reflux disease, transient lower oesophageal sphincter relaxation, gamma-aminobutyric acid, proton pump inhibitors
Gastro-oesophageal reflux disease (GORD), defined as the presence of symptoms or lesions that can be attributed to the reflux of gastric contents into the oesophagus, is one of the most common disorders affecting the gastrointestinal tract.1,2 The advent of proton pump inhibitors (PPIs), which strongly inhibit acid gastro-oesophageal reflux3–6 and which reduce duodeno-gastro-oesophageal reflux (duodenal reflux),7–10 has brought relief to many GORD patients. A subset of patients however have persistent reflux symptoms in spite of therapy with high doses of PPIs.11,12 In up to half of patients with persistent oesophagitis or reflux symptoms in spite of PPI therapy, persisting acid reflux can be demonstrated.11–13 These patients generally respond favourably to a further increase in the dose of PPI.5,6,11,12 In the remaining patients, intraluminal impedance monitoring or fibreoptic bilirubin monitoring (Bilitec) has been used to demonstrate ongoing non-acid reflux or duodenal reflux.13–15 These studies have shown that persisting lesions13,14 and symptoms15 can be related to non-acidic gastro-oesophageal reflux, of gastric and/or duodenal origin, that cannot be abolished by acid suppression. At present, the therapeutic options in these patients are limited. The value of prokinetic therapy in treating duodenal reflux was demonstrated only in patients who underwent partial gastrectomy and very high doses of cisapride were required.16 Antireflux surgery was shown to adequately reverse duodenal reflux9 but not all patients are suitable candidates for surgical therapy.
In both stationary and ambulatory studies, it was established that transient lower oesophageal sphincter relaxations (TLOSRs) are the main pathophysiological mechanism underlying acid reflux events.17–20 Studies combining intraluminal impedance monitoring with manometry also suggest that TLOSRs are the principal mechanism underlying non-acidic reflux episodes.20 Recently, it was shown that acute administration of the gamma-aminobutyric acidB (GABAB) receptor agonist baclofen can inhibit the occurrence of TLOSRs, thereby significantly decreasing acid reflux after a meal.21,22 It seems conceivable therefore that treatment with baclofen might also reduce exposure of the distal oesophagus to duodenal reflux.
The aim of the present study was to investigate the effect of baclofen on symptoms and duodenal reflux, persisting in spite of high dose PPI therapy.
MATERIALS AND METHODS
General study design
Consecutive patients with persistent heartburn or regurgitation while treated for at least three months with omeprazole 20 mg twice daily underwent ambulatory oesophageal pH and Bilitec monitoring at our institution while PPI therapy was continued. Prior to pH and Bilitec monitoring, patients were asked to complete a detailed questionnaire on symptoms and frequency, smoking and drinking habits, weight, and height, and all underwent upper gastrointestinal endoscopy followed by simultaneous ambulatory 24 hour oesophageal pH and Bilitec monitoring on one of the next four days. Treatment with omeprazole 20 mg twice daily was continued; all other drugs potentially affecting gastrointestinal motility and gastrointestinal secretion were discontinued at least one week prior to the study.
Patients were eligible for the study if they had a normal serum bilirubin level and if, under omeprazole 20 mg twice daily, they had normal acid exposure pH monitoring (less than 4% of the time with pH <4) and pathological duodenal reflux monitoring (Bilitec greater than 4.6% of the time with absorbance >0.14).22 These tests served both as pre-entry discrimination and as baseline measurements for the participating patients. Exclusion criteria were: peptic ulcer disease; previous oesophageal, gastric, or biliary surgery; previous abdominal or thoracic radiotherapy; active gastrointestinal bleeding; presence of oesophageal or fundic varices; diabetes mellitus; Zollinger-Ellison syndrome; progressive systemic sclerosis; Raynaud’s syndrome and other vascular diseases; neurological disorders; oesophageal or upper small intestinal Crohn’s disease; herpetic or Candida oesophagitis; or active solid tumour neoplastic disease. In addition, all patients with Barrett’s oesophagus were excluded from the study as the presence of metaplasia in the distal oesophagus is irreversible under medical treatment and may interfere with the assessment of persisting oesophagitis lesions.
In patients who agreed to participate in the study, treatment with omeprazole 40 mg daily was continued and baclofen (Lioresal; Novartis, Brussels, Belgium) 5 mg three times daily with meals was added. Every fourth day, the dose of baclofen was increased by 5 mg three times daily until a dose of 20 mg three times daily was reached after 10 days. On day 14, ambulatory pH and Bilitec monitoring was repeated while treatment with omeprazole 20 mg twice daily and baclofen 20 mg three times daily was continued. The ethics committee of the hospital accepted the study protocol.
Patient selection
Over 20 consecutive months, 78 patients with persistent heartburn or regurgitation while treated for at least three months with omeprazole 20 mg twice daily underwent ambulatory oesophageal pH and Bilitec monitoring at our institution while PPI therapy was continued.
Of 20 eligible patients, 16 (five men and 11 women) gave written informed consent for the study.
Reflux symptoms
Before and at the end of the study, all patients were given a 14 symptom questionnaire (heartburn, acid regurgitation, food regurgitation, chest pain, dysphagia, odynophagia, nausea, vomiting, choking, throat ache, hoarseness, nocturnal cough, nocturnal dyspnoea, wheezing) which they scored for severity using a numerical score (0 = absent, 1 = mild, 2 = moderate, 3 = severe).
Upper gastrointestinal endoscopy
All subjects underwent classical upper gastrointestinal endoscopy. If necessary, they were sedated with intravenous administration of diazepam (up to 10 mg) or midazolam (up to 5 mg). During endoscopy, the presence of oesophagitis was noted and graded according to the modified classification system of Savary and Miller.24 In addition, the presence and extent of Barrett’s oesophagus was noted.
Ambulatory pH monitoring
Ambulatory oesophageal pH monitoring was performed using an antimony pH electrode with a separate skin reference electrode (Synectics Medical, Stockholm, Sweden). Data were stored on a portable digital recorder (Digitrapper Mk III; Synectics Medical). Before each study, the pH probe was calibrated in buffer solutions of pH 7 and 1. An episode of acid reflux was defined as a decrease in oesophageal pH to <4 for more than 10 seconds.23,25
Measurement of duodeno-gastro-oesophageal reflux
The fibreoptic spectrophotometer Bilitec 2000 (Synectics) was used to quantify duodeno-gastro-oesophageal reflux. The system consists of a miniaturised probe of 1.5 mm diameter that carries light signals into the oesophagus and back via a plastic fibreoptic bundle. Before each study, the probe was calibrated in water. An episode of duodenal reflux is defined as an increase in oesophageal bilirubin absorbance of >0.14 for more than 10 seconds.23,25
Combined pH and duodenal reflux monitoring
Probes for assessing acid and duodeno-gastro-oesophageal reflux were introduced via a nasal orifice into the oesophagus 5 cm proximal to the lower oesophageal sphincter, defined by stationary oesophageal manometry. The probes were then attached with adhesive tape to the subject’s nose and cheek. In addition, appropriate positioning in the oesophagus was confirmed by fluoroscopy. Data collection devices were connected to the probes and worn on a belt on the patient’s waist. Registration of acid or duodeno-gastro-oesophageal reflux lasted for approximately 22 hours after which the probes were removed and the data transferred to a personal computer for analysis. Patients recorded the time of food or fluid consumption and posture changes on a diary card. They were instructed to stay upright during the day. During the recording time, only liquid meals (200 ml Nutridrink; 300 kcal: 13% proteins, 48% carbohydrates, and 39% lipids; Nutricia, Belgium), not interfering with Bilitec monitoring, were allowed.23 Patients were asked to preferably drink water and to avoid coffee, tea, and fruit juices during the recording.
Data analysis
Data were analysed with the aid of commercially available software (Gastrosoft Inc.; Synectics Medical, Irvine, Texas, USA). Acid and duodenal reflux were quantified separately with the following variables obtained from computerised analysis: number of reflux episodes, number of reflux episodes lasting longer than five minutes, and fraction of time of acid or duodeno-oesophageal reflux. The recording was divided into meal, postprandial (two hours after a meal), interdigestive, upright, and supine periods. Individual severity scores (0–3) for 14 reflux related symptoms were obtained from the questionnaire. An overall severity score (maximum score 42) was calculated by adding the severity scores of all individual symptoms in the questionnaire. We also determined the maximum individual severity score for each patient, before and after addition of baclofen.
Statistical analysis
Values are expressed as mean (SEM) for parametric data, and median (interquartile range) for non-parametric data. Data were compared using the Student’s t test, the Mann-Whitney U test, or χ2 test, wherever appropriate. A p value of <0.05 was considered significant.
RESULTS
Patient characteristics
Sixteen patients (five men, 11 women) with persistent heartburn or regurgitation in spite of omeprazole 20 mg twice daily for at least three months were included in the study after written informed consent was obtained. Mean age of the patients was 46.2 (2.8) years and mean body mass index was 28.3 (1.9) kg/m2. Eight patients were smokers and one patient reported regular use of alcohol.
Endoscopy
In all patients the endoscopic investigation took place before the 24 hour measurements. In nine patients no oesophageal lesions were found. According to the modified Savary and Miller classification, oesophagitis grade 1 was seen in five patients (31%) and oesophagitis grade 2 in two patients (13%). None of the patients was diagnosed with Barrett’s oesophagus and in three patients (19%) a hiatal hernia was found.
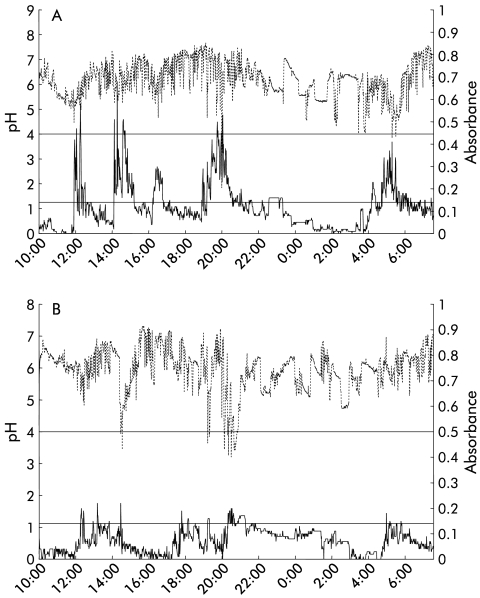
Bilitec and pH measurements under omeprazole treatment
Under omeprazole therapy alone (20 mg twice daily), all patients had normal oesophageal acid exposure (table 1 ▶, fig 1A ▶). On average, intraoesophageal pH was <4 for only 0.3 (0.05; 2.2)% of the recording time. Patients had 14 (2; 51) acid reflux episodes, none of which lasted longer than five minutes. The acid reflux that persisted during omeprazole therapy occurred almost exclusively in the upright position (table 1 ▶).
Table 1.
Acid exposure parameters during treatment with omeprazole 20 mg twice daily and with omeprazole 20 mg twice daily plus baclofen 10 mg three times daily
| Variable | Period | Omeprazole | Omeprazole + baclofen | p Value |
| % Time pH <4 | Total | 0.3 (0.05; 2.2) | 0.4 (0.15; 2.3) | NS |
| Upright | 0.4 (0; 2.9) | 0.7 (0.25; 1.8) | NS | |
| Supine | 0 (0; 0) | 0 (0; 0.2) | NS | |
| No of acid reflux episodes | Total | 14 (2; 52) | 17 (7; 36) | NS |
| Upright | 12 (2; 23.2) | 17.5 (6.7; 31.2) | NS | |
| Supine | 0 (0; 1.5) | 0.5 (0; 3) | NS | |
| No of acid reflux episodes lasting >5 min | Total | 0 (0; 0.5) | 0 (0; 0) | NS |
| Upright | 0 (0; 0) | 0 (0; 0) | NS | |
| Supine | 0 (0; 0) | 0 (0; 0) | NS |
Values are median (interquartile range).
Figure 1.
Combined pH and Bilitec monitoring studies. The x axis depicts time, the left y axis depicts intraoesophageal pH, and the right y axis depicts bilirubin absorbance. Cut offs of the normal ranges are indicated (pH <4 and absorbance >0.14). (A) Combined pH and Bilitec monitoring in a patient with typical reflux symptoms during omeprazole 20 mg twice daily treatment, showing normal acid exposure and pathological duodenal reflux exposure. (B) Combined pH and Bilitec monitoring during omeprazole 20 mg twice daily and baclofen 20 mg three times daily treatment, showing normal acid exposure and normalised duodenal reflux exposure.
As required by the inclusion criteria, all patients had pathological oesophageal Bilitec recordings while they were taking omeprazole 20 mg twice daily (table 2 ▶) On average, the distal oesophagus was exposed to duodenal reflux for 13.8 (11.8; 15.5)% of the time. Patients had 24 (14; 34) episodes of non-acid reflux, of which 5 (3; 8) lasted longer than five minutes. The majority of duodenal reflux episodes occurred in the upright position (17 (10; 25) episodes, amounting to exposure to duodenal reflux of 16 (10.9; 21.9)% of the time). In the supine position, 5 (1; 8) episodes of duodenal reflux resulted in 11.2 (0.9; 18.4)% of the time exposure to duodenal reflux (table 2 ▶).
Table 2.
Duodenal reflux exposure parameters during treatment with omeprazole 20 mg twice daily and with omeprazole 20 mg twice daily plus baclofen 10 mg three times daily
| Variable | Period | Omeprazole | Omeprazole + baclofen | p Value |
| % Time absorbance >0.14 | Total | 13.8 (11.8; 15.5) | 6.1 (0.8; 10.4) | <0.005 |
| Upright | 16 (10.9; 21.9) | 8.6 (1.3; 16.4) | 0.06 | |
| Supine | 11.2 (0.9; 18.4) | 0 (0; 1.1) | <0.05 | |
| No of duodenal reflux episodes | Total | 23 (14.5; 33) | 12 (5; 21) | 0.06 |
| Upright | 17 (10; 25) | 12 (1; 20) | 0.07 | |
| Supine | 4.5 (0.7; 8.2) | 0 (0; 0) | <0.05 | |
| No of duodenal reflux episodes lasting >5 min | Total | 5 (3; 8) | 2 (0.5; 4.5) | <0.05 |
| Upright | 4 (2.5; 5) | 2 (0.5; 4) | 0.06 | |
| Supine | 2 (0.5; 2) | 0 (0; 0) | <0.05 |
Values are median (interquartile range).
Bilitec and pH measurements during treatment with omeprazole and baclofen
Under combined treatment with omeprazole 20 mg twice daily and baclofen 20 mg three times daily, oesophageal acid exposure remained unchanged (table 1 ▶, fig 1B ▶). On average, intraoesophageal pH was below 4 for 0.4 (0.15; 2.3)% of the recording time. Patients had 17 (7; 36) acid reflux episodes, none of which lasted longer than five minutes. The persisting acid reflux occurred almost exclusively in the upright position (table 2 ▶).
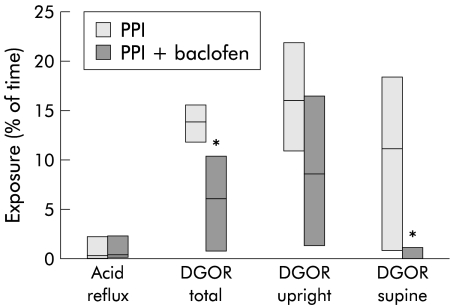
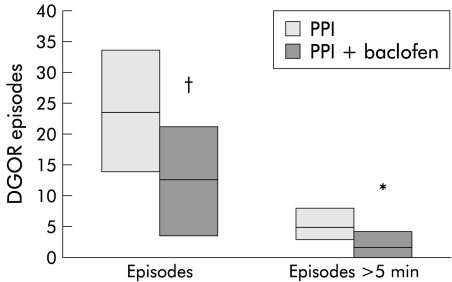
After addition of baclofen 20 mg three times daily to omeprazole 20 mg twice daily, distal oesophageal exposure duodenal reflux was significantly decreased to 6.1 (0.8;10.4)% of the time (p<0.05) (fig 2 ▶). The number of duodenal reflux episodes and the number of duodenal reflux episodes lasting longer than five minutes were significantly decreased (table 2 ▶, fig 3 ▶). Decreases in duodenal reflux exposure during baclofen treatment occurred both in the upright and supine positions but changes in supine duodenal reflux were most pronounced (table 2 ▶).
Figure 2.
Acid and duodenal reflux exposure during treatment with omeprazole 20 mg twice daily and during omeprazole 20 mg twice daily (PPI) plus baclofen 20 mg three times daily. PPI, proton pump inhibitor; DGOR, duodeno-gastro-oesophageal reflux. *p<0.05.
Figure 3.
Number of duodenal reflux episodes (DGOR) and number of duodenal reflux episodes lasting longer than five minutes during treatment with omeprazole 20 mg twice daily (PPI) and during omeprazole 20 mg twice daily plus baclofen 20 mg three times daily. *p<0.05; †p<0.06.
Symptom assessment and side effects
Symptom severity at baseline is summarised in table 3 ▶. During treatment with omeprazole 20 mg twice daily, overall symptom severity was 10.3 (1.7). The most prevalent symptoms were chest pain, heartburn, nausea, throat ache, odynophagia, and acid regurgitation. After addition of baclofen, overall symptom severity was significantly decreased to 5.8 (1.3) (p<0.01). Maximum symptom severity decreased from 26 (0.1) to 1.8 (0.3) (p<0.03). The severity of heartburn, odynophagia, and choking was significantly decreased (p<0.05) and a borderline decrease in the severity of throat ache occurred (p = 0.07) (table 3 ▶).
Table 3.
Symptom severity scores during treatment with omeprazole 20 mg twice daily and during omeprazole 20 mg twice daily plus baclofen 10 mg three times daily
| Symptom | Omeprazole | Omeprazole+baclofen | p Value |
| Heartburn | 1.6 (0.4) | 0.8 (0.3) | <0.05 |
| Acid regurgitation | 0.7 (0.2) | 0.6 (0.3) | NS |
| Food regurgitation | 0.4 (0.2) | 0.4 (0.2) | NS |
| Chest pain | 1.7 (0.3) | 1.1 (0.3) | NS |
| Dysphagia | 0.5 (0.2) | 0.4 (0.2) | NS |
| Nausea | 1.3 (0.3) | 0.9 (0.2) | NS |
| Choking | 0.6 (0.3) | 0.1 (0.1) | <0.05 |
| Odynophagia | 0.8 (0.3) | 0.1 (0.1) | 0.01 |
| Throat ache | 1.1 (0.3) | 0.6 (0.3) | 0.07 |
| Hoarseness | 0.5 (0.3) | 0.4 (0.2) | NS |
| Coughing | 0.4 (0.2) | 0.1 (0.1) | NS |
| Dyspnoea | 0.3 (0.2) | 0.1 (0.1) | NS |
| Vomiting | 0.5 (0.3) | 0.4 (0.2) | NS |
| Overall | 10.3 (1.7) | 5.8 (1.3) | <0.01 |
Values are mean (SEM).
Treatment with baclofen was generally well tolerated. Mild side effects occurring in four patients were transient nausea (n = 2) and drowsiness (n = 3). No dose reductions were necessary and none of the patients withdrew from the study.
DISCUSSION
In a subset of GORD patients, typical reflux symptoms persist in spite of PPI therapy. In up to half of the patients, ongoing non-acid reflux, for which treatment options are limited, can be demonstrated.13–15 The present study was a pilot study to investigate the value of add-on treatment with baclofen in patients with adequate control of acid reflux by a PPI but who had persisting reflux symptoms and ongoing duodenal reflux. We demonstrated that addition of the GABAB agonist baclofen reduced the number of duodenal reflux episodes and the duodenal reflux exposure that persists during PPI therapy. This effect occurred during a short term treatment course, demonstrating that the favourable effect of baclofen in GORD is preserved during repeated administrations. We also observed improvement in persistent reflux symptom, be it in an uncontrolled setting.
The prerequisite for gastro-oesophageal reflux to occur is failure of the antireflux barrier at the gastro-oesophageal junction. In healthy subjects and in most patients with mild to moderate GORD, both acid and non-acid reflux occurs, mainly during TLOSRs.17–20 Pharmacological intervention to reduce TLOSRs has been proposed as a non-surgical strategy to improve the antireflux barrier in patients with GORD, and several agents that inhibit the occurrence of TLOSRs were identified, including atropine, CCKA receptor antagonists, morphine, and nitric oxide synthase inhibitors.27 None of these agents has had clinical application in GORD therapy because of an unfavourable pharmacological profile.
More recently, administration of a single 40 mg dose of the GABAB agonist baclofen was shown to inhibit TLOSRs and to increase basal LOS pressure, thereby significantly decreasing acid reflux after a meal in healthy controls.22 In GORD patients, acute administration of 40 mg baclofen inhibited postprandial TLOSRs, without significantly affecting oesophageal acid exposure.23 Oesophageal peristalsis was not altered by baclofen in any of these studies. These observations suggest a therapeutic potential for baclofen in the inhibition of TLOSR related acid reflux events. However, currently available acid suppressive therapy is also most successful in patients with mild to moderate reflux disease with predominantly upright TLOSR related reflux episodes.3,4,11,12 As baclofen addresses a different factor of GORD pathophysiology, baclofen or related agents offer the potential to be used as add-on therapy in GORD patients with incomplete relief by acid suppression and/or in patients with more severe GORD.
In the present study, we used baclofen as add-on therapy in GORD patients with duodenal reflux that persisted during PPI treatment, confirming its therapeutic potential in treating duodenal reflux in a longer term setting. The dose of baclofen was progressively increased to 20 mg three times daily after 10 days. Re-evaluation after 14 days of baclofen treatment confirmed a significant decrease in the number of duodenal reflux episodes and a significant decrease in oesophageal duodenal reflux exposure. In keeping with putative inhibition of TLOSRs by baclofen, the number of reflux events and duodenal reflux exposure were decreased during the 24 hour period studied. Contrary to expectations, this beneficial effect was less pronounced in the upright period, and most prominent during the supine period. It is unclear whether this is related to inhibition of TLOSRs, or whether the increase in basal LOS pressure that was described in previous studies22,23 contributes to this effect. Reflux during TLOSRs depends on the characteristics of the gastric contents. With adequate acid suppression, patients will have no acid in the stomach, but duodenogastric reflux is unlikely to be affected. Previous studies have already established the high prevalence of duodeno-gastric reflux in the supine position.28 As a consequence, during PPI therapy, nocturnal TLOSRs are readily associated with duodenal refluxate. During the night, reflux due to TLOSRs occurs during episodes of arousal.29 Baclofen therefore may have reduced the number of nocturnal TLOSRs or the number of nocturnal arousal episodes, thereby decreasing nocturnal duodenal reflux episodes.
Furthermore, a decrease in the number of reflux events seems insufficient to explain all of the changes in duodenal reflux exposure. Treatment with baclofen significantly decreased the number of duodenal reflux episodes that lasted longer than five minutes. This could reflect improved oesophageal clearance of duodenal refluxate or decreased volume of the refluxate. The mechanisms involved in clearance of non-acid reflux are incompletely elucidated but previous studies using baclofen failed to show altered oesophageal peristaltic activity.22,23 Regarding the volume of the refluxate, it will be important to study the effects of baclofen on gastric emptying and on duodeno-gastric reflux episodes. Inhibition of vagal efferent activity by baclofen is likely to decrease vagally driven acid secretion, thereby also decreasing intragastric fluid volumes.30 It is unclear whether such a mechanism might still be of relevance during PPI therapy.
Apart from improving Bilitec measurements of duodenal reflux exposure, baclofen also improved a composite score of typical and atypical reflux symptoms, as well as some individual symptoms, such as heartburn, odynophagia, and choking. These findings are encouraging in a particularly difficult group of patients to manage, but confirmation of a clinically relevant effect of baclofen on refractory GORD symptoms awaits placebo controlled long term studies.
In summary, in the present study, the GABAB receptor agonist baclofen was shown to reduce symptoms and duodenal reflux in patients with insufficient relief during PPI therapy. These observations confirm that baclofen can inhibit reflux during repeated administration and suggest a therapeutic potential as an add-on in GORD patients with incomplete relief by acid suppression.
Abbreviations
GORD, gastro-oesophageal reflux disease
TLOSR, transient lower oesophageal sphincter relaxation
GABA, gamma-aminobutyric acid
PPI, proton pump inhibitor
REFERENCES
- 1.Isolauri J, Laippala P. Prevalence of symptoms suggestive of gastroesophageal reflux disease in an adult population. Ann Med 1995;27:67–70. [DOI] [PubMed] [Google Scholar]
- 2.Spechler SJ. Epidemiology and natural history of gastroesophageal reflux disease. Digestion 1992;51(suppl 1):24–9. [DOI] [PubMed] [Google Scholar]
- 3.Dehn TC, Sheperd HA, Colin-Jones D, et al. Double blind comparison of omeprazole versus cimetidine in the treatment of symptomatic erosive reflux oesophagitis, assessed endoscopically, histologically and by 24 h pH monitoring. Gut 1990;31:509–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hetzel DJ, Dent J, Reed WD, et al. Healing and relapse of severe peptic esophagitis after treatment with omeprazole. Gastroenterology 1988;95:903–12. [DOI] [PubMed] [Google Scholar]
- 5.Klinkenberg-Knol E, Nelis F, Dent J, et al. Long-term omeprazole treatment in resistant gastroesophageal reflux disease: efficacy, safety and influence on gastric mucosa. Gastroenterology 2000;118:661–9. [DOI] [PubMed] [Google Scholar]
- 6.Robinson M, Campbell DR, Sontag S, et al. Treatment of erosive reflux esophagitis resistant to H2-receptor antagonist therapy. Lansoprazole, a new proton pump inhibitor. Dig Dis Sci 1995;40:590–7. [DOI] [PubMed] [Google Scholar]
- 7.Marshall RE, Anggiansah A, Manifold DK, et al. Effect of omeprazole 20 mg twice daily on duodenogastric and gastro-oesophageal bile reflux in Barrett’s esophagus. Gut 1998;43:603–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Menges M, Muller M, Zeitz M. Increased acid and bile reflux in Barrett’s esophagus compared to reflux esophagitis, and effect of proton pump inhibitor therapy. Am J Gastroenterol 2001;96:331–7. [DOI] [PubMed] [Google Scholar]
- 9.Stein HJ, Kauer WK, Feussner H, et al. Bile reflux in benign and malignant Barrett’s esophagus: effect of medical acid suppression and Nissen fundoplication. J Gastrointest Surg 1998;2:333–41. [DOI] [PubMed] [Google Scholar]
- 10.Champion G, Richter JE, Vaezi MF, et al. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett’s esophagus. Gastroenterology 1994;107:747–54. [DOI] [PubMed] [Google Scholar]
- 11.Holloway RH, Dent J, Narielvala F, et al. Relation between oesophageal acid exposure and healing of oesophagitis with omeprazole. Gut 1996;38:649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klinkenberg-Knol EC, Meuwissen SGM. Combined gastric and esophageal 24-hour pH monitoring and esophageal manometry in patients with reflux disease resistant to treatment with omeprazole. Aliment Pharmacol Ther 1990;4:485–95. [DOI] [PubMed] [Google Scholar]
- 13.Tack J, Koek G, Demedts I, et al. Gastro-esophageal reflux disease poorly responsive to proton pump inhibitors: acid reflux, bile reflux or both? 2002(submitted for publication). [DOI] [PubMed]
- 14.Wilmer A, Tack J, Frans E, et al. Duodenogastroesophageal reflux and esophageal mucosal injury in mechanically ventilated patients. Gastroenterology 1999;116:1293–9. [DOI] [PubMed] [Google Scholar]
- 15.Vela M, Camacho-Lobato L, Srinivasan R, et al. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology 2001;120:1599–606. [DOI] [PubMed] [Google Scholar]
- 16.Vaezi MF, Sears -R, Richter JE. Placebo-controlled trial of cisapride in postgastrectomy patients with duodenogastroesophageal reflux. Dig Dis Sci 1996;41:754–63. [DOI] [PubMed] [Google Scholar]
- 17.Dodds WJ, Dent J, Hogan WJ, et al. Mechanisms of gastroesophageal reflux in patients with reflux esophagitis. N Engl J Med 1982;307:1547–52. [DOI] [PubMed] [Google Scholar]
- 18.Schoeman MN, Tippett MD, Akkermans LMA, et al. Mechanisms of gastroesophageal reflux in ambulant healthy human subjects. Gastroenterology 1995;108:83–91. [DOI] [PubMed] [Google Scholar]
- 19.Penagini R, Schoeman MN, Dent J, et al. Motor events underlying gastro-esophageal reflux in ambulant patients with reflux esophagitis. Neurogastroenterol Mot 1996;8:131–41. [DOI] [PubMed] [Google Scholar]
- 20.Sifrim D, Holloway R, Silny J, et al. Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am J Gastroenterol 2001;96:647–55. [DOI] [PubMed] [Google Scholar]
- 21.Lidums I, Lehmann A, Checklin H, et al. Control of transient lower esophageal sphincter relaxations and reflux by the GABA(B) agonist baclofen in normal subjects. Gastroenterology 2000;118:7–13. [DOI] [PubMed] [Google Scholar]
- 22.Zhang Q, Lehmann A, Checklin H, et al. Control of transient lower oesophageal relaxations and reflux by the GABAB agonist baclofen in patients with gastro-oesophageal reflux disease. Gut 2002;50:19–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tack J, Koek GH, Bisschops R, et al. Dietary restrictions during ambulatory monitoring of duodeno-gastro-esophageal reflux. Dig Dis Sci 2003;48:1213–20. [DOI] [PubMed] [Google Scholar]
- 24.Savary M, Miller G. L’oesophage. Manuel et Atlas d’Edoscopie.. Solothurn, Switzerland: Verlag Gassmann, 1977.
- 25.Cuomo R, Koek G, Sifrim D, et al. Analysis of ambulatory duodeno-gastro-esophageal reflux monitoring. Dig Dis Sci 2001;45:2463–9. [DOI] [PubMed] [Google Scholar]
- 26.Hirschowitz BI. A critical analysis, with appropriate controls, of gastric acid and pepsin secretion in clinical esophagitis. Gastroenterology 1991;101:1149–58. [DOI] [PubMed] [Google Scholar]
- 27.Holloway RH, Dent J. Medical treatment of gastroesophageal reflux disease—beyond the proton pump inhibitors. Dig Dis 2000;18:7–13. [DOI] [PubMed] [Google Scholar]
- 28.McDermott CM, Abrahams TP, Partosoedarso E, et al. Site of action of GABA(B) receptor for vagal motor control of the lower esophageal sphincter in ferrets and rats. Gastroenterology 2001;120:1749–62. [DOI] [PubMed] [Google Scholar]
- 29.Freidin N, Fisher MJ, Taylor W, et al. Sleep and nocturnal acid reflux in normal subjects and patients with reflux oesophagitis. Gut 1991;32:1275–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marshall RE, Anggiansah A, Owen WA, et al. The extent of duodenogastric reflux in gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol 2001;13:5–10. [DOI] [PubMed] [Google Scholar]