Abstract
Background: Irritable bowel syndrome (IBS) is a heterogeneous condition which is diagnosed according to specific bowel symptom clusters. The aim of the present study was to identify subgroups of IBS subjects using measures of rectal sensitivity and psychological symptoms, in addition to bowel symptoms. Such groupings, which cross conventional diagnostic approaches, may provide greater understanding of the pathogenesis of the condition and its treatment.
Method: A K means cluster analysis was used to group 107 clinic patients with IBS according to physiological, physical, and psychological parameters. All patients had severe IBS and had failed to respond to usual medical treatment. Twenty nine patients had diarrhoea predominant IBS, 26 constipation predominant, and 52 had an alternating bowel habit.
Results: The clusters were most clearly delineated by two variables: “rectal perceptual threshold (volume)” and “number of doctor visits”. Three subgroups were formed. Group I comprised patients with low distension thresholds and high rates of psychiatric morbidity, doctor consultations, interpersonal problems, and sexual abuse. Group II also had low distension thresholds but low rates of childhood abuse and moderate levels of psychiatric disorders. Group III had high distension thresholds, constipation or alternating IBS, and low rates of medical consultations and sexual abuse.
Conclusion: The marked differences across the three groups suggest that each may have a different pathogenesis and respond to different treatment approaches. Inclusion of psychosocial factors in the analysis enabled more clinically meaningful groups to be identified than those traditionally determined by bowel symptoms alone or rectal threshold.
Keywords: irritable bowel disease, rectal sensitivity, sexual abuse, interpersonal problems
Irritable bowel syndrome (IBS), by definition a cluster of symptoms without recognised aetiopathology, is a heterogeneous condition in which a variety of different biological, psychological, and social factors are likely to be implicated.1,2 Identification of meaningful subgroups of patients within this syndrome is therefore important as these groups may represent different aetiological and pathophysiological entities,3 and they may require different treatment approaches.4
Several attempts have been made to delineate subgroups of IBS based on a variety of different parameters including: pattern of symptoms;3 severity of symptoms;5 visceral hyperalgesia;6,7 intestinal transit;8 contractile and myoelectrical activity;9–12 and psychological factors (psychiatric disorder,13 sexual abuse,14 and life stress15). However, to date no subclassification has emerged as having sufficient practical utility to either enhance aetiological understanding or influence management. It is also probable that combinations of factors may be more aetiologically relevant than single factors alone. For example, the development of chronic symptoms post infection with Campylobacter may require both a gastrointestinal infection and the influence of psychological factors16 whereas for community subjects with bowel symptoms, psychological factors may play a less significant role.17–19
The development of the ROME criteria20 and the absence of biological markers has focused most attention on the categorisation of IBS according to bowel symptoms. The ROME criteria have helped to standardise therapeutic trials in IBS. However, delineation of subgroups based on several factors, additional to bowel symptoms, may help to identify more specific subgroups.
In the present study, we chose to focus on patients with IBS at the severe end of the spectrum; those with severe symptoms, who had failed to respond to routine treatment. From previous research, we would expect approximately half of these patients to suffer from psychiatric disorders.21,22 Thus they are an ideal group in which to study relationships between gut symptoms, physiology, and psychological disorders.
The aim of the present study was to use the statistical method of cluster analysis to identify subgroups from among such a group of IBS patients using factors, previously identified in the literature, as being of relevance in the pathogenesis of IBS. Thus this was a hypothesis generating study as opposed to one in which a specific hypothesis was tested.
SUBJECTS AND METHODS
This study formed the initial part of a large randomised controlled trial of the cost effectiveness of psychological treatment in intractable IBS. Patients who agreed to participate in the study were assessed at baseline and measures of rectal sensitivity, psychopathology, and bowel symptoms were obtained. They were then randomly allocated to one of three different 12 week treatment interventions with brief psychotherapy, an antidepressant, or treatment as usual, after which some of the measures were repeated. Details of the outcome of the trial have been reported elsewhere.23 This study focuses on the relationship between different baseline characteristics of the patients on entry to the study.
Patients with treatment resistant IBS
All patients who took part in the study were chronic clinic attenders (symptoms for at least six months) who had failed to respond to conventional treatment for IBS by gastroenterologists. Recruitment took place from clinics in seven hospitals in Northern England; three teaching hospitals and four district general hospitals. Clinic lists and hospital notes were screened to identify potential patients who were then assessed by a consultant gastroenterologist. They were therefore representative of a clinical treatment resistant IBS population. Patients enrolled in the study were aged between 18 and 65 years, fulfilled the ROME I criteria for IBS20 after physical examination and routine investigation, and were able to understand and complete the study questionnaires. Other entry criteria were: symptoms for more than six months, resistance to medical treatment, a pain severity score of >59 on a 0–100 visual analogue scale of a typical pain episode, and lack of contraindication to any of the two proposed treatments in the cost effectiveness trial (that is, the specific serotonergic reuptake inhibitor paroxetine or psychotherapy).
Normal controls
Twenty three healthy subjects (17 females and six males; mean age 32.4 years (range 20–45)) were recruited by advertisements placed in the local hospitals and the university. None of the subjects suffered from gastrointestinal symptoms. The results from these subjects were used to establish local 95% confidence intervals for rectal perception threshold.
Ethics committee approval was obtained for each hospital taking part in the study. Patients signed written consent to participate in the study after the trial had been verbally explained and they had read information sheets about the study. Additional consent was sought for participation in rectal threshold measurements.
Bowel symptom assessments
Bowel symptom questionnaire
Patients completed a previously validated bowel symptom questionnaire24 from which their bowel habit was classified according to ROME criteria as diarrhoea predominant, constipation predominant, or alternating.20 All patients had continuous or recurrent symptoms of: (1) abdominal pain, with one or more of the following: abdominal pain relieved with defecation, often (at least 25% of the time); and associated with change in frequency of stool often (more/less bowel movements with pain) or consistency of stool (hard or loose) with pain often; (2) at least two of the following: irregular pattern of defecation (more than three bowel openings daily or less than three per week); altered stool consistency (either hard or loose stool) often; incomplete rectal evacuation often and/or urgency often or straining often; abdominal bloating or distension often; and/or mucus in stools. In addition, all patients in the study had to have suffered symptoms for at least six months, have been unresponsive to previous treatment, and have severe abdominal pain, defined as >59 on a visual analogue scale. The questionnaire also included two ratings of abdominal pain: “pain today” and “typical pain” (using a linear analogue scale, anchored between descriptors of no pain (0) and worst ever pain (100)). A functional bowel severity index can be calculated based on the severity of pain and frequency of medical consultations.25 This was calculated using the following formula: current pain on the visual analogue scale (pain today) (0–100) plus (the number of doctor visits multiplied by 11). Patients with chronic functional abdominal pain were not included in the trial.
Bowel symptom diary
Patients kept a two week diary rating of 11 symptoms on a 0–6 Likert scale (abdominal pain, bloating, straining, mucus, incomplete evacuation, urgency, wind, hard stool, loose stool, frequency of motions, and nausea). The descriptors were: no problem=0, very mild=1, mild=2, moderate=3, severe=4, very severe=5, and worst possible=6. They completed this for two weeks prior to the assessment of rectal sensitivity. The mean score of each item for the two week period was calculated.
Psychological assessments
Presence of psychiatric disorders
Patients completed a detailed psychiatric assessment interview: Schedules for Clinical Assessment in Neuropsychiatry (SCAN).26 This interview lasts approximately 1–2 hours and enables a psychiatric diagnosis to be made according to ICD-10.27
Severity of psychological symptoms
Psychological distress was measured using the SCL-90-R.28 This consists of 90 items related to psychological distress. Each item is rated on a five point scale from 0 (not at all) to 4 (extremely). One of the items (item 40) “nausea or upset stomach” could be caused by either anxiety or bowel problems. For this reason, analyses using this measure were repeated with the item excluded to determine whether this had an impact on the results. Severity of depression was measured using the Hamilton depression rating scale (HDRS).29
History of sexual abuse
This was assessed using a validated screening questionnaire developed by Leserman and colleagues.30 The questionnaire consists of short questions about exposure, threat of sex, subjects touching and being touched, rape, and incest.
Interpersonal difficulties
Interpersonal difficulties were measured using the Inventory of Interpersonal Problems (short version) (IIP-32).31 This is a brief version of the Inventory of Interpersonal Problems.32 It comprises 32 self report items, and has good reliability and is sensitive to change.31
Quality of life
Health related quality of life was measured by the patient completing theSF-36.33 Data are provided as physical and mental component scores.34 The mean score on each for the general population is 50, with a standard deviation of 10. Low scores on this measure indicate poor health status and high scores indicate good health status.
Physiological assessments
Sensory responses to rectal distension were assessed in the manner previously reported in detail by Whitehead and colleagues.35 This method was designed to minimise anticipatory anxiety in subject undergoing the procedure, as the subject is unable to predict the sequence of balloon inflations. Each subject was invited to open his/her bowels if he/she felt the need to do so. S/he then lay in the left lateral decubitus position with hips and knees bent while a well lubricated tube (4 mm outer diameter), which incorporated a 17 cm2 non-compliant polyvinyl chloride bag (maximum capacity 1200 ml), attached between 9 and 19 cm from the catheter tip, and manometry ports sited at 2, 7, and 14 cm, was gently inserted into the rectum and positioned so that the distal pole of the bag was 5 cm from the anal verge. After insertion, the bag was inflated with 20 ml of air to separate the bag from the pressure sensor, and a “recovery” period was allowed until subjects reported no sensation of rectal distension, usually 10–15 minutes. The intrabag pressure was then set at 10 mm Hg using a computerised pump system (Synectics Visceral Stimulator; Medtronic-Synectics, Stockholm, Sweden) and rectal volume was recorded to provide a baseline index of rectal tone. The pump was then set to provide automated bag inflation sequences at a rate of 38 ml/s in 2 mm Hg steps, according to a double random staircase paradigm. Recordings were made of: (1) inflation pressure (mm Hg); (2) intrabag pressure (mm Hg); and (3) intrabag volume (ml).
Twenty five seconds into every inflation, triggered by an audible signal, the subject was asked to describe the sensation experienced (for example, like the presence of gas or stool) and its intensity. When the discomfort occurred, they were requested to press the keypad which triggered the system to switch to a tracking mode in which the next intrabag pressure stimulus would either be the same or 2 mm Hg lower than the stimulus that generated the discomfort. Two random sequences of inflation (random staircases) were conducted, the system switching between the two staircases in random fashion throughout the procedure. When discomfort had been signalled in each of the two staircases, the system automatically stopped the procedure.
Measurements used for analysis were average values of pressure and volume during the last 10 seconds of each of the distensions that caused discomfort, in both staircases.
Statistical analysis
Baseline data were analysed using parametric statistics, and are expressed as mean (SEM) values. Using the whole data set, Pearson correlation coefficients were used to explore linear relationships between different continuous variables. A K means cluster analysis was used to group patients according to physiological parameters, and physical and psychological symptoms.36 This method is exploratory and we had no preconceived ideas about how patients would cluster together. The technique aims to group subjects such that the distance between subjects within a group is minimised and the distance between the group centres is maximised. It does this using Euclidean distance measures in K dimensional space, where K is the number of different variables considered. In other words, it aims to put similar subjects in the same group. It does this in a hierarchical way such that the nearest (that is, most similar) two subjects are first put into a group. The two, three, and four group solutions were all explored.
The three cluster solution had the best fit to the data. The validity of the three subgroup solution was explored by comparing subgroup membership across physiological, physical, and psychological symptom measures, using ANOVA or χ2 tests, as appropriate. Significance was defined as p<0.05 for all tests, unless stated otherwise in the text.
For the purposes of comparison with previous research, patients were then categorised according to their threshold scores into hypersensitive, normosensitive, and hyposensitive groups, using data from normal controls to define the threshold scores. All analyses were carried out using SPSS for Windows, version 10.1.
RESULTS
A total of 176 patients were invited to undergo all assessments but 69 patients declined to participate in measurements of rectal sensitivity. Data are therefore presented on 107 patients who completed all the assessments. There was no significant difference in baseline measures of bowel symptoms, psychological symptoms, or demographic variables between those patients who agreed and those who declined to participate in the rectal distension study.
Of the 107 patients, 88 (82%) were female and 70 (65%) were married or cohabiting. Patients had suffered from IBS for a mean of 12 years (SD 9.3) and 13 (12%) were in receipt of incapacity benefit because of their disability.
Bowel symptom questionnaire
Diarrhoea was predominant in 29 patients (27%), constipation was predominant in 26 (24%), and 52 (49%) had an alternating bowel habit.
Bowel symptom diary
Individual diary symptoms which received the highest ratings were abdominal pain (3.0 (SD 1.0)), wind (2.7 (SD 1.3)), and bloating (2.7 (SD 1.3)). Not all patients completed the bowel diary. Table 1 ▶ provides information concerning missing data.
Table 1.
Measures of rectal perceptual thresholds for discomfort, abdominal symptoms, and psychological status in three irritable bowel syndrome subgroups identified by cluster analysis
| Variable | Group I (n=15) | Group II (n=62) | Group III (n=30) | ANOVA for continuous and χ2 for categorical variables | |
| Age (y) | 40.0 (2.8) | 38.7 (1.5) | 42.6 (2.0) | 1.10 | 0.34 |
| % female | 11 (73%) | 54 (87%) | 23 (77%) | 2.45 | 0.29 |
| Bowel symptoms | |||||
| Age at onset of symptoms (y) | 27.5 (2.9) | 27.5 (1.7) | 30.7 (2.2) | 0.68 | 0.51 |
| Duration of symptoms (y) | 12.7 (2.2) | 11.5 (1.3) | 12.0 (1.6) | 0.12 | 0.89 |
| Discomfort threshold | |||||
| Volume (ml) | 66.9 (10.9) | 58.6 (3.4) | 176.1 (9.3) | 104.8 | <0.001***III>I and II |
| Pressure (mm Hg) | 16.6 (2.4) | 12.6 (0.7) | 18.3 (1.5) | 7.6 | <0.001***III>II |
| Rome diagnosis | |||||
| %Constipation | 1 (7%) | 12 (19%) | 13 (43%) | ||
| %Diarrhoea | 5 (33%) | 20 (32%) | 4 (13%) | ||
| %Alternating | 9 (60%) | 30 (48%) | 13 (43%) | 10.51 | 0.033 |
| Functional bowel severity index | 208.3 (8.6) | 93.8 (4.2) | 75.9 (5.7) | 90.2 | <0.001***I>II and III |
| Days in pain per month | 25.8 (1.8)§ | 24.7 (1.1)§§ | 21.4 (1.9)¶ | 1.7 | 0.18 |
| Abdominal pain | |||||
| (typical) | 71.4 (3.2) | 64.8 (2.0) | 66.0 (3.0) | 1.2 | 0.32 |
| (today) | 51.4 (5.8) | 34.2 (2.8) | 25.7 (3.8) | 6.8 | 0.002** I>II and III |
| Diary chart | |||||
| Abdominal pain | 3.3 (0.3)‡ | 3.0 (0.1)†† | 2.9 (0.2)§ | 0.8 | 0.47 |
| Bloating | 2.3 (0.5)‡ | 2.8 (0.2)‡‡ | 2.9 (0.2)§ | 1.0 | 0.36 |
| Straining | 0.8 (0.2)‡ | 1.5 (0.2)‡‡ | 1.4 (0.3)§ | 2.0 | 0.15 |
| Incomplete evacuation | 2.1 (0.4)‡ | 1.8 (0.2)‡‡ | 1.4 (0.3)§ | 1.6 | 0.20 |
| Urgency | 2.7 (0.4)‡ | 1.6 (0.1)‡‡ | 0.8 (0.2)§ | 13.7 | <0.001*** I>II>III |
| Wind | 3.0 (0.5)‡ | 2.6 (0.2)‡‡ | 2.8 (0.3)§ | 0.58 | 0.57 |
| Mucus | 1.1 (0.5)‡ | 0.7 (0.2)‡‡ | 0.6 (0.2)§ | 0.81 | 0.45 |
| Hard stools | 0.7 (0.3)‡ | 1.2 (0.1)¶¶ | 1.1 (0.2)¶ | 0.93 | 0.40 |
| Loose stools | 2.5 (0.4)‡ | 1.8 (0.2)¶¶ | 1.0 (0.2)¶ | 8.3 | <0.001***I and II>III |
| Frequency of motions | 3.2 (0.5)‡ | 2.3 (0.2)‡‡ | 1.1 (0.1)§ | 13.2 | <0.001***I and II>III |
| Nausea | 1.5 (0.3)‡ | 1.4 (0.2)‡‡ | 0.7 (0.2)§ | 3.3 | 0.042* |
| Diary chart mean score | 2.0 (0.2)‡ | 1.9 (0.1)‡‡ | 1.6 (0.1)§ | 2.6 | 0.083 |
| Consultation rates and unemployment | |||||
| No of doctor visits | 14.3 (0.8) | 5.4 (0.3) | 4.6 (0.5) | 77.6 | <0.001*** I>II and III |
| Unemployed | |||||
| %Unemployed-ill health | 7 (47%) | 13 (21%) | 5 (17%) | ||
| %Unemployed | 4 (27%) | 4 (7%) | 2 (7%) | ||
| %Not unemployed | 4 (27%) | 45 (73%) | 23 (77%) | 14.4 | 0.007** |
| Sexual abuse | |||||
| Sexual abuse history | |||||
| %Adult severe | 3 (20%) | 8 (13%) | 3 (10%) | 0.88 | 0.64 |
| %Child any | 6 (40%) | 10 (16%)† | 7 (23%) | 4.02 | 0.13 |
| %Child broad | 6 (40%) | 4 (7%)† | 2 (7%) | 14.32 | 0.001**I>II and III |
| %Child touch | 6 (40%) | 3 (5%)† | 2 (7%) | 16.55 | <0.001*** I>II and III |
| %Child severe | 4 (27%) | 0 (0%)† | 0 (0%) | 25.22 | <0.001*** I>II and III |
| Psychiatric variables | |||||
| %Two or more psychiatric diagnoses | 12 (80%) | 33 (53%) | 11 (37%) | 9.23 | 0.023*I>III |
| %Anxiety disorder | 8 (58%) | 22 (35%) | 2 (7%) | 12.58 | 0.002**I and II>III |
| %Depressive disorder | 5 (33%) | 17 (27%) | 6 (20%) | 1.0 | 0.60 |
| SCL-90-R GSI | 1.0 (0.1) | 1.0 (0.1)‡ | 0.7 (0.1)‡ | 2.9 | 0.06 |
| %Suicidal ideation | 3 (20%) | 1 (2%) | 0.0 | 12.97 | 0.002**I>III |
| %Previous episode of self harm | 4 (27%) | 7 (11%) | 0.0 | 7.87 | 0.02* I>III |
| Hamilton depression rating scale | 14.8 (2.1) | 11.4 (0.8)‡ | 8.9 (0.9)¶ | 4.4 | 0.014* I>III |
| Inventory of Interpersonal Problems-32 | 1.4 (0.2) | 1.2 (0.1)‡ | 0.9 (0.1)¶ | 3.2 | 0.044* |
| Health status | |||||
| SF-36 physical function component score | 32.4 (2.7)† | 37.2 (1.5)‡ | 41.3 (1.7)†† | 3.3 | 0.04* I<III |
| SF-36 mental function component score | 38.1 (3.1)† | 40.5 (1.5)‡ | 41.6 (2.5)†† | 0.4 | 0.66 |
*p<0.05, **p<0.01, ***p<0.001.
Continuous values are shown as means (SEM). Categorical values are shown as number (%). Analyses based on ANOVA for continuous measures and χ2 test for categorical variables.
†Data missing from one subject in this group; ‡data missing from two subjects in this group; §data missing from three subjects in this group; ¶data missing from four subjects in this group; ††data missing from five subjects in this group; ‡‡data missing from six subjects in this group; §§data missing from eight subjects in this group; ¶¶data missing from 13 subjects in this group.
Psychological assessments
Forty seven patients (44%) had a psychiatric diagnosis. The most common conditions were depressive disorders (n=28 (26%)) and anxiety states (n=32 (30%)). The mean GSI score on the SCL-90-R was 0.59 (SD 0.61), which is well above that of the normal population (0.3 (SD 0.3)28). The severity of depression score on the HDRS was 11 (SD 6.5).
History of sexual abuse
Twenty five (23%) per cent reported some form of childhood or adult abuse. Four (4%) reported severe childhood abuse and 14 (13%) reported severe adult abuse. A study of prevalence of childhood sexual abuse in the UK reported a rate of 12% in the general population.37
Perception thresholds
The 95% confidence interval for normal controls for the volume that induced discomfort was 84–138 ml, and pressure 11–14 mm Hg. Sixty patients with IBS had threshold volumes for discomfort of below 84 ml (that is, hypersensitive), 22 patients had values above 84 ml but below 138 ml (that is, normosensitive), and 25 had thresholds above 138.0 ml (that is, hyposensitive).
Subgroups of IBS according to cluster analysis
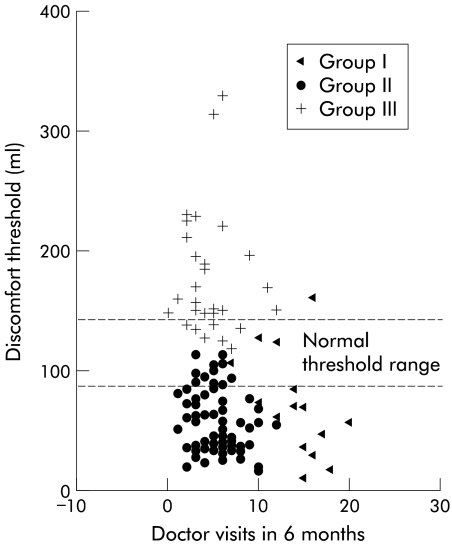
Using the cluster analysis, differentiation into three subgroups provided the clearest delineation. “Discomfort volume” and “number of doctor visits” were the two variables which best discriminated between the three clusters. The scatter plot in fig 1 ▶ shows the distribution of the three groups for these two variables. Comparisons between cluster variables for the three groups are shown in table 1 ▶. Data for the SCL-90-R show the scores based on responses from the 90 items. The data were reanalysed excluding item 40 to determine whether removal of this item (“nausea or upset stomach”) made a difference to the results. There was virtually no difference in the scores or differences between the three groups.
Figure 1.
Volume threshold to discomfort versus medical consultations according to the three clusters: group I, group II, and group III.
A small number of variables were not normally distributed, so comparison between the groups were reanalysed using the Kruskal-Wallis test, followed by Bonferroni corrected pairwise comparisons if the difference between the three groups was found to be significant at the 5% level. The results did not show any substantial differences. The between group p values were 0.64 (duration of symptoms), 0.002, group III>II (pressure), 0.29 (days in pain), 0.99 (mucus), <0.001, group I>III (frequency of motions), 0.034 (nausea), and <0.001, group I>II and III (visits to the doctor).
Group I comprised 15 patients with low distension thresholds, either an alternating or diarrhoea predominant pattern of bowel symptoms, a high prevalence of psychiatric morbidity (particularly complex psychiatric problems involving two or more psychiatric diagnoses and suicidal ideation), high doctor consultation rates, high rates of childhood sexual abuse, high levels of interpersonal difficulties, and low scores on the physical component score of the SF-36.
Patients in group II (n=62) had low thresholds to rectal distension, either an alternating or diarrhoea predominant pattern of bowel symptoms, intermediate rates of psychiatric disorders, and a low prevalence of childhood sexual abuse.
Patients in group III (n=30) had higher thresholds to rectal distension, suffered from constipation predominant IBS or an alternating habit, had lower rates of psychiatric disorders than the other two groups, and low rates of medical consultations, sexual abuse, and interpersonal difficulties.
In relation to the cluster analysis, both the two and four group solutions were also explored. When two groups were specified, this had the effect of combining groups I and II, and when four groups were specified a further group containing just two subjects was formed.
Differences between patients with a low, normal, or high rectal perceptual threshold
The whole data set were then grouped according to their threshold scores into those with low, normal, or high thresholds (that is, a more conventional way of grouping the data). In contrast with the cluster analysis, there were fewer differences between the groups, particularly in relation to psychosocial variables. There were no significant differences between the three groups for any of the abuse variables, percentage unemployed, percentage with two or more psychiatric diagnoses, depression scores (HDRS) or suicidal ideation, interpersonal difficulties, or quality of life.
There was a similar pattern to the cluster analysis in relation to bowel symptom data, with significant differences between the groups for “urgency”(p<0.001 low>normal>high), “loose stools” (p<0.002 low>normal and high), and “frequency of motions” (p<0.002 low>high). According to the Rome diagnoses, constipation predominant IBS was less common in the low threshold group, and diarrhoea predominant IBS was less common in the high threshold group (p=0.033). Anxiety disorders were significantly more prevalent in patients with low or high threshold scores (p=0.01) (low=42%; normal=18%; and high=48%).
DISCUSSION
This study is one of the largest and most detailed investigations of the relationship between bowel symptoms, psychological variables, and rectal sensitivity in IBS.
Cluster analysis produced groupings which appear to be clinically meaningful. We found two groups of patients both of whom had low rectal thresholds and marked psychological symptoms. They were indistinguishable in terms of age, sex, type of IBS, or severity of individual bowel symptoms when measured by diary. However, one group (group I) had a much higher prevalence of childhood sexual abuse, and consulted doctors more frequently. This group was also more likely to have complex psychiatric problems (that is, two or more coexisting psychiatric diagnoses, current suicidal ideation, and a previous history of deliberate self harm), interpersonal difficulties, and be unemployed because of ill health. We have termed this group, “distressed high utilisers”.
Patients in the second group (group II) had low threshold scores and a high prevalence of psychiatric disorders, similar to those in group I. However, they had a much lower prevalence of childhood sexual abuse, were less disabled by their symptoms than group I, and were not frequent consulters. We have termed them “distressed low utilisers”.
Patients in the third subgroup (group III) had high discomfort thresholds, were more likely to suffer from constipation predominant symptoms, and had lower levels of psychological disturbance and interpersonal difficulties than the other groups; particularly anxiety. Group III patients had low consultation rates and complained of less pain. We have termed these patients “tolerant low utilisers”.
The groupings resulting from the cluster analysis produced better discrimination between the patient groups on a greater number of variables than grouping patients according to rectal thresholds. For example, like other investigators,38 we found no relationship between abuse and rectal sensitivity if patients were grouped according to rectal discomfort scores. The cluster analysis however suggested a more subtle relationship between sexual abuse, discomfort threshold, severity of pain, psychiatric complexity, and treatment seeking in a subgroup of IBS patients with low discomfort thresholds.
It has been suggested that two cognitive traits, selective attention to gastrointestinal disease and disease attribution, may contribute to increased pain sensitivity.39,40 It is possible that anxious patients in groups I and II both had increased selective attention to gastrointestinal sensations but, in addition, patients in group I may have had high levels of disease attribution driving them to seek treatment. The psychological measures used in this study did not allow us to determine cognitive processing but further investigation of the specific cognitive processes in each of the three groups we identified will be important.
It was interesting that patients in group I (distressed high utilisers) reported more severe abdominal pain than patients in group II (distressed low utilisers) but their diary bowel chart scores did not differ significantly. This suggests that distressed high utilisers may perceive their pain to be worse when asked to rate it at a particular time point but that the overall severity of their IBS symptoms are no different from others who report much lower degrees of disability and doctor visits (group II). This highlights the problems in assessing the severity of disability when there is no objective measure of the disorder. It also suggests that disability arising from IBS is likely to be related to factors other than the severity of reported pain.
Constipation prone IBS patients have been studied by previous investigators who have suggested there are two subtypes of these patients41: those who have lost the call to stool and have hyposensitivity to slow rectal distension and those who have retained the call to stool and have hypersensitivity. Our tolerant group (group III) showed the greatest overlap with the former of these subtypes. The lack of major psychiatric disturbance in this group raises the question of whether patients’ symptoms may be secondary to a neuromuscular disorder of the colon. This is consistent with recent work which has suggested that the extrinsic autonomic innervation to the gut is disturbed in patients with constipation, and is possibly the primary aetiological factor.42
Both groups I and II had much higher rates of anxiety than group III. Recent study of IBS patients with phobic anxiety has suggested that anxiety may interfere with the processing of visceral information in the frontal cerebral region, providing a possible neurophysiological mechanism for the relationship between psychiatric disorders and perceptual thresholds.43 The findings of the present study suggest such mechanisms may only be relevant for very specific subgroups of IBS patients.
One of the potential uses of the cluster analysis in this study is that the findings suggest that different treatment approaches may be beneficial for the different groups. One can hypothesise that the distressed high utilisers (group I) may benefit most from intensive psychological treatment. The distressed low utilisers may benefit from a combination of psychological treatment and drug treatment for their bowel disorder whereas tolerant low utilisers are most likely to benefit from attention to constipation, and psychological treatments may be of little benefit. Such hypotheses merit testing in controlled studies.
Of immediate relevance to clinicians is the relationship between high consultations and psychiatric comorbidity. Patients who consult frequently should alert the physician to check for comorbid psychiatric disorders and the possibility of sexual abuse. The physician may wish to set aside a specific period of time in the clinic to see such an individual and attempt to develop a rationale for referral to psychiatric services. Patients with diarrhoea who have failed to respond to conventional treatment should also receive a careful assessment to detect anxiety or depression.
There are similarities and differences between the present study and the only previous study of IBS patients in which a cluster analysis was employed.6 Mertz et al also found three subgroups of patients, two of which are similar to our own: a group of hypersensitive patients with diarrhoea predominant IBS and a group of hyposensitive patients with constipation predominant IBS. Their third group however was somewhat different. They found a hypersensitive group of patients who complained of constipation predominant IBS. Mertz et al did not use psychosocial variables in the cluster analysis and their IBS patient population (new attenders at an outpatient clinic) was different to ours. Their work however raises the possibility that there may be further identifiable and clinically relevant subgroups of IBS patients.
Positive aspects of the study include: recruitment of a representative sample of clinic patients with treatment resistant IBS; measurement of bowel symptoms using a validated questionnaire, a detailed symptom diary, and visual analogue rating scales; measurement of psychological status using standardised questionnaires as well as a semi structured interview; and measurement of rectal perceptual thresholds using unbiased methods.
There are three major limitations of the study. Firstly, approximately 40% of patients who were approached declined the rectal sensitivity measures. Although they appeared similar to those who agreed in terms of gastrointestinal symptoms and psychological profile, subtle differences cannot be excluded. Secondly, the study was carried out in secondary and tertiary care centres and therefore the findings should not be generalised to primary care or community subjects with IBS. Finally, it is important to recognise that the clusters identified in this paper apply specifically to severe IBS and should not be extrapolated to the entire spectrum of IBS. It is quite possible that there are other distinct clusters within the IBS population as a whole. The way forward must be to identify specific subgroups for whom specific treatments can be developed and targeted.
Acknowledgments
The Medical Research Council (MRC) of UK financed the study. The North Western Region Health Authority (UK) R&D Directorate financed the psychotherapists. SKB provided paroxetine but were not involved in the design or conduct, or analysis of the trial.
Abbreviations
IBS, irritable bowel syndrome
HDRS, Hamilton depression rating scale
Appendix
North of England IBS Research Group
Chris Babbs, Joe Barlow, Karna Dev Bardhan, Francis Creed, David Dawson, Lakshmi Fernandes, Elspeth Guthrie, Stephanie Howlett, Linda McGowan, Jane Martin, Jim Moorey, Kieran Moriarty, Stephen Palmer, Joy Ratcliffe, Nicholas Read, Wynne Rees, Christine Rigby, Irene Sadowski, Jon Shaffer, David Thompson, Barbara Tomenson, Pierre Willemse.
REFERENCES
- 1.Kellow JE, Delvaux M, Azpiroz F, et al. Principles of applied neurogastroenterology: physiology/motility-sensation. Gut 1999;45(suppl II):II17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drossman DA, Creed FH, Olden KW, et al. Psychosocial aspects of the functional gastrointestinal disorders. Gut 1999;45(suppl II):II25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ragnarsson G, Bodemar G. Division of the irritable bowel syndrome into subgroups on the basis of daily recorded symptoms in two outpatient samples. Scand J Gastroenterol 1999;34:993–1000. [DOI] [PubMed] [Google Scholar]
- 4.Whitehead WE. Patient subgroups in irritable bowelsyndrome that can be defined by symptom evaluation and physical examination. Am J Med 1999;107(suppl 5A):33S–40S. [DOI] [PubMed] [Google Scholar]
- 5.Drossman DA, Whitehead WE, Toner BB, et al. What determines severity among patients with painful functional bowel disorders. Am J Gastroenterol 2000;95:974–80. [DOI] [PubMed] [Google Scholar]
- 6.Mertz H, Naliboff B, Munakata J, et al. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology 1995;109:40–52. [DOI] [PubMed] [Google Scholar]
- 7.Whitehead WE, Palsson OS. Is rectal pain sensitivity a biological marker for irritable bowel syndrome: psychological influences on pain perception. Gastroenterology 1998;115:1263–71. [DOI] [PubMed] [Google Scholar]
- 8.Cann PA, Read NW, Brown C, et al. Irritable bowel syndrome: relationship of disorders in the transit of a sungle solid meal to symptom patterns. Gut 1983;24:405–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Snape WJ, Carlson GM, Cohen S. Colonic myoelectric activity in the irritable bowel syndrome. Gastroenterology 1976;70:326–30. [PubMed] [Google Scholar]
- 10.Taylor I, Derby C, Hammond P. Is there a myoelectrical abnormality in the irritable bowel syndrome? Gut 1978;19:391–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson DG, Laidlow JM, Wingate DL. Abnromal small-bowel motility demonstrated by radiotelemetry in a patient with irritable colon. Lancet 1979;ii:321–3. [DOI] [PubMed] [Google Scholar]
- 12.Kellow JE, Gill RC, Wingate DL. Prolonged ambulant recordings of small bowel motility demonstrate abnormalities in the irritable bowel syndrome. Gastroenterology 1990;98:1208–18. [DOI] [PubMed] [Google Scholar]
- 13.Creed FH, Guthrie EA. Progress report: psychological factors in the irritable bowel syndrome. Gut 1987;28:1307–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drossman DA, Talley NJ, Leserman J, et al. Sexual and physical abuse and gastrointestinal illness: Review and recommendations. Ann Intern Med 1995;123:782–4. [DOI] [PubMed] [Google Scholar]
- 15.Bennett EJ, Tennant CC, Piesse C, et al. Level of chronic life stress predicts clinical outcome in irritable bowel syndrome. Gut 1998;43:256–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gwee KA, Leong YL, Graham C, et al. The role of psychological and biological factors in postinfective gut dysfunction. Gut 1999;44:400–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Drossman DA, McKee DC, Sandler RS, et al. Psychosocial factors in the irritable bowel syndrome. A multivariate study of psychologic distress associated with irritable bowel syndrome. Comparison of community and medical clinic samples. Gastroenterology 1988;95:701–8. [DOI] [PubMed] [Google Scholar]
- 18.Heaton KW, O’Donnell LJD, Braddon FEM, et al. Symptoms of irritable bowel syndrome in a British urban community: consulters and nonconsulters. Gastroenterology 1992;102:1962–7. [DOI] [PubMed] [Google Scholar]
- 19.Zighelboim J, Talley NJ, Phillips S, et al. Visceral perception in irritable bowel syndrome. Dig Dis Sci 1995;40:819–27. [DOI] [PubMed] [Google Scholar]
- 20.Drossman DA, Thompson WG, Talley N, et al. Indentification of sub-groups of functional gastrointestinal disorders. Gastroenerol Int 1990;3:159–72. [Google Scholar]
- 21.Creed FH, Craig T, Farmer RG. Functional abdominal pain, psychiatric illness and life events. Gut 1988;29:235–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guthrie E, Creed FH, Whorwell PJ. Severe sexual dysfunction in patients with the irritable bowel syndrome; a comparison of patients with inflammatory bowel disease and peptic ulcer disease. BMJ 1987;295:576–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Creed F, Fernandez L, Guthrie E, et al. The cost-effectiveness of psychotherapy and paroxetine for severe irritable bowel syndrome. Gastroenterology 2003;124:303–17. [DOI] [PubMed] [Google Scholar]
- 24.Drossman DA, Li Z, Andruzzi E, et al. U. S. householder survey of functional GI disorders: prevalence, sociodemography and health impact Dig Dis Sci 1993;38:1569–80. [DOI] [PubMed] [Google Scholar]
- 25.Drossman DA, Li Z, Toner BB, et al. Functional bowel disorders. A multicenter comparison of health status and development of illness severity index. Dig Dis Sci 1995;40:986–95. [DOI] [PubMed] [Google Scholar]
- 26.SCAN World Health Organisation. Schedules for Clinical Assessment in Neuropsychiatry (SCAN). Geneva: Division of Mental Health, 1994.
- 27.10th Revision of the International Statistical Classification of Diseases and Related Health Problems. Geneva: World Health Organisation, 1992.
- 28.SCL-90-R Derogatis LR. The SCL-90-R Manual-II: Scoring, administration and procedures for the SCL-90-R, 2nd ed. Towson, MD: Clinical Psychometric Research, 1992.
- 29.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry 1960;23:56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leserman J, Li Z, Drossman DA, et al. Impact of sexual and physical abuse dimensions on health status: development of an abuse severity measure. Psychosom Med 1997;59:152–60. [DOI] [PubMed] [Google Scholar]
- 31.Barkham M, Hardy GE, Startup M. The structure, validity and clinical relevance of the inventory of interpersonal problems. Br J Med Psychol 1996;67:171–85. [DOI] [PubMed] [Google Scholar]
- 32.Horowitz L, Rosenberg SE, Saul E, et al. The inventory of interpersonal problems. J Consult Clin Psychol 1988;56:885–92. [DOI] [PubMed] [Google Scholar]
- 33.Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): 1. Conceptual framework and item selection. Med Care 1992;30:473–83. [PubMed] [Google Scholar]
- 34.Ware JE, Kosinski M, Bayliss MS, et al. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the medical outcomes study. Med Care 1995;33:AS64–79. [PubMed] [Google Scholar]
- 35.Whitehead WE, Holtkotter B, Enck P, et al. Tolerance for rectosigmoid distension in irritable bowel syndrome. Gastroenterology 1990;98:1187–92. [DOI] [PubMed] [Google Scholar]
- 36.Everitt BS. Statistical methods for medical investigations, 2nd edn. London: Edward Arnold, 1994.
- 37.Baker AW, Duncan SP. Child sexual abuse: A study of prevalence in Great Britain. Child Abuse Neglect 1985;9:457–67. [DOI] [PubMed] [Google Scholar]
- 38.Whitehead WE, Crowell MD, Davidodd AL, et al. Pain from rectal distension in women with irritable bowel syndrome. Relationship to abuse. Dig Dis Sci 1997;47:796–804. [DOI] [PubMed] [Google Scholar]
- 39.Nalabof BD, Munakata J, Fullerton S, et al. Evidence for two distinct perceptual alterations in irritable bowel syndrome. Gut 1997;41:505–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Whitehead WE, Palsson OS. Is rectal pain sensitivity a biological marker for irritable bowel syndrome: psychological influences on pain perception. Gastroenterology 1998;115:1263–71. [DOI] [PubMed] [Google Scholar]
- 41.Harraf F, Schmulson M, Saba L, et al. Subtypes of constipation predominant irritable bowel syndrome based on rectal perception. Gut 1998;43:388–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Emmanuel AV, Mason HJ, Kamm MA. Relationship between psychological state and level of activity of extrinsic gut innervation in patients with a functional gut disorder. Gut 2001;49:209–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blomhoff S, Spetalen S, Jacobson MB, et al. Phobic anxiety changes the function of brain-gut axis in irritable bowel syndrome. Psychosom Med 2001;63:959–65. [DOI] [PubMed] [Google Scholar]