Abstract
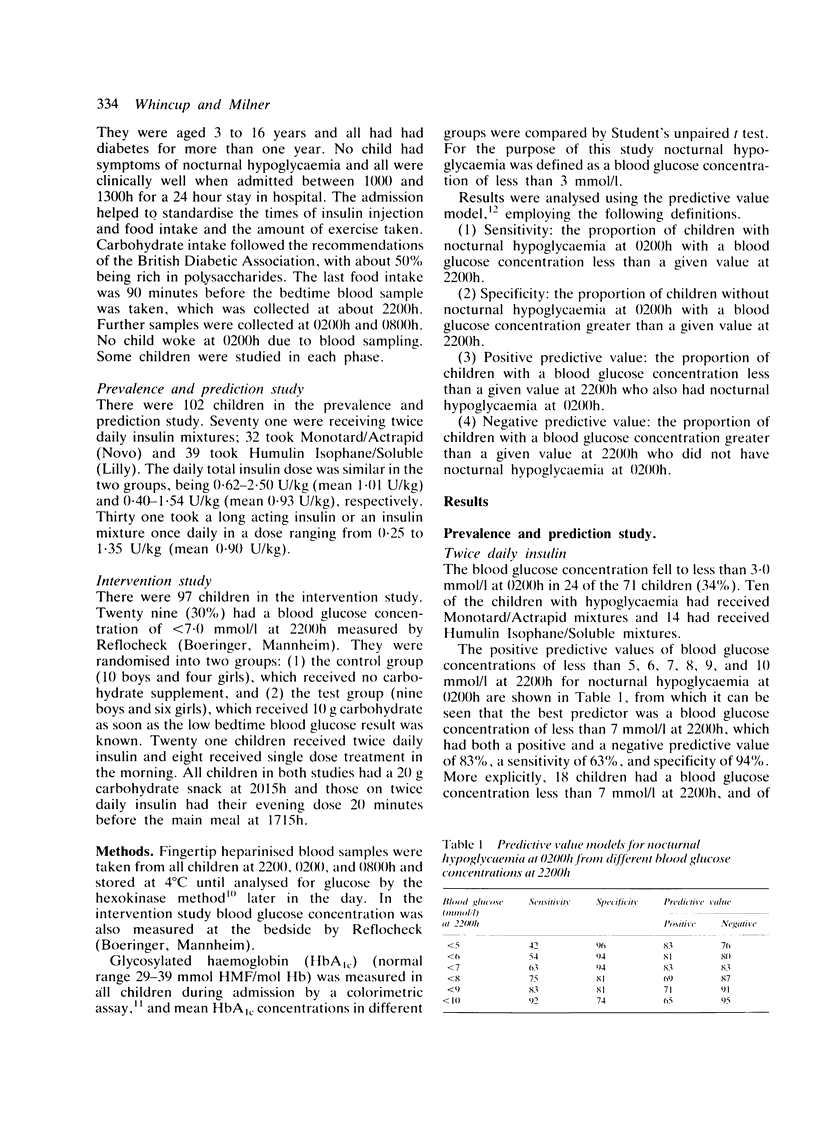
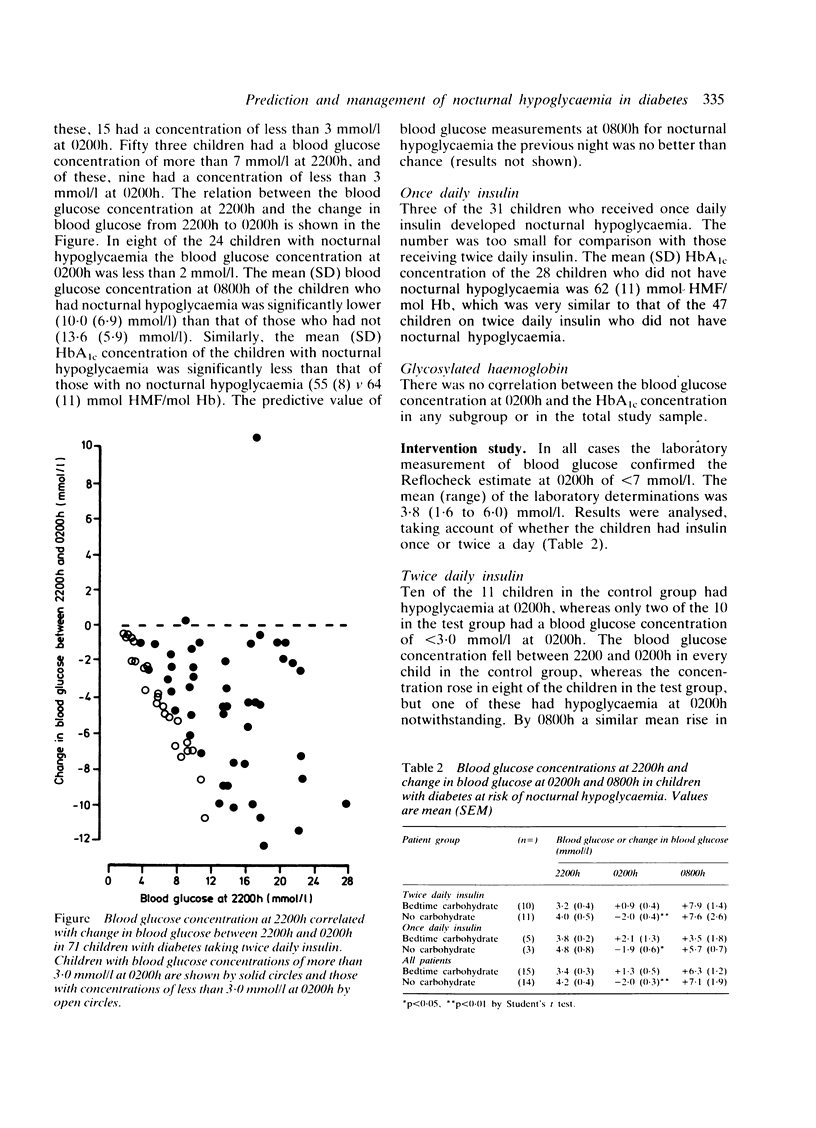
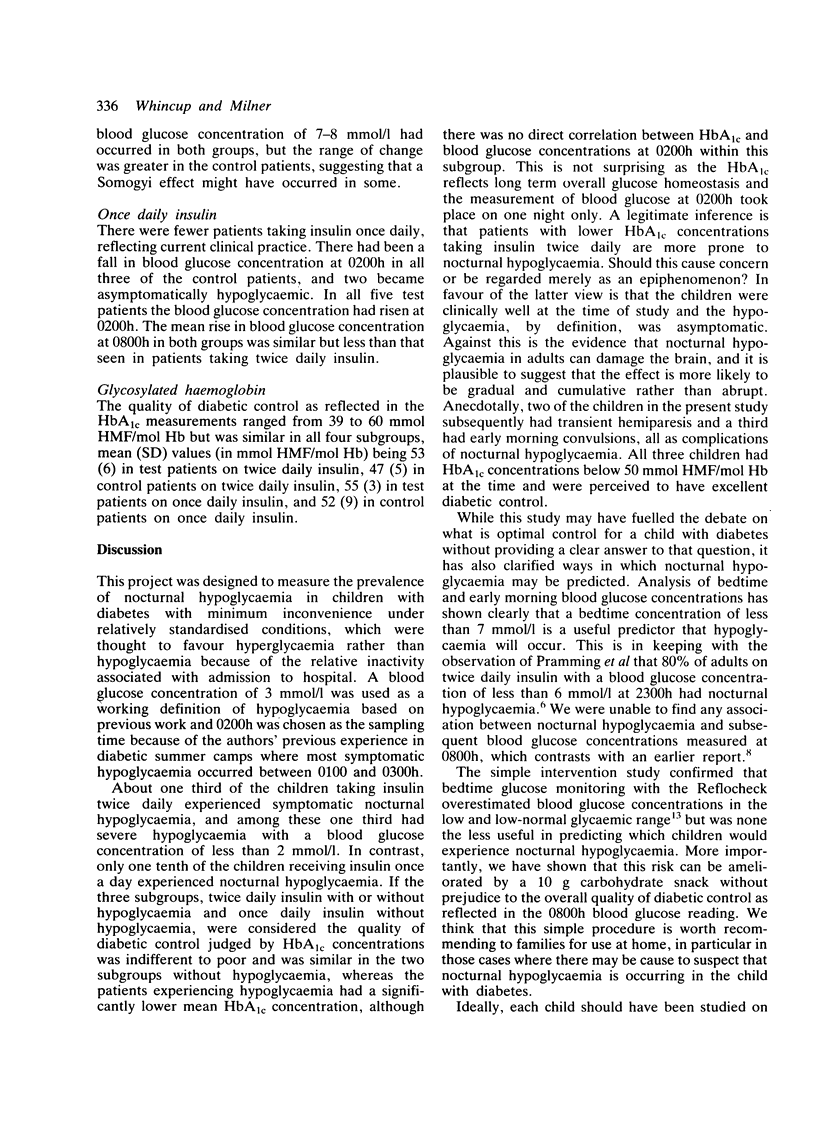
Blood glucose measurements were made at 2200, 0200, and 0800 h in 102 children with diabetes during a 24 hour planned admission to hospital. Nocturnal hypoglycaemia (less than 3.0 mmol/l) occurred in 24 of 71 (34%) children on twice daily insulin and in three of 31 (10%) children on once daily insulin. Predictive value modelling showed that a blood glucose concentration of less than 7 mmol/l at 2200 h was the best predictor of nocturnal hypoglycaemia, with a sensitivity of 63%, specificity of 94%, and positive and negative predictive values of 83%. Blood glucose measurement at 0800 h had no predictive value for nocturnal hypoglycaemia. The mean (SD) glycosylated haemoglobin concentration of children on twice daily insulin who had nocturnal hypoglycaemia was 55 (8) mmol HMF/mol Hb, which was significantly less than that of children on twice daily insulin who did not have hypoglycaemia (64 (11) mmol HMF/mol Hb) or those on once daily insulin (62 (11) mmol HMF/mol Hb). A controlled trial was then performed in which 29 children with diabetes who had a blood glucose concentration at 2200 h of less than 7 mmol/l measured by Reflocheck were randomised into two groups, one of which received 10 g carbohydrate supplement and the other of which did not. Thirteen of the 14 children in the control group had hypoglycaemia at 0200 h, whereas the snack prevented hypoglycaemia in 12 of 15 in the test group. Blood glucose values in the two groups at 0800 h were similar. We conclude that bedtime glucose measurement in children on twice daily insulin is a useful predictor for nocturnal hypoglycaemia, which can be prevented by a small carbohydrate snack in those at risk.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baumer J. H., Edelsten A. D., Howlett B. C., Owens C., Pennock C. A., Savage D. C. Impact of home blood glucose monitoring on childhood diabetes. Arch Dis Child. 1982 Mar;57(3):195–199. doi: 10.1136/adc.57.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bondar R. J., Mead D. C. Evaluation of glucose-6-phosphate dehydrogenase from Leuconostoc mesenteroides in the hexokinase method for determining glucose in serum. Clin Chem. 1974 May;20(5):586–590. [PubMed] [Google Scholar]
- Flückiger R., Winterhalter K. H. In vitro synthesis of hemoglobin AIc. FEBS Lett. 1976 Dec 1;71(2):356–360. doi: 10.1016/0014-5793(76)80969-6. [DOI] [PubMed] [Google Scholar]
- Pramming S., Thorsteinsson B., Bendtson I., Rønn B., Binder C. Nocturnal hypoglycaemia in patients receiving conventional treatment with insulin. Br Med J (Clin Res Ed) 1985 Aug 10;291(6492):376–379. doi: 10.1136/bmj.291.6492.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramasamy R. Unrecognised nocturnal hypoglycaemia masquerading as senile dementia. Postgrad Med J. 1983 Sep;59(695):575–577. doi: 10.1136/pgmj.59.695.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbloom A. L., Giordano B. P. Chronic overtreatment with insulin in children and adolescents. Am J Dis Child. 1977 Aug;131(8):881–885. doi: 10.1001/archpedi.1977.02120210059012. [DOI] [PubMed] [Google Scholar]
- Silas J. H., Grant D. S., Maddocks J. L. Transient hemiparetic attacks due to unrecognised nocturnal hypoglycaemia. Br Med J (Clin Res Ed) 1981 Jan 10;282(6258):132–133. doi: 10.1136/bmj.282.6258.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vecchio T. J. Predictive value of a single diagnostic test in unselected populations. N Engl J Med. 1966 May 26;274(21):1171–1173. doi: 10.1056/NEJM196605262742104. [DOI] [PubMed] [Google Scholar]
- Winter R. J. Profiles of metabolic control in diabetic children-frequency of asymptomatic nocturnal hypoglycemia. Metabolism. 1981 Jul;30(7):666–672. doi: 10.1016/0026-0495(81)90081-0. [DOI] [PubMed] [Google Scholar]


