Clinical presentation
A 32 year old, gravida 2, para 2, was admitted at 36 weeks’ gestation with upper abdominal pain. During her second pregnancy she frequently had epistaxis. At 39 weeks’ gestation she delivered a healthy girl after an elective caesarean section which was complicated by a total blood loss of 1.5 litres. Progressive liver failure and shock led to her transport to our hospital one day post partum. She had no history of alcohol abuse, viral hepatitis, and was not receiving any medications.
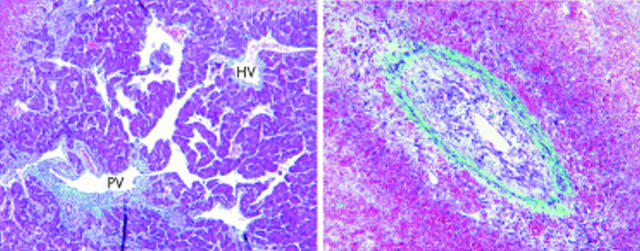
Continuing abdominal bleeding was suspected and at laparotomy 5 litres of blood were found in the abdominal cavity from sites of recently lysed adhesions. On day 4 post partum, liver failure worsened with grade IV encephalopathy necessary to perform an orthotopic liver transplantation. The procedure was complicated by severe intraoperative bleeding (30 litres). A section of the explanted liver is illustrated in fig 1 ▶. Postoperative follow up was complicated by intra-abdominal infections and steroid refractory chronic rejection leading to failure of the graft. She was successfully retransplanted four months later and is currently doing well.
Figure 1.
Question
What was the mechanism of liver failure in this patient?
See page 709 for answer
This case is submitted by: