Abstract
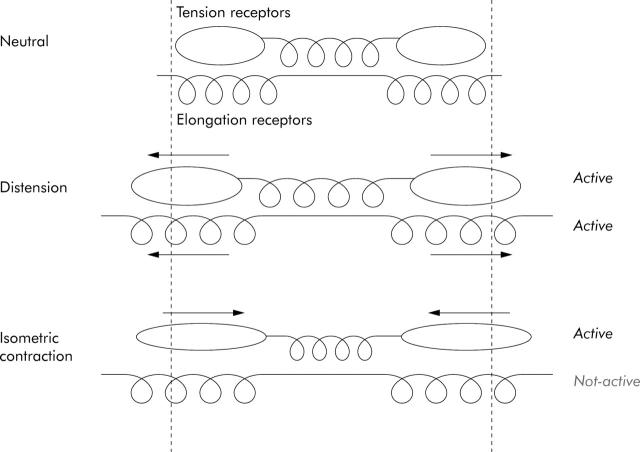
Background: Perception of colonic distension, which is enhanced in a subset of patients with irritable bowel syndrome, requires activation of mechanoreceptors. In animal studies, distension activates both in series (“tension”) and in parallel (“elongation”) mechanoreceptors. During active contractions against a fixed volume balloon, tension receptors are activated without elongation of receptor activation.
Aim: To evaluate the role of tension receptors in the perception of mechanical stimuli from the colon in healthy subjects.
Methods: A 700 ml balloon connected to a barostat-manometer assembly was placed in the descending colon of 10 healthy subjects. After volume controlled distension (50 ml/2 minutes) to assess the first perception threshold, fixed volume subthreshold distension (122 (16) ml) was maintained for a 30 minute period before and after administration of neostigmine 0.5 mg intravenously. Mean intraballoon pressure, number, amplitude, and duration of contractions, and frequency of sensations were analysed. The period after neostigmine was divided into 10 second intervals and evaluated for the occurrence of contractions and onset of sensations. Fisher’s exact test was applied to calculate the sensation-contraction association probability (SAP) as (1.0−p)×100%.
Results: Neostigmine increased intraballoon pressure (p<0.01), number of contractions (p<0.01), and number of sensations (p<0.01) per minute in all subjects. In seven of 10 subjects a significant association (SAP >95%) was found between sensations and contractions. In the remaining subjects, contractions were not associated with sensations and had lower amplitude (p<0.05) and duration (p<0.01) compared with contractions in the other seven subjects.
Conclusion: In humans, tension receptors are involved in mediating colonic mechanosensitivity.
Keywords: barostat, colon, manometry, mechanoreceptors, visceral sensitivity, irritable bowel syndrome
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterised by episodes of symptoms referring to the large bowel, in the absence of organic disease that readily explains them.1 Although several pathophysiological mechanisms may contribute to IBS symptoms, current concepts attribute a major role to visceral hypersensitivity.2–4 Rectal and colonic balloon studies have demonstrated enhanced sensitivity to rectal or colonic distension in a subset of patients with IBS although colonic compliance is normal.2–9
Even though the reasons for this hypersensitivity to distension are unknown, mechanoreceptors must be activated to transduce the distending stimulus to the brain. In the gut wall, mechanosensitive receptors are located in the smooth muscle and serosal layers.10 In animals, serosal mechanoreceptors arranged in parallel (“elongation”) respond to stimuli that elongate the visceral wall.10,11 Muscular mechanoreceptors arranged in series (“tension”) respond to stimuli that increase tension of the visceral wall (fig 1 ▶).10,11 Balloon distension activates both elongation and tension receptors. Recent studies have underlined the role of changes in wall tension in determining perception of gastric12,13 and rectal distension14 but this has not been established for perception of colonic distension.
Figure 1.
Schematic representation of the response of tension and elongation receptors.
Different methods have been used to study the role of tension mechanoreceptors in gastric studies. The simplified law of Laplace has been used to estimate gastric wall tension during barostat studies15 but this requires a number of assumptions that are not fulfilled during colonic distension: the colon has to assume a spherical shape, the colonic wall has to be infinitely thin, and no active contractions occur.16 Others used agents that relax the viscera but a combination of distension and relaxation may have opposite effects on tension receptors.17,18
In animal studies, active contraction against a fixed volume balloon located in the lumen of viscera has been demonstrated to activate tension receptors without elongation receptor activation,11 and this approach has been used to study the role of changes in wall tension in the perception of gastric distension in healthy subjects.13 Isometric contractions (against an intraluminal fixed volume balloon) of viscera in close apposition to the balloon generate increases in intraballoon pressure which reflect changes in wall tension, and the need for calculation of absolute values of wall tension is overcome. Active contractions during controlled circumferential stretch have also been used to activate tension receptors in the guinea pig colon and rectal wall.19 In the present study, we used neostigmine to induce colonic phasic contractions in the presence of a fixed volume balloon inflated in the descending colon in healthy subjects and we evaluated the temporal relationship between the occurrence of contractions and changes in sensation.
MATERIALS AND METHODS
Subjects
Ten healthy subjects (seven males; mean age 24 (1) years) participated in the study. Subjects had no gastrointestinal symptoms, normal bowel habit, normal physical examination, and no previous gastrointestinal surgery (except for appendicectomy). None of the subjects was taking a drug known to influence bowel motility. All women had a negative plasma β-human chorionic gonadotropin pregnancy test within 48 hours of the procedures. Each subject gave written informed consent to participate in the study which was approved by the ethic committee.
Study design
After a 12 hour fasting period, all subjects were admitted to the motility clinic for bowel preparation, comprising two to four 2 l tap water enemas. Left sided colonoscopy was then performed under conscious sedation with intravenous midazolam (5 mg) and a multilumen barostat-manometry assembly incorporating six manometer point transducers and a balloon linked to an electronic barostat (Synectics Visceral Stimulator, Sweden) was introduced into the left colon. After 90 minutes of recovery, participants were placed in the right lateral position on a bed, the barostat balloon was unfolded by inflation with 150 ml of air, and thereafter was completely deflated. The position of the balloon inside the colonic lumen was checked fluoroscopically at the beginning and end of each study.
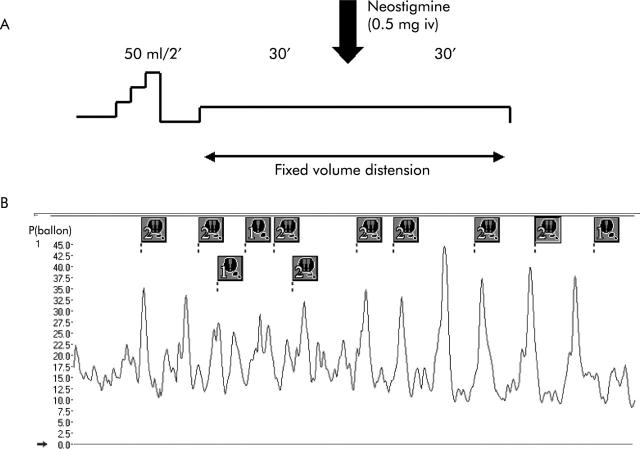
Figure 2A ▶ shows the experimental procedure performed in each subject. Volume controlled stepwise distension (50 ml/2 minutes) was performed until the occurrence of first perception. After 15 minutes of recovery, intraballoon volume was set at a level 50 ml below the first perception of distension and the recording was continued for 30 minutes before and after intravenous injection of 0.5 mg of neostigmine (Prostigmin; ICN, Zoetermeer, the Netherlands). During the recording period, subjects were instructed to avoid movement and to stay awake. Heart rate and blood pressure were monitored before and at 15 and 30 minutes after neostigmine injection. Intraballoon pressure and manometry were monitored throughout the study.
Figure 2.
(A) Scheme of the experimental procedure performed in each subject. (B) Example of part of a tracing recorded by the barostat in one subject after administration of neostigmine. The vertical axis shows intraballoon pressure recorded by the barostat. Each marker indicates the onset of sensation. The number identifies the intensity of sensation chosen by the subject. Note the temporal relation between contractions and sensations.
Barostat-manometer assembly
The highly compliant polyethylene balloon (10 cm long, 700 ml capacity) was tied 27 cm from the end of a multilumen polyvinyl tube (Zinectics SVS Barostat Catheter; Medtronic, Functional Diagnostics A/S, Skoveland, Denmark). It was linked to the barostat pressure sensor by a smaller lumen tube (0.8 mmØ) and to the air injection-aspiration system by another larger lumen tube (2.5 mmØ). Two pairs of three pressure recording side ports, each at 5 cm intervals, were situated 5 cm oral and 5 cm caudal to the barostat balloon, respectively. These were connected to pressure recording ports and perfused with water at 0.4 ml/min (Arndorfer Medical Specialties Inc., Greendale, Wisconsin, USA). In general, the three oral pressure recording side ports were in the upper descending colon and the three aboral ones were located in the sigmoid colon. A personal computer using Polygram for Windows recorded barostat and manometry data.
Registration of sensations
Sensations were recorded using a subject operated marker device connected to the computer. All subjects were instructed to report the intensity of sensations on a four number keypad (1–4, 1 = first sensation, 4 = discomfort) whenever they noticed any change in perception.
Data analysis
Analysis of intraballoon pressure recordings
The intraballoon pressure baseline was calculated using dedicated software developed in our own laboratory.18 Movement artefacts were visually identified and removed from analysis. Five minute baseline pressure (excluding phasic contractions) was averaged over a 30 minute period before and after administration of neostigmine. Mean baseline pressure during the 30 minute period before and after injection represented, respectively, basal and post-drug tone of the colonic segment occupied by the barostat balloon.
A colonic phasic pressure wave was defined as a monophasic increase in intraballoon pressure of 5 mm Hg above baseline lasting at least four seconds and interrupting respiratory pressure fluctuations. Isolated pressure increases lasting less than four seconds with amplitudes of more than 5 mm Hg were considered artefacts. For each pressure wave, amplitude and duration were calculated. Amplitude of the colonic phasic pressure waves (mm Hg) was measured from the baseline pressure to the peak of the wave, and duration (seconds) from the onset of the upstroke to the end of the wave.
Analysis of manometry recordings
A contraction was defined as a pressure increment >10 mm Hg above baseline lasting for more than five seconds. A contraction was defined as propagated when it was recorded caudally in more than two manometric channels. Contractions reaching high amplitudes and propagating caudally for ⩾15 cm were considered high amplitude propagated contractions (HAPCs), according to published criteria.20 Amplitude, duration, and velocity of propagation of contractions were assessed automatically using dedicated software developed in our own laboratory21 and confirmed visually. Propagation velocity(cm/s) was calculated as the relation of distance between recording transducers with time of onset of contraction in those recording transducers.
Association between sensations and contractions
The relation between sensations recorded by the subject operated device and contractions recorded by the barostat was evaluated using a modification of the symptom association probability described by Weusten and colleagues.22 In the absence of a generally accepted time interval to consider a colonic contraction associated with a sensation, a 10 second interval, corresponding to the median duration of phasic contractions, was chosen as the time window. The period after administration of neostigmine was subdivided in 10 second intervals and evaluated for the occurrence of increases in sensation. An increase in sensation was considered contraction related if the upstroke of the contraction occurred within 10 seconds before the recorded increase in sensation. Tracings were then evaluated for the occurrence of phasic contractions without an increase in sensation within the time intervals following the peak of the contractions. Finally, the remaining time was subdivided into corresponding intervals and identified as intervals with no sensations and no contractions. Following this procedure, a 2×2 contingency table for occurrence of contractions and sensations was obtained for each subject (fig 3 ▶). Fisher’s exact test was applied to the contingency table of each subject to calculate the probability of increases in sensation associated with phasic contractions. A probability value of <0.05 (two tailed) indicated that the two variables were statistically related. The sensation-contraction association probability (SAP) was expressed as (1.0−p)×100%. Figure 2B ▶ shows an example of part of a tracing recorded by the barostat in one subject after administration of neostigmine. The same analysis of the association was also performed to evaluate the relation between sensations and contractions recorded by the manometry.
Figure 3.
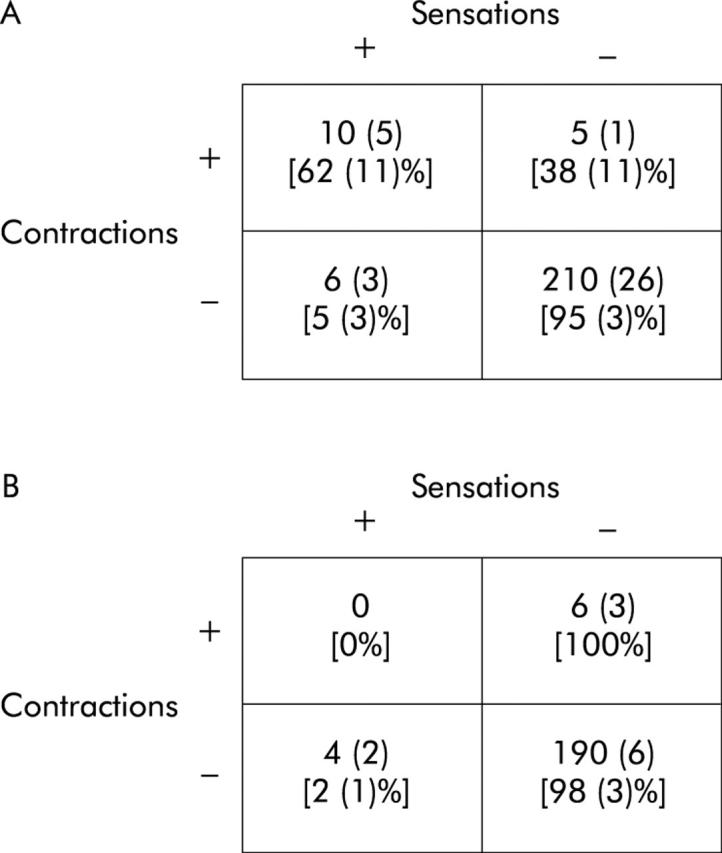
(A) Contingency table reporting the mean (SEM) number of intervals with the four combinations of events in subjects with a significant association between contractions and sensation (n = 7). Numbers in parentheses are line percentages. (B) Contingency table reporting the mean (SEM) number of intervals with the four combinations of events in subjects without a significant association between contractions and sensation (n = 3). Numbers in parentheses are line percentages.
Statistical analysis
Wilcoxon and Mann-Whitney U tests were used to compare intra- and intersubject variations, respectively, in intraballoon pressure, number, amplitude, and duration of contractions, and frequency of sensations before and after neostigmine injection. Fisher’s exact test was applied to calculate the probability of association between variables. Correlation between variables was evaluated using Pearson’s test. Bonferroni’s correction was applied to multiple comparisons. Differences were considered to be significant at the 5% level. All data are given as mean (SEM).
RESULTS
The mean volume evoking the first perception was 166 (38) ml. The subthreshold volume applied to maintain a constant level of distension inside the balloon was 122 (16) ml. Neostigmine was administered intravenously to every healthy subject. None developed cholinergic side effects. Blood pressure and heart rate were not significantly altered by administration of neostigmine.
Effect of neostigmine on intraballoon pressure and number of contractions recorded by the barostat
During the 30 minute period of volume controlled distension before neostigmine, mean intraballoon pressure was 7.6 (1) mm Hg and the number of contractions was 1.1 (0.6). Neostigmine significantly increased intraballoon pressure (10 (1) mm Hg; p = 0.002) and number of contractions (11 (3), p = 0.003; 0.23 (0.02) contractions per minute). The increase in intraballoon pressure occurred within the first five minutes after neostigmine injection in every subject. The first contraction occurred 9 (2) minutes after the onset of infusion and the mean number of contractions per minute was 2 (1) during the first 10 minutes after neostigmine administration.
Effect of neostigmine on number of contractions recorded by manometry
During the 30 minute period before drug administration, the average number of contractions per channel was 13 (6). Neostigmine significantly increased the number of contractions (108 (26), p = 0.005; 3 (0.8) contractions per minute). The first contraction occurred 6 (2) minutes after the onset of infusion.
Effect of neostigmine on number of sensations
The number of sensations during the 30 minute period before and after neostigmine administration were 1.2 (0.6) and 11 (5), respectively (p = 0.007). The first sensation occurred 7 (2) minutes after neostigmine and the mean number of sensations per minute was 0.25 (0.02).
Association between sensations and contractions recorded by the barostat
Application of Fisher’s exact test to the contingency table demonstrated a significant association between contractions and sensations in 7/10 subjects. Four subjects had an SAP >99% and three 96–99%. The mean interval between contraction and sensation in the 10 second intervals with contractions associated with sensations was 4 (0.6) seconds.
Figure 3 ▶ reports the mean contingency tables in subjects with (fig 3A ▶) and without (fig 3B ▶) a significant association between sensations (S) and contractions (C). In subjects with a significant association, 62 (11)% of contractions were associated with sensations, and the presence of contractions explained 65 (12)% of the total number of sensations. Intensities of 1, 2, 3, and 4 identified 5 (5)%, 20 (4)%, 44 (13)%, and 31 (15)% of contraction related sensations, respectively, and 3 (2)%, 57 (15)%, 32 (11)%, and 8 (8)% of contraction unrelated sensations, respectively. In subjects without a significant association, the mean absolute number of intervals with S+C- and with C+S- was similar to that in subjects with an association between contractions and sensations. In contrast, no contractions were associated with sensations. Intensity of 0, 1, 2, and 3 identified 0%, 22 (11)%, 27 (5)%, and 49 (16)% of contraction unrelated sensations, respectively. No correlation was found between the threshold for first perception and percentage of perceived contractions (r = 0.08, NS).
Characteristics of contractions associated (perceived) and not associated (unperceived) with sensations
In subjects with a significant association between contractions and sensations, mean amplitude of perceived contractions was significantly higher than that of unperceived contractions (23 (1) v 20 (1) mm Hg; p = 0.007) whereas duration did not differ (13 (1) v 14 (1) seconds). In subjects without an association between contractions and sensations, amplitude and durations of unperceived contractions were significantly smaller than those of perceived contractions in subjects with an association (18 (0.8) v 23 (1) mm Hg (p = 0.01) and 8 (0.4) v 13 (1) seconds (p = 0.001)).
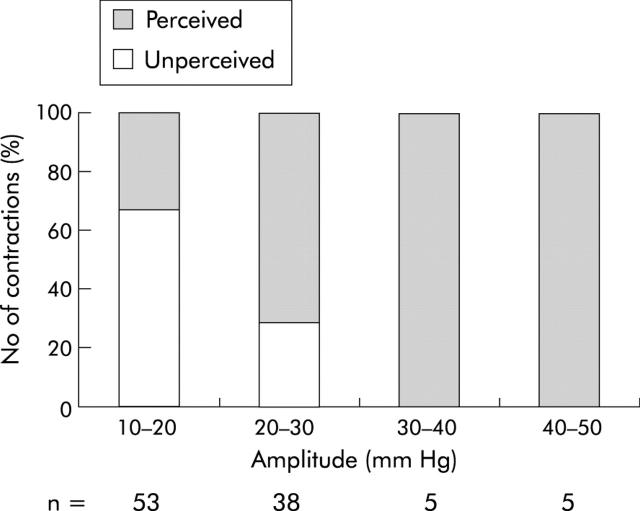
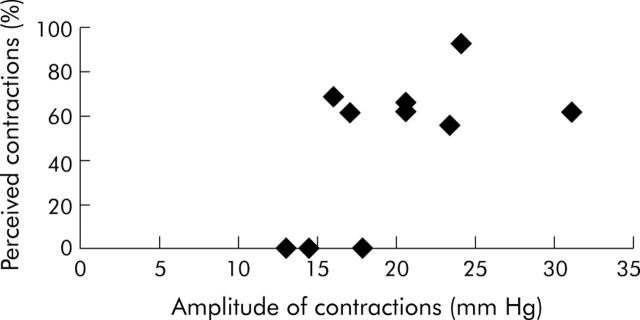
Figure 4 ▶ shows the percentage of perceived contractions for different categories of amplitude. Amplitude above 20 mm Hg yielded 67% of perceived contractions and 23% of unperceived contractions (p<0.0001). Figure 5 ▶ presents the relation between mean amplitude of contractions and the percentage of perceived contractions in every subject. Considering perceived contractions, there was no correlation between amplitude or duration and type of sensations associated (r = 0.007, p = 0.54 for amplitude and r = 0.004, p = 0.63 for duration). The amplitude of perceived and unperceived contractions was similar during the first, second, and third 10 minute periods after administration of neostigmine (19 (1), 23 (1), and 23 (2) mm Hg for perceived contractions, respectively (NS); 19 (2), 20 (2), and 19 (2) mm Hg for unperceived contractions, respectively (NS)). In the same way, duration of perceived and unperceived contractions did not differ during the first, second, and third 10 minute periods after neostigmine (12 (3), 11 (2), and 12 (1) seconds for perceived contractions, respectively (NS); 13 (3), 12 (2), and 9 (1) seconds for unperceived contractions, respectively (NS)).
Figure 4.
Percentage of perceived and unperceived contractions according to different ranges in amplitude.
Figure 5.
Relation between amplitude of total contractions and percentage of perceived contractions in each subject.
Considering all contractions, no correlation was found between volume of distension and amplitude of contractions (r = 0.31, p = 0.41).
Characteristics of propagation of contractions recorded by the barostat
In three subjects with a significant association between contractions and sensations, administration of neostigmine induced the occurrence of 1, 2, and 2 HAPCs, respectively. Mean amplitude and duration of these contractions were 152 (31) mm Hg and 18 (2) seconds. Mean time of propagation of these HAPCs was 0.70 (0.08) cm/se. In the first and second subjects, these HAPCs followed the occurrence of a perceived contraction recorded by barostat. In the third subject, one HAPC followed a perceived contraction and one followed an unperceived contraction (fig 6 ▶). In the remaining subjects, the occurrence of perceived and unperceived contractions was followed or preceded by the presence of non-propagated low amplitude contractions. The mean amplitude and duration of these contractions were 34 (4) mm Hg and 9 (0.8) seconds.
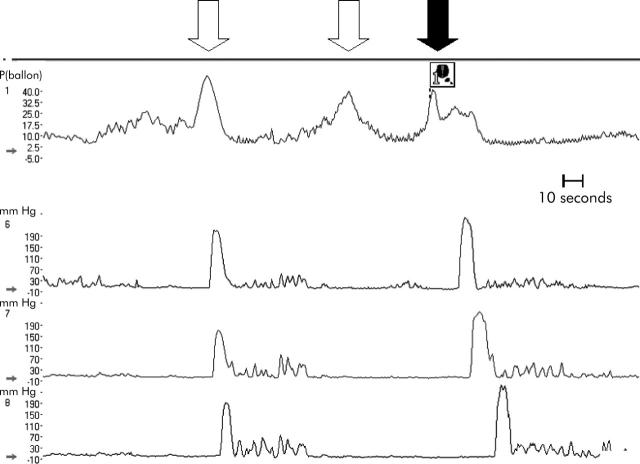
Figure 6.
Example of part of a tracing in one subject after administration of neostigmine. The vertical axis indicates the pressure inside the balloon (channel 1) and the pressure recorded by the manometer at the level of the three side ports below the balloon (channels 6–8). The black arrow indicates a perceived contraction while the white arrows show two unperceived contractions. The marker shows the onset of a sensation. Note that the first unperceived contraction (channel 1) was followed by a high amplitude propagated contraction (HAPC) in the three distal channels (channels 6–8); the second unperceived contraction (channel 1) was not propagated; and the third contraction (channel 1) was perceived (followed in 10 second interval periods by a sensation) and was followed by a HAPC (channels 6–8).
Association between sensations and contractions recorded by manometry
Application of Fisher’s exact test to the contingency table in each subject responding to neostigmine injection did not demonstrate a significant association between sensations and contractions recorded by the manometer in any of the 10 subjects. Mean SAP was 26 (12)%. Amplitude and duration of these contractions were 38 (5) mm Hg and 10 (0.8) seconds, respectively.
DISCUSSION
Previous studies have highlighted the role of changes in wall tension in the perception of gastric12,13 and rectal distensions.14 The present study has evaluated the role of tension receptors in determining the perception of colonic distension. In animal studies, the occurrence of active contractions against a fixed volume balloon activates tension receptors and increases the firing of the afferent pathways.11,19 In the present study, a balloon located in the descending colon was inflated to a fixed volume and neostigmine was administered intravenously. A previous study had demonstrated that neostigmine increases colonic phasic and tonic motor activity and perception but it was unclear whether these sensations were consequent to, or independent of, the increase in colonic contractility.23 In the present study, we confirmed that neostigmine increased colonic tone and induced phasic contractions. The presence of isometric contractions, phasic and tonic, against a fixed volume balloon was associated with the occurrence of sensations, suggesting involvement of changes in colon wall tension in colonic perception.
Establishing a cause and effect relationship between two biological events occurring over time is a difficult task.24 It has been shown that the methodology of probabilistic inference is most appropriate to demonstrate the relationship between two events occurring in a temporal sequence.22,24,25 In particular, the contingency table has been applied to determine the relationship between gastro-oesophageal reflux and symptoms15 and between rectal contractions and sensations.14 Using a similar analysis, we divided the period after administration of neostigmine into intervals of 10 seconds in which we evaluated the presence of a phasic contraction and of an increase in sensation. For each subject, the frequency of occurrence of all four possible combinations was registered in a contingency table and analysed statistically using Fisher’s exact test. Even though a statistically significant result does not prove a causal relationship between contraction and sensation, it provides objective information on the probability that the observed association in time between two events occurs by chance. In our study the probability that the observed association occurred by chance was <5% in three subjects and <1% in four subjects. Moreover, in none of the subjects was a statistically significant relationship found between sensations and contractions recorded by manometry above or below the fixed volume balloon. This result is strongly supportive of the hypothesis that changes in wall tension, induced by phasic contractions against a fixed volume balloon, mediate mechanosensitivity of the colon in humans.
In the contingency table analysis, the choice of the time window is critical to the demonstration of an association between two events. A longer time window increases the probability of finding a association between two events whereas a shorter time window provides a more conservative analysis. In our study the choice of the time window was based on the necessity to mediate between the subject time of reaction after the perception of a contraction and a conservative approach to the statistical analysis. The presence of a time interval between the contraction and its perception by the subjects shorter than the time interval chosen to analyse the association between the two events adds additional support to our choice of a time window.
The association between contractions and sensations was not found in all subjects. In a minority of subjects, contractions induced by neostigmine were not associated with increases in sensation. In subjects with a significant association between contractions and sensations, the amplitude of perceived contractions was greater than that of unperceived contractions. In subjects without an association between contractions and sensations, all contractions were unperceived and they had a significantly lower amplitude and shorter duration. Thus it is possible that a certain critical degree of activation of tension receptors is required for activation of the brain-gut axis. Recently, it has been demonstrated that subliminal gut stimulation activates the same cortical areas as supraliminal stimuli, but the intensity and volume of this activation recorded by functional magnetic resonance imaging is lower during subliminal stimuli.26 These results suggest that the perception of non-painful sensations from the colon may depend on the intensity of the peripheral stimulation.
The reason for the presence of contractions with different amplitude and duration characteristics in the two groups of subjects could reside in the variability of response to a low dose of neostigmine. Alternatively, it could relate to the method of recording. The lack of continuous imaging control during the experiment does not allow exclusion of the presence of a different relation between dimensions of the balloon inflated in the colon in subjects with and without an association between contractions and sensations. Under these conditions colonic contractions may find minor resistance inducing less or absent activation of tension mechanoreceptors. However, lack of a correlation between amplitude of contractions and volume of distension argues against this hypothesis.
Activation of tension receptors induced by phasic contractions was not the only explanation for the occurrence of sensations during colonic distension. Indeed, in a minority of subjects sensations occurred that were not associated with contractions. Moreover, in subjects with a significant association between contractions and sensations, approximately 35% of sensations were not associated with contractions. Sensations not associated with phasic contractions could originate from activation of mechanoreceptors in other segments of the gastrointestinal tract or from activation of other types of receptors in balloon distended segments, such as mechanoreceptors stimulated by the balloon stroking the mucosa.10 Finally, these sensations could be the result of the psychological tendency of subjects to report sensations in the absence of stimuli or perceptual response bias.27
The characteristic of propagation of contractions did not seem to influence perception during colonic distension. However, it has to be considered that neostigmine induced mainly non-propagated contractions and propagated contractions represented only a small percentage of total perceived contractions.
The findings of this study expand our knowledge of the mechanisms of perception of colonic distension and may be relevant in better understanding the pathophysiology and treatment of at least a subset of IBS patients. Animal studies have demonstrated that activation of tension receptors in series with longitudinal muscle transmits information at the level of colonic contractile activity to the central nervous system.28 Previous studies in humans have demonstrated that the increase in colonic motility during volume controlled distensions is followed by the occurrence of painful and non-painful sensations, but no association between motor and sensory events was established.23 The present study demonstrates a relation between sensations and colonic contractions and underlines the role of tension receptors in the perception of non-painful sensations from the colon. Several studies have confirmed that, as a group, IBS patients are hypersensitive to balloon distension of the colon or of the rectosigmoid,4–9 and this is considered an important mechanism in the generation of symptoms in these patients.3 If perception or symptoms in patients with hypersensitivity to colonic distension are related to activation of tension sensitive mechanoreceptors, as recently suggested in the rectum,14 then inactivation of tension receptors by inducing colonic relaxation or inhibiting strong contractions might provide an approach to relieve symptoms.
In conclusion, the present study demonstrates that tension receptors play a role in the perception of mechanosensitive stimuli in the colon. Under our experimental conditions, neostigmine increased colonic tone and induced the occurrence of phasic contractions against a fixed volume balloon. Isometric contraction against a fixed volume balloon enhanced colonic wall tension and was associated with the occurrence of sensations.
Abbreviations
SAP, sensation-contraction association probability
IBS, irritable bowel syndrome
HAPCs, high amplitude propagated contractions
MDP, minimal distending pressure
REFERENCES
- 1.Thompson WG, Longstreth GF, Drossman DA, et al. Functional bowel disorders and functional abdominal pain. Gut 1999;45 (suppl II) :43–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones J , Boorman J, Cann P, et al. British Society of Gastroenterology guidelines for the management of the irritable bowel syndrome. Gut 2000;47 (suppl II) :ii1–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Camilleri M , Coulie B, Tack J. Visceral hypersensitivity: facts, speculations, and challenges. Gut 2001;48:125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouin M , Plourde V, Boivin M, et al. Rectal distension testing in patients with irritable bowel syndrome: sensitivity, specificity, and predictive values of pain sensory thresholds. Gastroenterology 2002;122:1771–7. [DOI] [PubMed] [Google Scholar]
- 5.Bradette M , Delvaux M, Staumont G, et al. Evaluation of colonic sensory thresholds in IBS patients using a barostat. Definition of optimal conditions and comparison with healthy subjects. Dig Dis Sci 1994;39:449–57. [DOI] [PubMed] [Google Scholar]
- 6.Whitehead WE, Engel BT, Schuster MM. Irritable bowel syndrome. Physiological and psychological differences between diarrhea-predominant and constipation-predominant patients. Dig Dis Sci 1980;25:404–13. [DOI] [PubMed] [Google Scholar]
- 7.Whitehead WE, Holtkotter B, Enck P, et al. Tolerance for rectosigmoid distension in irritable bowel syndrome. Gastroenterology 1990;98:1187–92. [DOI] [PubMed] [Google Scholar]
- 8.Lembo T , Munakata J, Mertz H, et al. Evidence for the hypersensitivity of lumbar splanchnic afferents in irritable bowel syndrome. Gastroenterology 1994;107:1686–96. [DOI] [PubMed] [Google Scholar]
- 9.Mertz H , Naliboff B, Munakata J, et al. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology 1995;109:40–52. [DOI] [PubMed] [Google Scholar]
- 10.Grundy D , Scratchard T. Sensory afferents from the gastrointestinal tract. In: Schultz S, ed. Handbook of physiology. The gastrointestinal system. Bethesda Maryland: American Physiological Society, 1989:593–620.
- 11.Iggo A . Tension receptors in the stomach and urinary bladder. J Physiol 1955;128:593–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Distrutti E , Azpiroz F, Soldevilla A, et al. Gastric wall tension determines perception of gastric distension. Gastroenterology 1999;116:1035–42. [DOI] [PubMed] [Google Scholar]
- 13.Piessevaux H , Tack J, Wilmer A, et al. Perception of changes in wall tension of the proximal stomach in humans. Gut 2001;49:203–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corsetti M , Cesana MB, Bhoori S, et al. Altered rectal motor response to distension in patients with irritable bowel syndrome: role of rate of distension. Clin Gastroenterol Hepatol 2004;2:49–56. [DOI] [PubMed] [Google Scholar]
- 15.Distrutti E , Azpiroz F, Soldevilla A, et al. Gastric wall tension determines perception of gastric distention. Gastroenterology 1999;116:1035–42. [DOI] [PubMed] [Google Scholar]
- 16.Gregersen H , Kassab GS. Biomechanics of the gastrointestinal tract. Neurogastroenterol Motil 1996;8:277–97. [DOI] [PubMed] [Google Scholar]
- 17.Thumshirn M , Camilleri M, Choi MG, et al. Modulation of gastric sensory and motor functions by nitrergic and alpha-2 adrenergic agents in humans. Gastroenterology 1999;116:573–85. [DOI] [PubMed] [Google Scholar]
- 18.Tack J , Coulie B, Wilmer A, et al. Influence of sumatriptan on gastric fundus tone and on perception of gastric distension in man. Gut 2000;46:468–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lynn PA, Olsson C, Zagorodnyuk V, et al. Rectal intraganglionic laminar endings are transduction sites of extrinsic mechanoreceptors in the guinea pig rectum. Gastroenterology 2003;125:786–94. [DOI] [PubMed] [Google Scholar]
- 20.De Schryver AM, Samsom M, Smout AJ. In search of objective manometric criteria for colonic high-amplitude propagated pressure waves. Neurogastroenterol Motil 2002;14:375–81. [DOI] [PubMed] [Google Scholar]
- 21.Andrioli A , Wilmer A, Coremans G, et al. Computer-supported analysis of continuous ambulatory manometric recordings in the human small bowel. Med Biol Eng Comput 1996;34:336–43. [DOI] [PubMed] [Google Scholar]
- 22.Weusten BLAM, Roelofs JMM, Akkermans LMA, et al. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology 1994;107:1741–5. [DOI] [PubMed] [Google Scholar]
- 23.Law NM, Bharucha AE, Undale AS, et al. Cholinergic stimulation enhances colonic motor activity, transit, and sensation in humans. Am J Physiol 2001;281:G1228–37. [DOI] [PubMed] [Google Scholar]
- 24.Orr WC. Noncardiac chest pain: conundrum of cause and effect. Am J Gastroenterol 1991;86:1548–50. [PubMed] [Google Scholar]
- 25.Orr WC. The physiology and philosophy of cause and effect. Gastroenterology 1994;107:1898–901. [DOI] [PubMed] [Google Scholar]
- 26.Kern MK, Shaker R. Cerebral cortical registration of subliminal visceral stimulation. Gastroenterology 2002;122:290–8. [DOI] [PubMed] [Google Scholar]
- 27.Whitehead WE, Palsson OS. Is rectal pain sensitivity a biological marker for irritable bowel syndrome: psychological influences on pain perception. Gastroenterology 1998;115:1263–71. [DOI] [PubMed] [Google Scholar]
- 28.Miller SM, Szurszewski JH. Circumferential, not longitudinal, colonic stretch increases synaptic input to mouse prevertebral ganglion neurons. Am J Physiol Gastrointest Liver Physiol 2003;285:G1129–88. [DOI] [PubMed] [Google Scholar]