Abstract
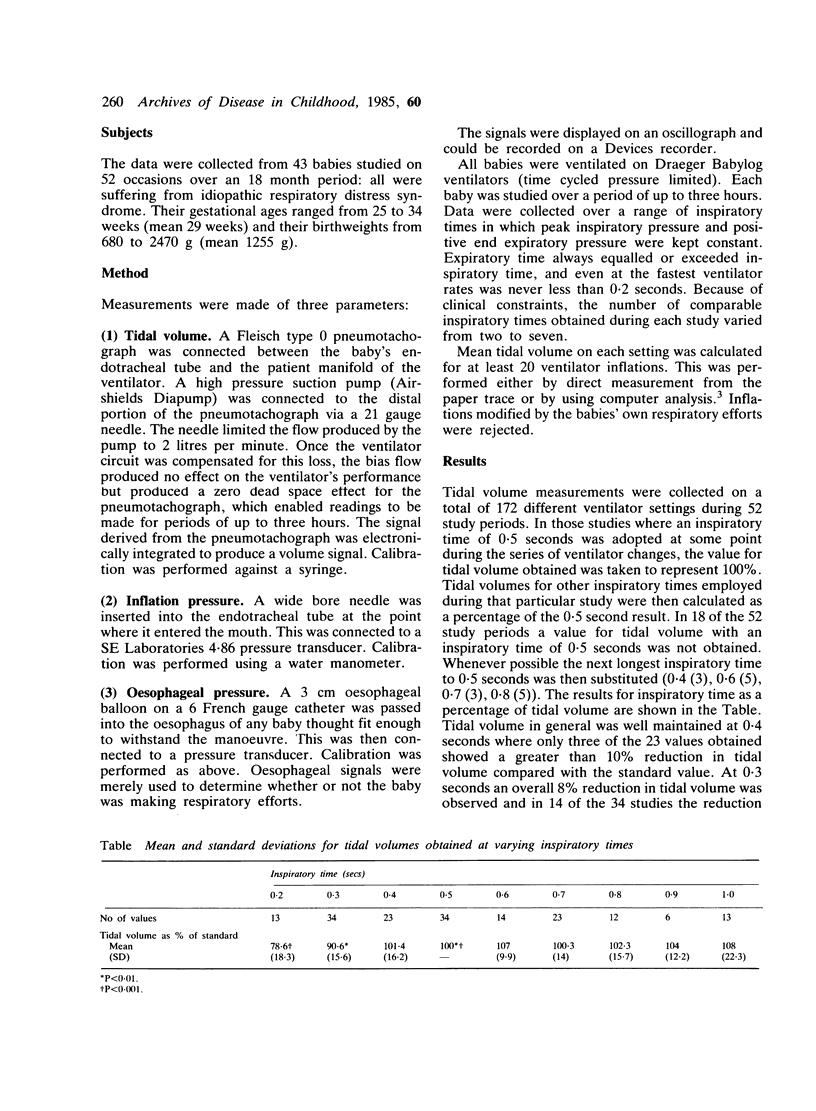
We measured the tidal volume achieved during intermittent positive pressure ventilation using various inspiratory times with a minimum of 0.2 seconds. Results indicate that tidal volume shows no reduction with inspiratory times down to 0.4 seconds. An inspiratory time of 0.3 seconds, however, is likely to reduce tidal volume by 8%, and at 0.2 seconds a 22% fall may be anticipated.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Field D., Milner A. D., Hopkin I. E. High and conventional rates of positive pressure ventilation. Arch Dis Child. 1984 Dec;59(12):1151–1154. doi: 10.1136/adc.59.12.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds E. O. Effect of alterations in mechanical ventilator settings on pulmonary gas exchange in hyaline membrane disease. Arch Dis Child. 1971 Apr;46(246):152–159. doi: 10.1136/adc.46.246.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes G. M., Milner A. D., Hodges I. G., Henry R. L., Elphick M. C. Nebulised therapy in acute severe bronchiolitis in infancy. Arch Dis Child. 1983 Apr;58(4):279–282. doi: 10.1136/adc.58.4.279. [DOI] [PMC free article] [PubMed] [Google Scholar]



