Abstract
Aim: Our aim was to perform a prospective evaluation of the frequency and diagnostic consequences of extracolonic findings at multidetector array computed tomography colonography (MDCTC) in asymptomatic patients undergoing surveillance for former colorectal polyps or cancer.
Patients and methods: Seventy five consecutive patients undergoing surveillance for former colorectal cancer (CRC) or large bowel adenoma were examined with MDCTC. Two independent observers evaluated the images with regard to extracolonic findings. Patient records and radiological information systems were reviewed to determine the results and consequences of the workup derived from MDCTC.
Results: Sixty five per cent (95% confidence interval (CI) 55–73%) of patients had extracolonic abnormalities and in 12% (CI 7–18%) of patients additional workup was indicated. Two patients (3% (CI 1–6%)) underwent surgery because of the findings (one) or because of complications of the workup (one).
Conclusion: MDCTC identifies a large number of extracolonic findings. Approximately 12% of asymptomatic patients undergo additional workup, of benefit to only a few. The high prevalence of extracolonic findings may make MDCTC a problematic colorectal screening tool for both ethical and economic reasons.
Keywords: colon, colorectal screening, computed tomography, colonography, extracolonic findings
Computed tomography colonography (CTC) is a minimally invasive colon imaging technique for detection of colonic neoplasms. Previous studies have shown mixed results with regard to polyp and cancer detection compared with conventional colonoscopy but the examination has been proposed as an option for colorectal screening by many authors.1–6
In addition to the colorectum, organs, vessels, bone, and soft tissue are also depicted, with the possibility of diagnosing pathology outside the large bowel. However, there is also a risk of carrying out expensive, unnecessary, and even harmful workups. Two prospective studies have addressed the issue of extracolonic pathology at CTC, with large differences in the prevalence of extracolonic findings and the need for additional workup.7,8
In this study, we report the clinical consequences of prospectively recorded extracolonic pathology at multidetector array computed tomography colonography (MDCTC) in asymptomatic patients undergoing surveillance for former colorectal cancer (CRC) or large bowel adenoma.
PATIENTS AND METHODS
The study protocol was approved by the local ethics committee and informed consent was obtained from all participants. In total, 75 asymptomatic patients (35 women, 40 men; median age 61 years (range 33–78)) were examined with both MDCTC and colonoscopy.
We invited 101 consecutive patients undergoing surveillance because of a history of neoplastic polyps or CRC to participate in the study; 85 accepted and 75 subsequently participated. Two patients were excluded because of other severe diseases and two cases were cancelled because of computed tomography (CT) scanner mechanical difficulty. Three patients had severe incompetence of the anal sphincter and were excluded because it was impossible to obtain satisfying colonic distension. Three other patients were excluded from the project because of non-compliance with the bowel cleansing procedure.
Patients had, on average, been examined by colonoscopy 3.6 years (range 1–5) before entering the study and 31 of these patients had undergone colorectal surgery for CRC or large adenomas a median of five years (range 1–12) before study participation.
Technique
CT scanning was performed immediately before colonoscopy with a Marconi Mx8000 scanner (Marconi Medical Systems Inc., Cleveland, Ohio, USA). Glucagon 1 mg was administered intravenously prior to the examination to reduce the occurrence of colonic spasms; oral or intravenous contrast was not administered. The colon was insufflated with room air through a rectal rubber catheter to maximum patient tolerance without pain. A scout view of the abdomen and pelvis was obtained to monitor colonic distension and additional air was insufflated if necessary and accepted. Patients were examined with a slice thickness of 3.2 mm (4×2.5 mm), increment 1.6 mm, 70 mAs, 120 kV, rotation time 0.5 seconds, pitch 1.25, standard resolution, field of view to fit, in the supine and prone positions. The left flexure in particular can be located very close to the diaphragm and it is necessary to obtain images of the most distal 2–5 cm of the lungs to ensure that the entire colon is depicted (fig 1 ▶). On average, image acquisition was obtained in 2 ×17 seconds generating 500–600 axial images. The effective radiation dose, calculated from the PC programme CT Dose version 0.6.7, was 6 mSv.
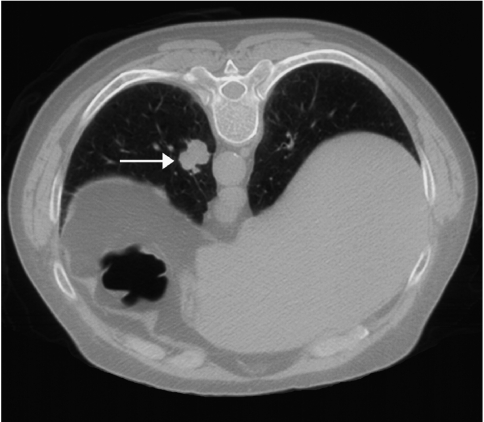
Figure 1.
Axial computed tomographic image of a 74 year old male showing a 20 mm lung tumour in the most distal part of the left lung (white arrow). The colonic lumen corresponding to part of the left flexure is seen (black).
Methods for polyp detection have been described previously.9 Image evaluation with regard to extracolonic findings was performed on a MxView workstation (Marconi Medical Systems Inc.). Two radiologists (a consultant radiologist and a research fellow) independently evaluated the data sets with regard to extracolonic pathology on two dimensional axial and multiplanar reformatted images with preset window/level settings which could be adjusted interactively. Both observers were unaware of patients’ medical histories and all extracolonic findings reported by one or both observers were included.
For each organ (lung, liver, gall bladder, pancreas, spleen, adrenal glands, kidneys, genital organs, vessels, soft tissue, and bone) the type of pathology was noted and observers commented on the necessity for further workup and the type of workup recommended using standards from the daily clinical work at our department. Reasons for workup were findings not previously known from other examinations or from the patient history: aortic aneurysm; likely malignant masses; indeterminate adrenal or pulmonary lesions of any size; indeterminate masses in solid organs (liver, kidney, spleen); and ovarian cysts larger than 4 cm maximum diameter. Before additional workup was initiated, a check was made to determine whether the lesion was known to the patient or had been found at a previous examination or previous hospital. The latter was done by reviewing records from former hospitalisations at our or other institutions and by reviewing the computerised radiological information system at our hospital. The research fellow informed the patient and organised the follow up with the relevant clinical departments. Atherosclerosis of the aorta and lumbar spondylosis were not assessed as they were extremely common in this group of patients.
Six months after MDCTC, all patient records and computerised radiology information at our institution were reviewed to record the consequences of the workup. In patients referred to other hospitals for workup, relevant information concerning the workup was obtained.
Statistics
The χ2 test was used to compare the distribution of sex, with a level of significance of 0.0510; 95% confidence intervals (CI) were calculated using binomial distribution.
RESULTS
MDCTC revealed 68 extracolonic findings among 49 patients (65% (95% CI 55–73%)). In 12% (95% CI 7–18%) of patients, additional workup was recommended and the findings prompted additional workup in eight patients (one patient refused to undergo workup). Two patients (3% (95% CI 1–6%)) underwent surgery as a consequence of the workup or because of complications of the workup (table 1 ▶). Table 2 ▶ shows the distribution of sex and the need for additional workup. Four males and five females had extracolonic pathology indicating further workup; this difference was not statistically significant (p = 0.57).
Table 1.
Extracolonic findings that resulted in further workup
| Finding at CTC | Patients with extracolonic finding (n) | Patients with additional workup (n) | Workup | Results | Patients who underwent surgery |
| Lung tumour | 1 | 1 | Chest x ray 1/1, CT 1/1, FNA 1/1 | Non-small cell pulmonary carcinoma | Lung resection. Recurrent disease, died 1 y after surgery |
| Hepatic mass | 1 | 1 | US 1/1 | Fatty sparing | |
| Renal cyst | 12 | 1 | US 1/12 | Renal cyst | |
| Adrenal mass | 3 | 2* | CT 2/3, blood test 2/3, urine-VMA 2/3 | Incidentaloma (n = 2) | |
| Suspicion of local recurrence of rectal carcinoma | 1 | 1 | MRI 1/1, US w/FNA 1/1 | Endometrioma | Surgical drainage of infection after FNA |
| Ovarian cyst, simple, >4 cm | 1 | 1 | US 1/1 | Cyst | |
| Enlarged uterus | 4 | 1 | US ¼ | Fibromatous uterus |
*One patient did not want additional workup because of other severe disease.
CTC, computed tomography colonography; CT, computed tomography; US, ultrasound; FNA, fine needle aspiration; VMA, vanillylmandelic acid; MRI, magnetic resonance imaging.
Table 2.
Distribution by sex of patients with extracolonic findings
| Male | Female | |
| No extracolonic findings | 14 | 12 |
| Extracolonic findings present, workup not needed | 22 | 18 |
| Extracolonic findings present, workup needed | 4 | 5 |
Data are number of patients.
One patient with a hyperdense renal cyst was examined by ultrasound because the lesions had heterogeneous attenuation at CT. Ultrasound showed renal cyst with haemorrhage. One patient with an enlarged uterus was examined because the exact nature of the enlargement was unclear.
Table 3 ▶ shows the number of patients with abnormalities that did not prompt additional workup and represents patients with an abnormality previously known or patients with lesions of minor clinical importance. Twenty six patients (35% (95% CI 25–43%)) were classified as not having abnormal extracolonic findings by both observers.
Table 3.
Extracolonic findings that did not prompt further workup
| Finding | No of patients |
| Pleural effusion | 1 |
| Pleural plaque | 1 |
| Hepatic cyst | 10 |
| Hepatic steatosis | 3 |
| Hepatic calcifications | 3 |
| Gall stones | 6 |
| Pancreatic calcifications | 3 |
| Renal calcifications | 3 |
| End stage kidney | 1 |
| Renal calculi | 2 |
| Aortic ectasia | 1 |
| Calcified mesenterial lymph nodes | 1 |
| Hernia (hiatus, inguinal) | 5 |
| Ovarian cyst, ⩽4 cm | 2 |
| Sacroiliitis | 1 |
| Osteosclerotic lesions, bone* | 1 |
| Cystic lesions in pelvic bone† | 1 |
*Patient with known prostatic cancer.
†Patient with former trauma of the hip, known degenerative lesions.
DISCUSSION
In a Danish population consisting of asymptomatic patients undergoing polyp/cancer surveillance, we found extracolonic abnormalities by MDCTC in 65% of cases, with the need for further workup in 12% and surgery in 3%. Image interpretation was performed independently by two observers initially unaware of the patient’s history, and additional workup was recommended independently of the indications for study participation. We had expected extracolonic findings to be more prevalent among women (because the female genitals are covered within the scan field) but we found an even distribution of extracolonic findings among men and women.
In an American population consisting of patients undergoing CRC or polyp surveillance and patients with known colorectal lesions, Hara et al found incidental extracolonic findings by two observers in 41% of 264 patients and “highly important” findings in 11%.7 Seven per cent of patients underwent additional workup and 2% underwent surgery; patients were examined with single slice CT.7 In an Australian study with 100 predominantly symptomatic patients and single slice CT, but only one observer, 15% of the population had extracolonic findings not previously known, 11% underwent further workup, and 2% underwent surgery.8 Corrected for bowel associated pathology, additional workup was indicated in 11% of 74 patients in our study because of pathology, without association with their former colorectal disease, and one patient underwent surgery (1.4%). Compared with the studies of Hara and colleagues7 and Edwards and colleagues,8 the discrepancies may be due to differences in the populations studied and in the standards and indications for further workup in different countries. Compared with other Western countries, Denmark has relatively few spiral CT scanners per million inhabitants11 and our population may not has been as well examined before entering the study and therefore more of our findings may not have been previously known. The use of two observers and also the improved spatial resolution with MDCTC compared with single slice CTC may have contributed to the larger number of extracolonic findings—especially incidentalomas of the adrenal glands (fig 2 ▶) which were small in two of our patients (5 and 6 mm). Despite these differences, all three studies found that extracolonic findings at CTC prompted intervention in approximately 2% of patients as a direct consequence of the findings or as a result of complications associated with the workup.
Figure 2.
Axial computed tomographic (CT) image of a 65 year old female showing a 10 mm focal process in the left adrenal gland (white arrow). No hormonal abnormalities were found and the size of the lesion was unchanged at the follow up CT scan performed six months after CT colonography. The patient was eventually diagnosed with “incidentaloma”.
Our results raise the question of whether MDCTC is a colon examination or abdominal screening—this study reveals MDCTC as a sort of “Pandora’s box”, releasing a cascade of diagnostic events with medicolegal, ethical, and economic implications. On the other hand, the examination depicts numerous conditions, knowledge of which may be beneficial to the patient and clinician, even if the patient has no symptoms at the time of diagnosis. Furthermore, MDCTC can detect harmful conditions at an earlier stage and therefore improve survival—this applies to aortic aneurysms and some forms of cancer.12 As was the case with the patient with the lung tumour, it also carries a risk of lead time bias—that is, survival is not improved but the patient lives longer with the diagnosis because the disease was found before it produced any symptoms. Although this gives patients an opportunity to organise their lives, it does not necessarily improve the quality of life.
We studied a high risk population for colon pathology, and not a screening population of, for example, subjects aged ⩾50 years with no risk factors for developing CRC other than age, and hence our findings cannot be applied directly to other populations. However, the frequency of extracolonic pathology prompting further workup reported here may be comparable with the frequency in a screening population. In a former study evaluating cleansing regimens prior to CTC,13 we found extracolonic pathology prompting additional workup in five of 29 healthy volunteers aged >45 years (17%) and surgery in one patient (3.4%). In contrast, we found extracolonic findings with the need for additional workup in 23% of 66 symptomatic patients (95% CI 15–35%) and the need for surgery in one patient, indicating that extracolonic findings in this group of patients were not that “incidental” (Ginnerup Pedersen et al, unpublished).
The sensitivity and specificity of CTC for detections of polyps and cancer in a screening population are unknown and furthermore, we do not know if the population would attend screening with CTC. At present, with no possibility of “filtering” extracolonic data, extracolonic pathology is a major problem if CTC is to be used for colorectal screening, in terms of both ethical and economic issues. Studies from screening mammography have shown that women classified as “false positive” are more liable not to reattend screening mammography.14 The fact that healthy people can be classified as “false positive” because of colonic as well as extraintestinal findings may produce problems with patient compliance if CTC were to be used as a continuous screening examination. Some of these extracolonic findings will be diagnosed (and a workup will be performed) in the first screening round, therefore not inconveniencing the patients or incurring additional costs, but there is a risk of frightening patients away from reattending.
Our study emphasises the need for patients to be informed of the possibility of extracolonic findings that may prompt further workup or the detection of conditions that can be serious. In the present study, the possibility “of checking” extracolonic organs was mentioned as a positive motivation for study participation by many patients. Patients without extracolonic findings or with extracolonic findings of no importance were relieved (although not monitored) but much anxiety was induced in those with extracolonic findings that prompted additional workup. The need for workup in approximately 12% of patients may perhaps be acceptable if extracolonic pathology could be excluded in the 88% without an obvious need for workup. This is not the case because the examination is performed without contrast enhancement and with low tube current and therefore with inferior image quality with regard to soft tissue, and our findings may be the tip of the iceberg. Moreover, some conditions may not even be detectable with contrast enhanced CT. Clinicians should not hesitate to refer patients with normal extracolonic findings at CTC to the appropriate examination if conditions not detected are suspected.
In conclusion, MDCTC identifies a large number of extracolonic findings. Approximately 12% of patients undergo additional workup, of benefit to only a few. The high prevalence of extracolonic findings may make MDCTC a problematic colorectal screening tool for both ethical and economic reasons.
Acknowledgments
Financial support for this study was provided by the Danish Medical Research Council; the Danish Institute for Health Technology Assessment (DIHTA); Forskningsinitiativet, County of Aarhus; the Danish Cancer Foundation, Kliniske Forskningsenhed in Aarhus, AP Møller og Hustru Chastine Mc-Kinney Møllers Fond til Almene Formål, Eva and Henry Frænkels Mindefond; and Institute of Experimental Clinical Research, Aarhus University.
Abbreviations
CRC, colorectal cancer
CT, computed tomography
CTC, computed tomography colonography
MDCTC, multidetector array computed tomography colonography
REFERENCES
- 1.Rex DK, Vining D, Kopecky KK. An initial experience with screening for colon polyps using spiral CT with and without CT colography (virtual colonoscopy). Gastrointest Endosc 1999;50:309–13. [DOI] [PubMed] [Google Scholar]
- 2.Mendelson RM, Foster NM, Edwards JT, et al. Virtual colonoscopy compared with conventional colonoscopy: a developing technology. Med J Aust 2000;173:472–5. [DOI] [PubMed] [Google Scholar]
- 3.Pescatore P, Glucker T, Delarive J, et al. Diagnostic accuracy and interobserver agreement of CT colonography (virtual colonoscopy). Gut 2000;47:126–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fenlon HM, Nunes DP, Schroy PC, et al. A comparison of virtual and conventional colonoscopy for the detection of colorectal polyps. N Engl J Med 1999;341:1496–503. [DOI] [PubMed] [Google Scholar]
- 5.Yee J, Akerkar GA, Hung RK, et al. Colorectal neoplasia: performance characteristics of CT colonography for detection in 300 patients. Radiology 2001;219:685–92. [DOI] [PubMed] [Google Scholar]
- 6.Macari M, Bini EJ, Xue X, et al. Colorectal neoplasms: prospective comparison of thin-section low-dose multi-detector row CT colonography and conventional colonoscopy for detection. Radiology 2002;224:383–92. [DOI] [PubMed] [Google Scholar]
- 7.Hara AK, Johnson CD, MacCarty RL, et al. Incidental extracolonic findings at CT colonography. Radiology 2000;215:353–7. [DOI] [PubMed] [Google Scholar]
- 8.Edwards JT, Wood CJ, Mendelson RM, et al. Extracolonic findings at virtual colonoscopy: implications for screening programs. Am J Gastroenterol 2001;96:3009–12. [DOI] [PubMed] [Google Scholar]
- 9.Ginnerup Pedersen B, Christiansen TE M, Bjerregaard NC, et al. Colonoscopy and multi-detector array computed tomography colonography—detection rates and feasibility. Endoscopy 2003;35:736–42. [DOI] [PubMed] [Google Scholar]
- 10.Altman DG. Practical statistics for medical research. London: Chapman and Hall, 1991.
- 11.Thomsen HS. The radiological structure in Denmark. Eur Radiol 1997;7:441–2. [DOI] [PubMed] [Google Scholar]
- 12.Ashton HA, Buxton MJ, Day NE, et al. The multicentre aneurysm screening study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet 2002;360:1531–9. [DOI] [PubMed] [Google Scholar]
- 13.Ginnerup Pedersen B, Christiansen TE, Mortensen FV, et al. Bowel cleansing methods prior to CT colonography. Acta Radiol 2002;43:306–11. [DOI] [PubMed] [Google Scholar]
- 14.McCann J, Stockton D, Godward S. Impact of false-positive mammography on subsequent screening attendance and risk of cancer. Breast Cancer Res 2002;4:R11. [DOI] [PMC free article] [PubMed] [Google Scholar]