We present the case of a 49 year old man who had suffered histologically confirmed ulcerative colitis (UC) since 1998. He had been asymptomatic for four years when in August 2002 an acute relapse developed. Colonoscopy and histology of a superficial bowel specimen showed clear signs of active UC with no signs of malignancy. Despite adequate therapy he failed to improve and was referred for restorative proctocolectomy because of steroid dependency and end stage colon. By the time of his referral, violaceous reddish-brown nodules had developed on his extremities. Skin biopsy showed spindle cells and vascular slits. Histological diagnosis was Kaposi’s sarcoma (KS) of the skin. He underwent a restorative proctocolectomy with ileostomy in March 2003. The pathological examination of the colon showed features of UC and surprisingly, characteristic signs of KS also. Human immunodeficiency virus (HIV) tests were negative. Human herpesvirus-8 (HHV-8) DNA was detected in native samples from affected skin but not in peripheral blood or the large intestine. The patient recovered rapidly after operation. Steroid therapy was gradually withdrawn. Cutaneous lesions regressed completely with hyperpigmentation, and no new lesions were observed, despite receiving no treatment (fig 1 ▶).
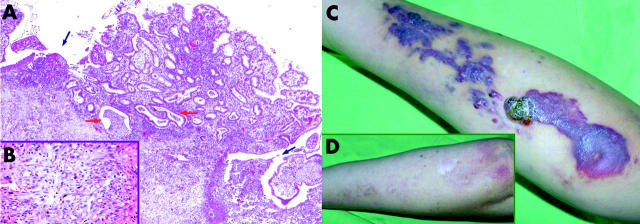
Figure 1.
(A) Histological signs of ulcerative colitis and Kaposi’s sarcoma (KS) from the resected colon. Ulcers (blue arrows) at the base of a pseudopolyp and crypt abscesses (red arrows) can be seen (haematoxylin-eosin staining, 100× magnification). (B) Typical features of KS can be identified in the submuscular connective tissue layer of the colon (haematoxylin-eosin staining, 400× magnification). (C) Kaposi’s sarcoma on the forearm of the patient, and the same region a year after operation (D).
There are four clinical variants of KS: classic, endemic, acquired immunodeficiency syndrome (AIDS) associated, and iatrogenic.1 Excessive use of immunosuppressive drugs in the second part of the 20th century has been associated with a higher prevalence of iatrogenic KS.2 Start of the disease, after administration of the triggering drug in previously reported studies, ranged from less than one month to more than 20 years. The dose of steroid ranged from 5 to 125 mg/day. There was no evident correlation between the development of KS and dose or duration of steroid therapy.3 Our patient had been treated with 12–125 mg methylprednisolone daily for about four months when his skin lesions appeared. Reduction or discontinuation of immunosuppressive drugs often leads to considerable improvement in KS lesions.4,5 In accordance with these data, after withdrawal of steroid therapy the skin symptoms of our patient regressed spontaneously. Visceral KS is quite frequent in AIDS patients and can affect virtually all viscera, but colonic KS is rare. These patients are often asymptomatic or have aspecific symptoms.6 As KS affects the submucosa more often, superficial bowel biopsies frequently miss it, as happened in our case. A link between HHV-8, a gamma herpesvirus, and KS was first reported more than 10 years ago.7,8 The virus was found in more than 90% of KS samples from HIV seropositive patients but it has low prevalence in healthy controls. HHV-8 DNA persists in endothelial cells and spindle cells of KS. According to the literature, the HHV-8 virus alone is not sufficient to form KS but it may be an important cofactor in the development of the disease. In our case, we detected HHV-8 genome in native samples from skin lesions but failed to do so in paraffin embedded colonic samples. The occurrence of colonic KS and UC together is rare. We found eight similar cases in the English literature (table 1 ▶).
Table 1.
Main data from previously published articles on the coexistence of colonic Kaposi’s sarcoma (KS) and ulcerative colitis (UC)
| Reference | Year of publication | HIV status | Pathology of the colon | Skin lesion | Treatment |
| Gordon9 | 1966 | No information | UC | No | Colectomy |
| Adlersberg10 | 1970 | No infoarmation | Non-specific colitis | No | Colectomy |
| Roth11 | 1978 | No information | Segmental non-specific colitis | Yes | Subtotal colectomy |
| Weber12 | 1985 | Positive | Non-specific colitis of the rectosigmoid colon, separate lesion in the caecum | Yes | Alpha interferon+radiotherapy of rectal KS |
| Biggs13 | 1987 | Positive | UC | Yes | Urgent colectomy for toxic megacolon and later abdominoperineal excision for rectal KS |
| Meltzer14 | 1987 | Negative | UC distal to the descendent colon | Yes | Proctocolectomy with ileostomy |
| Thompson15 | 1989 | Negative | UC | No | Restorative proctocolectomy |
| Tedesco16 | 1999 | Negative | UC | No | Restorative proctocolectomy |
Our patient was the fourth who was HIV negative and developed KS in association with UC. To our knowledge he was the first proven HHV-8 positive case who developed disseminated KS during immunosuppressive treatment for UC. Our treatment policy was successful. The patient, in spite of his poor condition, tolerated the surgical therapy well. After cessation of his steroid therapy KS regressed spontaneously. He remains well 35 months after surgery.
Acknowledgments
We would like to express our thank to Professor Péter Kupcsulik for revision of the manuscript.
Conflict of interest: None declared.
References
- 1.Martin RW III, Hood AF, Farmer ER. Kaposi sarcoma. Medicine 1993;72:245–61. [DOI] [PubMed] [Google Scholar]
- 2.Frances C. Kaposi’s sarcoma after renal transplantation. Nephrol Dial Transplant 1998;13:2768–73. [DOI] [PubMed] [Google Scholar]
- 3.Trattner A, Hodak E, David M, et al. The appearance of Kaposi sarcoma during corticosteroid therapy. Cancer 1993;72:1779–83. [DOI] [PubMed] [Google Scholar]
- 4.Wijnveen AC, Persson H, Björck S, et al. Disseminated Kaposi’s sarcoma—full regression after withdrawal of immunosuppressive therapy: report of a case. Transplant Proc 1987;19:3735–6. [PubMed] [Google Scholar]
- 5.Duman S, Töz H, Aşçi G, et al. Successful treatment of post-transplant Kaposi’s sarcoma by reduction of immunosuppression. Nephrol Dial Transplant 2002;17:892–6. [DOI] [PubMed] [Google Scholar]
- 6.Saltz RK, Kurtz RC, Lightdale CJ, et al. Gastrointestinal involvement in Kaposi’s sarcoma. Gastroenterology 1982;82:1168. [Google Scholar]
- 7.Chang Y, Cesarman E, Pessin MS, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi’s sarcoma. Science 1994;266:1865–9. [DOI] [PubMed] [Google Scholar]
- 8.Kemény L, Gyulai R, Kiss M, et al. Kaposi’s sarcoma-associated herpesvirus/human herpesvirus-8: a new virus in human pathology. J Am Acad Dermatol 1997;37:107–13. [DOI] [PubMed] [Google Scholar]
- 9.Gordon HW, Rywlin AM. Kaposi’s sarcoma of the large intestine associated with ulcerative colitis: A hitherto unreported occurrence. Gastroenterology 1966;50:248–53. [Google Scholar]
- 10.Adlersberg R. Kaposi’s sarcoma complicating ulcerative colitis: report of a case. Am J Clin Pathol 1970;54:143–6. [DOI] [PubMed] [Google Scholar]
- 11.Roth JA, Schell S, Panzarino S, et al. Visceral Kaposi’s sarcoma presenting as colitis. Am J Surg Pathol 1978;2:209–14. [DOI] [PubMed] [Google Scholar]
- 12.Weber JN, Carmichael DJ, Boylston A, et al. Kaposi’s sarcoma of the bowel presenting as apparent ulcerative colitis. Gut 1985;26:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Biggs BA, Crowe SM, Lucas CR, et al. AIDS related Kaposi’s sarcoma presenting as ulcerative colitis and complicated by toxic megacolon. Gut 1987;28:1302–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meltzer SJ, Rotterdam HZ, Korelitz BI. Kaposi’s sarcoma occurring in association with ulcerative colitis. Am J Gastroenterol 1987;82:378–81. [PubMed] [Google Scholar]
- 15.Thompson GB, Pemberton JH, Morris S, et al. Kaposi’s sarcoma of the colon in a young HIV-negative man with chronic ulcerative colitis. Report of a case. Dis Colon Rectum 1989;32:73–6. [DOI] [PubMed] [Google Scholar]
- 16.Tedesco M, Benevolo M, Frezza F, et al. Colorectal Kaposi’s sarcoma in an HIV-negative male in association with ulcerative rectocolitis: a case report. Anticancer Res 1999;19:3045–8. [PubMed] [Google Scholar]