Distal intestinal obstruction syndrome (DIOS) occurs in 15.9% of adults with cystic fibrosis (CF).1 Usually the diagnosis is based on history, physical examination, and plain abdominal roentgenogram. The increased risk of gastrointestinal complications such as DIOS is well known after lung transplantation.2,3 Due to the added risk of gastrointestinal surgery in the postoperative period4 and the generally good response to conservative treatment, it is necessary to distinguish DIOS from other gastrointestinal complications. Nevertheless, descriptions of computed tomographical patterns of DIOS in the international literature are rare.5
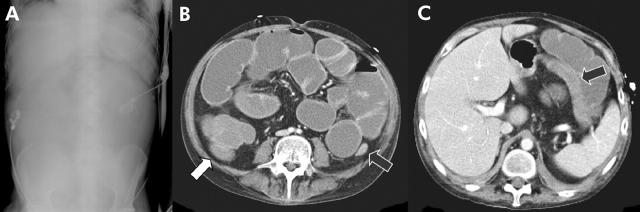
We present the case of a 34 year old male suffering from end stage CF. Because of gastrointestinal manifestations of CF, the patient had exocrine pancreas insufficiency. As a consequence of deterioration in respiratory function, lung transplantation was performed. Despite enzymatic and propulsive medical treatment the patient developed an acute abdomen during the postoperative period. To determine the cause of his symptoms abdominal radiographs and computed tomography were performed. Abdominal plain films showed remarkably little abdominal gas and poor delineation of the abdominal organs (fig 1A ▶). Contrast enhanced computed tomography showed massive dilatation of the small bowel and proximal colon with marked swelling of the intestinal wall (fig 1B, C ▶). The lumen of the small intestine and proximal part of the ascending colon were filled with a homogeneous mass (fig 1B ▶) with increasing roentgen opacity from the duodenum (approximately 19 Hounsfield units (HU)) to the right hemicolon (approximately 39 HU). Isolated air fluid levels were seen in the small bowel. The transverse, descending, and sigmoid colon were thin with only little faeces. There was no evidence of external compression. Based on these findings a diagnosis of DIOS was made. Laparotomy, performed due to failure of medical treatment, confirmed the diagnosis.
Figure 1.
(A–C) Abdominal plain film showing remarkably little abdominal gas and poor delineation of the abdominal organs. Markedly distended small bowel loops and right hemicolon (white arrow) completely filled with a homogenous mass. Swelling of the intestinal wall with increased contrast medium enhancement. Thin transverse and descending colon with only few faeces (black arrows).
DIOS is unique to patients with cystic fibrosis. Intestinal obstruction developed due to accumulation of highly viscous muco-faeculent material in the terminal ileum and right hemicolon. Pancreatic insufficiency is a prerequisite for DIOS but is not its only pathophysiological cause. Other factors such as reduced intestinal water content, lower luminal acidity of the foregut, accumulation of intraluminal macromolecules, dehydration of the mucus layer due to altered intestinal secretion, and slow intestinal transit contribute to the development of DIOS.1,6
Plain films are only of limited value in differentiating DIOS from other causes of acute abdomen. In the case of DIOS, they usually show typical signs of a small bowel ileus but other frequent reasons for ileus in patients with CF (for example, adhesions,3 intussusception,7 paralytic ileus due to perforated appendicitis,8 or Crohn’s disease8) cannot be excluded without further investigation. In our case, abdominal plain films showed no typical signs of small bowel ileus but little abdominal gas with poor delineation of the abdominal organs leading to the differential diagnoses of ascites, colitis, mesenteric infarction, and proximal bowel obstruction. In contrast with the plain abdominal radiograph, computed tomography showed the criteria of DIOS. The small bowel was completely filled with a homogenous mass with increasing roentgen opacity from the duodenum (approximately 19 HU) to the right hemicolon (approximately 39 HU), suggesting increasing viscosity of the intestinal content due to water absorption. In accordance with previous descriptions of DIOS,3 obstruction occurred in the right hemicolon.
Our case showed that abdominal plain films, as used in previous studies, are not adequate for the diagnosis of DIOS. Computed tomography can reveal the characteristic signs of DIOS and exclude inherent differential diagnoses. We have demonstrated for the first time that DIOS causes increasing opacity of intestinal contents during small intestinal passage, suggesting increasing viscosity.
Conflict of interest: None declared.
References
- 1.Dray X, Bienvenu T, Desmazes-Dufu N, et al. Distal intestinal obstruction syndrome in adults with cystic fibrosis. Clin Gastroenterol Hepatol 2004;2:498–503. [DOI] [PubMed] [Google Scholar]
- 2.Gillijam M, Chaparro C, Tullis E, et al. GI complications after lung transplantation in patients with cystic fibrosis. Chest 2003;1:37–41. [DOI] [PubMed] [Google Scholar]
- 3.Minkes RK, Langer JC, Skinner MA, et al. Intestinal obstruction after lung transplantation in children with cystic fibrosis. J Pediatr Surg 1999;10:1489–93. [DOI] [PubMed] [Google Scholar]
- 4.Rescorla FJ, Grosfeld JL. Contemporary management of meconium ileus. World J Surg 1993;17:318–25. [DOI] [PubMed] [Google Scholar]
- 5.Moody AR, Haddock JA, Given-Wilson R, et al. CT monitoring of therapy for meconium ileus. J Comput Assist Tomogr 1990;14:1010–12. [DOI] [PubMed] [Google Scholar]
- 6.Eggermont E. Gastrointestinal manifestations in cystic fibrosis. Eur J Gastroenterol Hepatol 1996;8:731–8. [PubMed] [Google Scholar]
- 7.Khera G, Kumarage S, Strekozov B. Adult intussusception in a cystic fibrosis patient-mimicking acute appendicitis. Aust NZ J Surg 2004;74:807–11. [DOI] [PubMed] [Google Scholar]
- 8.Chaum C. Colonic disorders in adult cystic fibrosis. Can J Gastroenterol 2001;15:586–90. [DOI] [PubMed] [Google Scholar]