The clinical implications of non-alcoholic fatty liver disease (NAFLD) are derived mostly from its common occurrence in the general population and the potential of the condition to progress to fibrosis and cirrhosis.1 Markers that help in making an early diagnosis and treatment are warranted. Protein C is a vitamin K dependent glycoprotein that functions as a circulating anticoagulant through proteolytic cleavage and inactivation of the coagulation factors Va and VIIIa.2 Whether or not protein C levels increase in patients with NAFLDs has not been assessed.
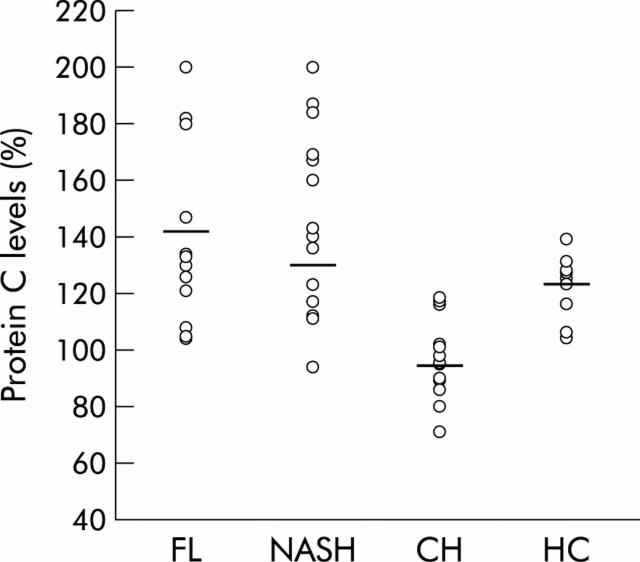
We measured protein C levels in 44 patients (28 men and 16 women; mean ages 45 (11) and 49 (12) years, respectively); 15 patients with fatty liver (FL), 15 with non-alcoholic steatohepatitis (NASH), and 14 with chronic viral hepatitis B+C (CH). All were diagnosed by histology and liver technetium scan or ultrasound. Ten healthy subjects were used as controls. Obesity, hyperlipidaemia, and diabetes were present in 60%, 73%, and 23% of cases, respectively; 64% of patients had elevated liver enzyme tests (alanine aminotransferase 45 (21) IU/l in FL and 43 (18) IU/l in NASH). Mean protein C levels were significantly increased in patients with NAFLD (n = 30) compared with those with chronic viral hepatitis (140 (36)% v 101 (24)%; p<0.0009) and healthy individuals (140 (36)% v 120 (12); p<0.04). No significant difference in protein C levels was noted between simple fatty liver and NASH. (149 (34)% and 130 (37)%, respectively; p = 0.07)). A significant correlation was found between protein C and extent of fatty infiltration (r = 0.63; p<0.001) (fig 1 ▶), insulin resistance index (r = 0.3; p<0.01), and triglyceride levels (r = 0.45, p<0.001). Protein C could discriminate correctly between NAFLDs and chronic viral hepatitis in 82% of cases. No significant association was found between protein C and aminotransferase levels.
Figure 1.
Protein C levels (normal 70–130%) in the study population (fatty liver (FL), non-alcoholic steatohepatitis (NASH), chronic viral hepatitis B+C (CH), and healthy controls (HC)). Horizontal bars indicate median levels.
In conclusion, protein C was elevated in patients with NAFLD. The underlying mechanism remains unknown. Agewall et al suggested an increase in hepatic synthesis of protein C due to increased hepatic insulin resistance.3 Increased levels have been reported in patients with diabetes, hypertriglyceridaemia, and nephrotic syndrome, with the use of anabolic steroids, oral contraceptives, and alcohol, and with increasing age.4 Diabetes and hypertriglyceridaemia are predisposing conditions to fatty liver5 and were present in 23% and 73% of cases, respectively. The remaining conditions were excluded by clinical and biochemical findings. Although more studies are needed, these preliminary findings suggest that elevated protein C levels together with elevated liver enzymes may be used as markers for NAFLD and may obviate the need for liver biopsy.
Conflict of interest: None declared.
References
- 1.Angulo P . Nonalcoholic fatty liver disease. N Engl J Med 2002;346:1221–31. [DOI] [PubMed] [Google Scholar]
- 2.Bajzar L . Thrombin activatable fibrinolysis inhibitor and an antifibrinolytic pathway. Arterioscler Thromb Vasc Biol 2000;20:2511–18. [DOI] [PubMed] [Google Scholar]
- 3.Agewall S, Bokemarket L, Wiskstrand J, et al. Insulin sensitivity and haemostatic factors in clinically healthy 58-year old men. Thromb Haemost 2000;84:571–5. [PubMed] [Google Scholar]
- 4.Bell H, Odegaard OR, Anderson T, et al. Protein C in patients with alcoholic cirrhosis and other liver diseases. J Hepatol 1992;14:163–7. [DOI] [PubMed] [Google Scholar]
- 5.Assy N, Kaita K, Mymin D, et al. Fatty infiltration of liver in hyperlipidemic patients. Dig Dis Sci 2000;45:1929–34. [DOI] [PubMed] [Google Scholar]