When the wireless capsule endoscope (WCE) was introduced,1 fears that the capsule might become impacted caused early clinical protocols to exclude any patients with a hint of previous subacute obstruction or symptoms suggestive of Crohn’s disease.2–6 In fact a few patients with Crohn’s disease were inadvertently included in these early studies3–6 as the symptoms of this disease are often subtle and other investigations are sometimes inconclusive. WCE in a short time has acquired a well established role in the investigation of patients with recurrent gastrointestinal bleeding of obscure origin when gastroscopy and colonoscopy fail to reveal the source.2–6 Occult Crohn’s disease was found to be a cause of bleeding or anaemia in several of these series. Capsule endoscopy has been used in more than 100 000 patients worldwide.
Several comparative studies have shown that WCE could outperform push enteroscopy in finding clinical causes of bleeding. Although the image quality of push enteroscopy is superior in the area it reached, WCE did not miss much that push enteroscopy saw and provided images from the large percentage of the small intestine that could not be reached by push enteroscopy. In five comparisons the capsule found more small intestinal pathology than push enteroscopy (66%, 68%, 69%, 55%, 66% v 19%, 32%, 36%, 38%, 28%)3–5,7,8 and four of these studies showed statistically significant differences in favour of capsule endoscopy.4,5,7,8
WCE has also performed well in comparisons with small bowel radiology. Just as the numbers of barium meal and barium enemas have atrophied with the widespread availability of gastroscopy and colonoscopy, radiological investigations of small intestinal disease may also wither with the advent of painless less invasive enteroscopy offered by the wireless capsule endoscope.
The first published study on this topic by Costamagna et al in Gastroenterology9 comparing capsule endoscopy with radiology in the form of a small bowel meal caused controversy because some felt that WCE was being compared with an inferior radiological investigation. In this study, barium follow through was normal in 17 patients and showed ileal nodularity in three patients. Capsule endoscopy was normal in three patients and showed positive findings in the remaining 17 patients. The barium study was considered diagnostic in four (20%) patients. Capsule endoscopy was considered diagnostic in nine (45%) patients, suspicious in eight (40%) patients, and failed in three (15%) patients. For obscure gastrointestinal bleeding, the diagnostic potential of barium follow through was much worse compared with capsule endoscopy (5% v 31%; p <0.05). Capsule endoscopy was well tolerated and better accepted by patients compared with the most recently performed endoscopic procedure.
Subsequent studies have shown that wireless capsule was also superior to state of the art enteroclysis (small bowel enema) and computed tomography (CT) enteroclysis, which currently constitute the best available radiological investigations for imaging the small bowel.
Liangpunsakul and colleagues10 compared state of the art enteroclysis with WCE for its capacity to demonstrate ulcers in the small intestine. There were 40 patients during this study period with negative upper and lower endoscopies and small bowel series. Three patients had multiple small bowel ulcers detected by WCE. The radiologists were told in advance of the WCE findings. Despite this, the enteroclysis studies were negative. All three patients improved after therapy for Crohn’s disease. In this study, WCE was more sensitive for small bowel ulcers than the best enteroclysis available.
Voderholzer and colleagues11 compared the diagnostic yield of WCE with CT enteroclysis. Twenty two patients with suspected small bowel pathology underwent both CT enteroclysis and wireless capsule enteroscopy examinations, conducted by two independent blinded investigators. The results of the two investigations (diagnoses and number, extent, and location of lesions detected) were compared by a third investigator. Patients included in the study had obscure gastrointestinal bleeding (n = 8), Crohn’s disease (n = 8), unexplained diarrhoea (n = 5), or suspected carcinoid tumour (n = 1). Pathological lesions were detected using capsule enteroscopy in 13 patients (59 %) and using CT enteroclysis in eight (36%; p = 0.12). In seven patients (one case each of colonic Crohn’s disease, diverticulitis, Meckel’s diverticulum, carcinoid tumour, mesothelioma, colonic polyps, and irritable bowel syndrome), no pathological changes were found in the small intestine using either method. The diagnosis was established by wireless capsule enteroscopy in four patients with obscure bleeding whereas CT enteroclysis was positive in only one patient (p = 0.1). Crohn’s disease was found in two patients with unexplained diarrhoea. Small bowel lesions were identified in six patients with known Crohn’s disease using capsule enteroscopy or CT enteroclysis. Wireless capsule enteroscopy detected more small bowel lesions than CT enteroclysis in patients with obscure gastrointestinal bleeding and Crohn’s disease.
Enteroclysis with or without CT or magnetic resonance may produce superior images compared with barium follow through but is hated by many patients who find the trans-nasal intubation of the duodenum uncomfortable. Technical improvements in MR have allowed this technology to provide good quality small bowel images using MR enteroclysis, and contrast swallowed by mouth may provide nearly as good images as those acquired when contrast is administered by nasoduodenal tube.12
The surprise to many endoscopists using capsule endoscopy was how some apparently very severe mucosal abnormalities could be missed on good quality radiological studies.
There are now several fully published peer reviewed studies suggesting that Crohn’s disease can be diagnosed with capsule endoscopy in patients who have had a negative colonoscopy, gastroscopy, and small bowel barium studies.13–17 It may be true that a higher rate of ileoscopy might have increased the rate of diagnosis of Crohn’s disease in some of these series. Rates of ileoscopy in large published series of colonoscopy are surprisingly low (for example, 11% in 9000 patients18) and it can be difficult to get through the ileocaecal valve, especially if Crohn’s disease has altered the anatomy of the valve. WCE on the other hand does not always reach the ileocaecal valve because of delayed transit.
It is clear from these and other studies that patients with normal ileoscopy at colonoscopy have been found to have small bowel abnormalities which are thought to be Crohn’s disease at capsule endoscopy and appeared to respond to treatment for this condition. Mow and colleagues,16 Hume and colleagues,19 and Lo20 suggested that capsule enteroscopy may be especially helpful in distinguishing Crohn’s disease from ulcerative colitis in patients with indeterminate colitis, perhaps especially in those in whom ileal pouch formation is being considered. WCE has also been used in children with gastrointestinal blood loss, anaemia, or abdominal pain, and cases of Crohn’s disease are a moderately common finding in this group.21,22 In India, WCE was able to provide images of small intestinal tuberculosis which can be difficult to distinguish from Crohn’s disease.23
In Voderholzer’s paper published in this issue of Gut,24 the frequency of small intestinal Crohn’s disease found by WCE in a consecutive series of patients with Crohn’s was double that detected by CT enteroclysis (25 v 12/41; p<0.005) and these findings led to alteration of management in 10 patients with clinical improvement in all (see page 369). They suggest that the logic of designing slow release treatments that are only effective in the colon and terminal ileum for Crohn’s disease may be flawed. Their results also demonstrate that a normal terminal ileoscopy at colonoscopy does not exclude active small bowel Crohn’s disease higher up and also that a normal wireless capsule examination does not rule out the diagnosis of Crohn’s disease (lesions can be missed or not reached).
Because WCE appears superior to all current forms of radiological investigation of the small intestine in detecting the mucosal abnormalities of Crohn’s disease, one might imagine that there would be rapid adoption of this technique which does not expose patients to the hazards of repeated high dose x ray examinations and that radiological methods might be abandoned. There will be some hesitancy to do this for three reasons. There is anxiety that a capsule might become stuck or impacted against a stricture. The costs and manpower implications of changing from small bowel radiology to WCE will slow the rate of uptake. WCE will probably be less good than radiology at detecting fistulae and this might be a reason for occasionally choosing radiological investigations in preference to capsule examinations.
Addressing the stricture issue, capsule impaction does occur and the reported incidence was 2% in one large pooled series.25 Perhaps unexpectedly, most capsule impactions are asymptomatic and rarely produce obstructive symptoms of colicky abdominal pain, failure to pass gas, or vomiting. If the capsule is pointing forwards it may provide good images of the stricture. It is usually possible to tell if the capsule is pointing forwards as it passes through the pylorus and does not usually “tumble” once in the small intestine. For many patients, capsule impaction can be a good outcome as it can lead to surgery which can cure symptoms and also provide histological diagnoses, which are sometimes unexpected. Most recommend that if the capsule examination does not show images of the colon, and the patient does not notice the passage of the capsule in the stool, a plain abdominal x ray should be performed approximately seven days after the examination to check for capsule retention.
It would dampen enthusiasm for the use of wireless capsule examination in Crohn’s disease if a radiological study such as a CT enteroclysis had to precede every wireless capsule examination. Alternative options might include the use of a “patency capsule”, careful patient selection to avoid patients with symptoms suggestive of subacute obstruction, using capsules on a thread so that the capsule could be retrieved if it got stuck at a stricture, making a smaller diameter capsule, which might also be valuable in small children, and developing better retrieval methods.
A “patency” capsule has been developed (M2A patency; Given, Yoqneam, Israel) to detect possible strictures non-invasively which might lead to capsule retention. This device has identical dimensions to the M2A wireless capsule endoscope. It contains a small transponder in the form of a passive radiofrequency identification tag (RFID) and a dissolving body. Patency is verified if the capsule is excreted intact from the patient’s body. Excretion is tested before disintegration with a patency scanner, which emits a radiofrequency signal and detects the presence of the RFID tag in the patient’s body. If the capsule is retained in the gastrointestinal tract, it disintegrates into small, mostly soft, fragments which can easily pass through strictures
Clinical studies with the patency capsule are available at present in abstract form only. In one study, 61 patients ingested 63 patency capsules: 36 capsules were excreted intact (29/36 in less than 40 hours) and 27 disintegrated in the gastrointestinal tract. Of 54 patients who had radiographically indicated strictures, 31/54 passed the capsules intact. Fifteen patients who tested positively for patency were given the M2A video capsule, all of which passed naturally.26 These results suggest that this method might be used in patients with suspected Crohn’s disease strictures to allow safe use of the wireless capsule endoscope without prior radiological investigation, even in patients with strictures.
The absence of a “definition” of Crohn’s disease causes difficulties. Voderholzer and colleagues24 has suggested that the finding of more than 10 aphthous ulcers on a capsule examination is strongly suggestive of Crohn’s disease. It seems likely that a few patients with one or two aphthous ulcers may be found to have Crohn’s disease if they are followed up, but most will not. It is also apparent that a normal wireless capsule examination does not exclude Crohn’s disease as lesions are missed by this examination, as with any other, and because macroscopic mucosal abnormalities can heal completely and relapse later in the colon and are likely to do the same in the small intestine. The ultimate diagnosis of patients with a few aphthous ulcers in the small intestine on WCE, assuming such patients are not taking non-steroidal anti-inflammatory drugs, will require prospective studies.
Capsule endoscopy appears to be most valuable in its ability to diagnose early Crohn’s disease, and several studies have demonstrated its value in patients with suggestive symptoms but negative colonoscopy and radiology. It also has proved valuable in investigating children with symptoms suggestive of Crohn’s disease.20,21
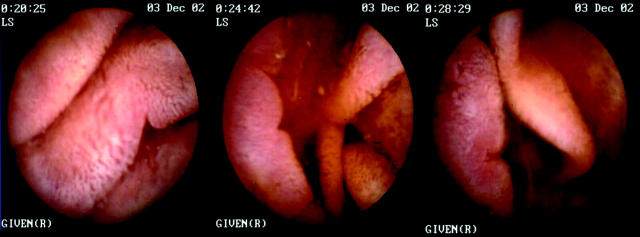
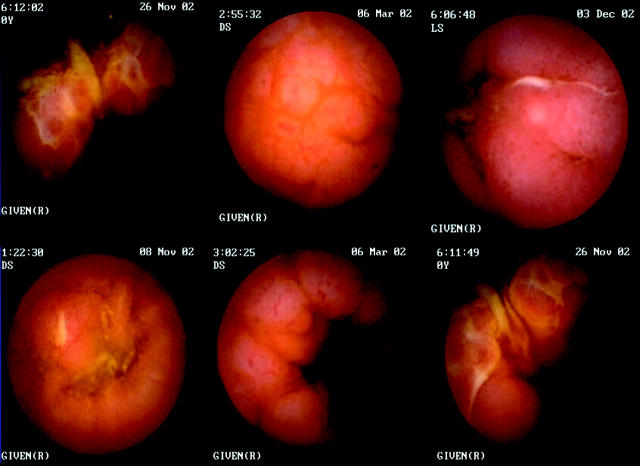
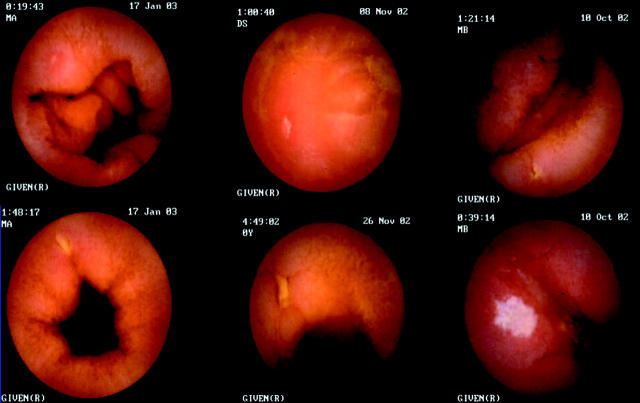
It may be possible to categorise early endoscopic appearances of small bowel Crohn’s disease from wireless capsule images as follows: notching of folds, a few small aphthous ulcers, larger ulcers, linear ulcers, circumferential involvement, abnormal vascularity, vasculitis, and even cobblestone appearances before radiological involvement can be demonstrated. The images in figs 1 ▶–4 ▶ were all taken from patients with normal small bowel radiology who improved clinically when treated for Crohn’s disease. Location, length of segment involvement, and small bowel transit information can be derived from the capsule images, localisation imager, and timer, although the capsule often does not move at a steady rate and frequently moves in a retrograde fashion.
Figure 1.
Notching on folds and notching with an inflammatory penumbra.
Figure 4.
Cobblestone appearances: nodularity with and without ulceration.
WCE does not yet feature a biopsy capacity. Such a function would be very valuable for management and diagnosis of small intestinal Crohn’s. The advent in Japan of a practical but demanding form of push enteroscopy with a double balloon system has allowed for the first time the possibility of taking directed biopsies under endoscopic visual control from the mid jejunum and upper ileum27 without surgery.
There is currently a problem with how best to use capsule endoscopy in patients with abdominal pain or irritable bowel-like syndrome symptoms. Some of these patients may have Crohn’s disease or perhaps coeliac disease but most will not have small intestinal pathology. The finding of one or two aphthous ulcers or erosions in patients during capsule endoscopy is common and it is likely that many of these do not have Crohn’s disease. It may be clinically expedient at present to avoid using WCE in patients with chronic abdominal pain unless they also have abnormal blood tests or other symptoms such as weight loss, as the incidence of clinically relevant small intestinal pathology is very low while minor clinically irrelevant abnormalities are common.28
It seems probable that the wireless capsule will have an increasing role in the investigation and management of Crohn’s disease and will be used in preference to radiological investigations using x rays. It is likely to be of most assistance in the early diagnosis, in determining the extent and sites of small intestinal involvement, and in examining patients with indeterminate colitis. It may also be valuable in differentiating Crohn’s from other causes of small intestinal disease, find a role as a radiation free method of follow up, and provide evidence about the cause of specific symptoms which might in turn lead to more logical therapy. The study published in this issue of Gut suggests that WCE is emerging from an early descriptive phase of astonishment that excellent images of small intestinal Crohn’s can be so easily acquired when radiological studies are normal and is beginning to learn how best to take advantage of the information which can be acquired from this technological advance.
Supplementary Material
Figure 2.
Aphthous and larger ulcers.
Figure 3.
Crohn’s vasculitis.
REFERENCES
- 1.Iddan G, Meron G, Glukhovsky A, et al. Wireless capsule endoscopy. Nature 2000;405:417. [DOI] [PubMed] [Google Scholar]
- 2.Appleyard M, Glukhovsky A, Swain P. Wireless-capsule diagnostic endoscopy for recurrent small-bowel bleeding. N Engl J Med 2001;344:232–3. [DOI] [PubMed] [Google Scholar]
- 3.Lewis BS, Swain P. Capsule endoscopy in the evaluation of patients with suspected small intestinal bleeding: Results of a pilot study. Gastrointest Endosc 2002;56:349–53. [DOI] [PubMed] [Google Scholar]
- 4.Ell C, Remke S, May A, et al. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy 2002;34:685–9. [DOI] [PubMed] [Google Scholar]
- 5.Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut 2003;52:1122–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pennazio M, Santucci R, Rondonotti .et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: Report of 100 consecutive cases. Gastroenterology 2004;216:643–53. [DOI] [PubMed] [Google Scholar]
- 7.Mata A, Llach J, Bordas JM, et al. Role of capsule endoscopy in patients with obscure digestive bleeding. Gastroenterol Hepatol 2003;26:619–23. [DOI] [PubMed] [Google Scholar]
- 8.Saurin JC, Delvaux M, Gaudin JL, et al. Diagnostic value of endoscopic capsule in patients with obscure digestive bleeding: Blinded comparison with push enteroscopy. Endoscopy 2003;35:576–84. [DOI] [PubMed] [Google Scholar]
- 9.Costamagna G, Shah SK, Riccioni ME, et al. A prospective trial comparing small bowel radiographs and video capsule endoscopy for suspected small bowel disease. Gastroenterology 2002;123:999–1005. [DOI] [PubMed] [Google Scholar]
- 10.Liangpunsakul S, Chadalawada V, Rex DK, et al. Wirelewss capsule endoscopy detects small bowel ulcers in patients with normal results from state of the art enteroclysis. Am J Gastroenterol 2003;98:1295–8. [DOI] [PubMed] [Google Scholar]
- 11.Voderholzer WA, Ortner M, Rogalla P, et al. Diagnostic yield of wireless capsule enteroscopy in comparison with computed tomographic enteroclysis. Endoscopy 2003;35:1009–14. [DOI] [PubMed] [Google Scholar]
- 12.Schreyer AG, Geissler A, Albrich H, et al. Abdominal MRI after enteroclysis or with oral contrast in patients with suspedted or proven Crohn’s disease. Clin Gastroenterol Hepatol 2004;6:491–7. [DOI] [PubMed] [Google Scholar]
- 13.Scapa E, Jacob H, Lewkowicz S, et al. Initial experience of wireless-capsule endoscopy for evaluating occult gastrointestinal bleeding and suspected small bowel pathology. Am J Gastroenterol 2002;97:2776–9. [DOI] [PubMed] [Google Scholar]
- 14.Fireman Z, Mahajna E, Broide E, et al. Diagnosing small bowel Crohn’s disease with wireless capsule endoscopy. Gut 2003;52:390–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herrerias JM, Caunedo A, Rodriguez-Tellez M, et al. Capsule endoscopy in patients with suspected Crohn’s disease and negative endoscopy. Endoscopy 2003;35:564–8. [DOI] [PubMed] [Google Scholar]
- 16.Mow WS, Lo SK, Targan SR, et al. Initial experience with wireless capsule enteroscopy in the diagnosis and management of inflammatory bowel disease. Clin Gastroenterol Hepatol 2004;2:31–40. [DOI] [PubMed] [Google Scholar]
- 17.Ge ZZ, Hu YB, Xiao SD. Capsule endoscopy in diagnosis of small bowel Crohn’s disease. World J Gastroenterol 2004;10:1349–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bowles CJ, Leicester R, Romaya C .et al. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut 2004;53:277–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hume G, Whittaker D, Radford-Smith G, et al. Can capsule endoscopy (CE) help differentiate the aetiolgy of indeterminate colitis? Conference proceedings of 3rd International Conference on Capsule Endoscopy, Miami, Florida, 2004;38A.
- 20.Lo SK. Capsule endoscopy in the diagnosis and management of inflammatory bowel disease. Gastrointest Endosc Clin N Am 2004;14:179–93. [DOI] [PubMed] [Google Scholar]
- 21.Seidman EG, Sant’Anna AM, Dirks MH. Potential applications of wireless capsule endoscopy in the pediatric age group. Gastrointest Endosc Clin N Am 2004;14:207–17. [DOI] [PubMed] [Google Scholar]
- 22.Arguelles AF, Arguelles MF, Caunedo AA, et al. Utility of capsule endoscopy in pediatric gastroenterology. An Pediatr (Barc) 2003;59:586–9. [DOI] [PubMed] [Google Scholar]
- 23.Reddy DN, Sriram PV, Rao GV, et al. Capsule endoscopy appearances of small-bowel tuberculosis. Endoscopy 2003;35:99. [DOI] [PubMed] [Google Scholar]
- 24.Voderholzer WA, Beinhoelzl J, Rogalla P, et al. Small bowel involvement in Crohn’s disease: a prospective comparison of wireless capsule endoscopy and computed tomography enteroclysis. Gut 2005;54:369–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Enns R, Mergender K, Brandabur J, et al. Capsule endoscopy CE: A multicentre, international review and comparison of capsule studies done in three different tertiary-care centres. Gastrointest Endosc 2003;57:AB101. [Google Scholar]
- 26.Bolvin M, Lochs H, Voderholzer W, et al. Evaluation of the Given patency system in the GI tract—results of a multicentre study. Conference proceedings of 3rd International Conference on Capsule Endoscopy, Miami, Florida, 2004;37A.
- 27.Yamamoto H, Sekine Y, Sato Y, et al. Total enteroscopy with a nonsurgical steerable double balloon method. Gastrointest Endosc 2001;53:216–20. [DOI] [PubMed] [Google Scholar]
- 28.Bardan E, Nadler M, Chowers Y, et al. Capsule endoscopy for the evaluation of patients with chronic abdominal pain. Endoscopy 2003;35:688–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.