Abstract
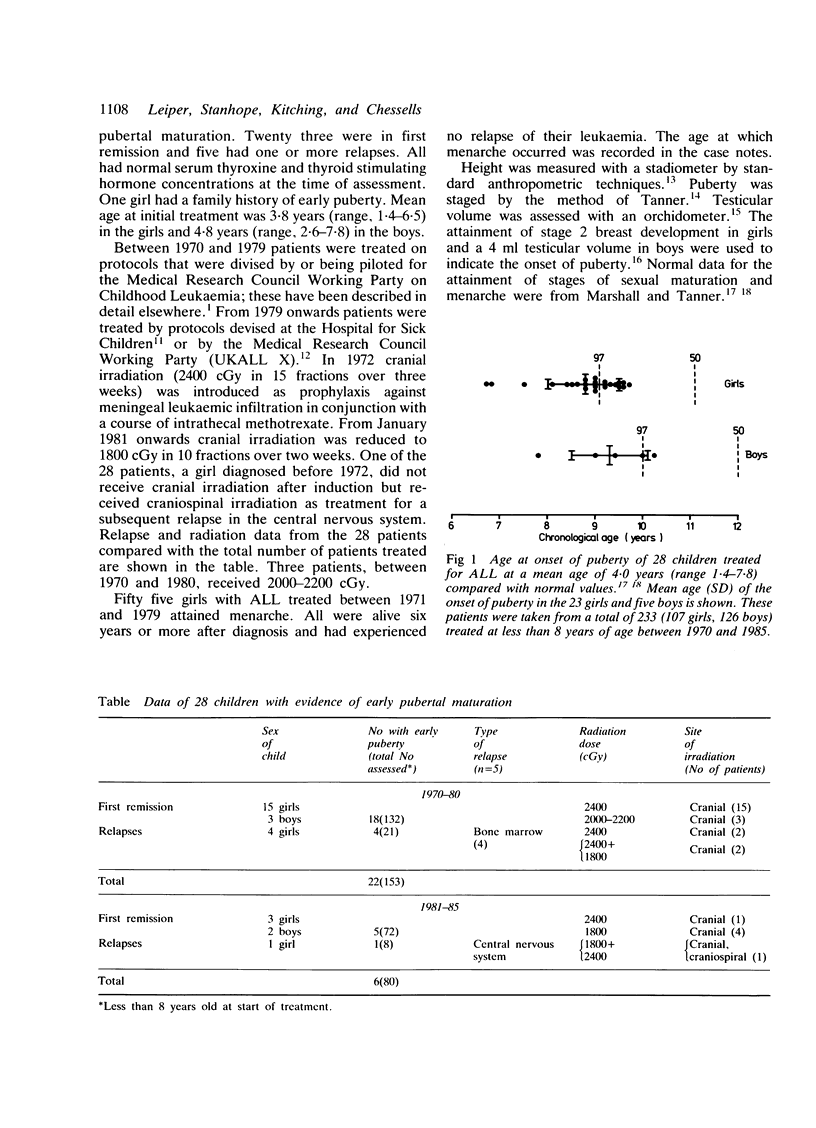
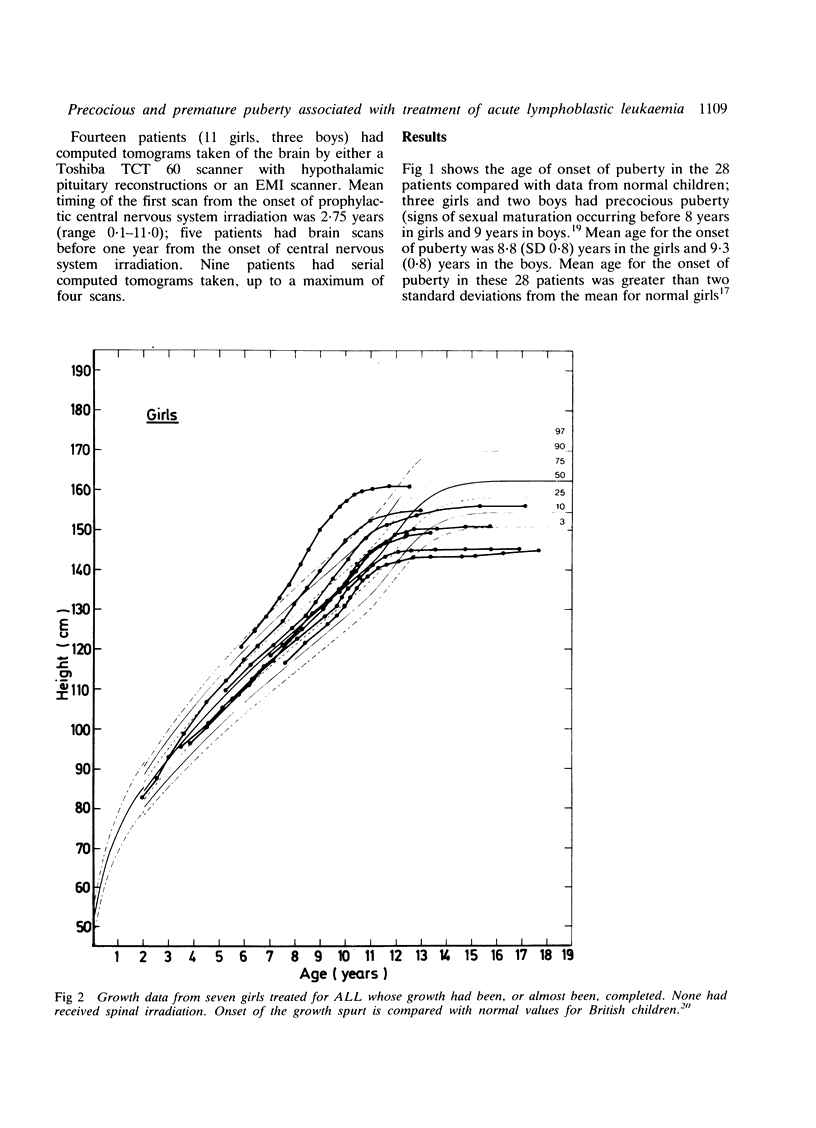
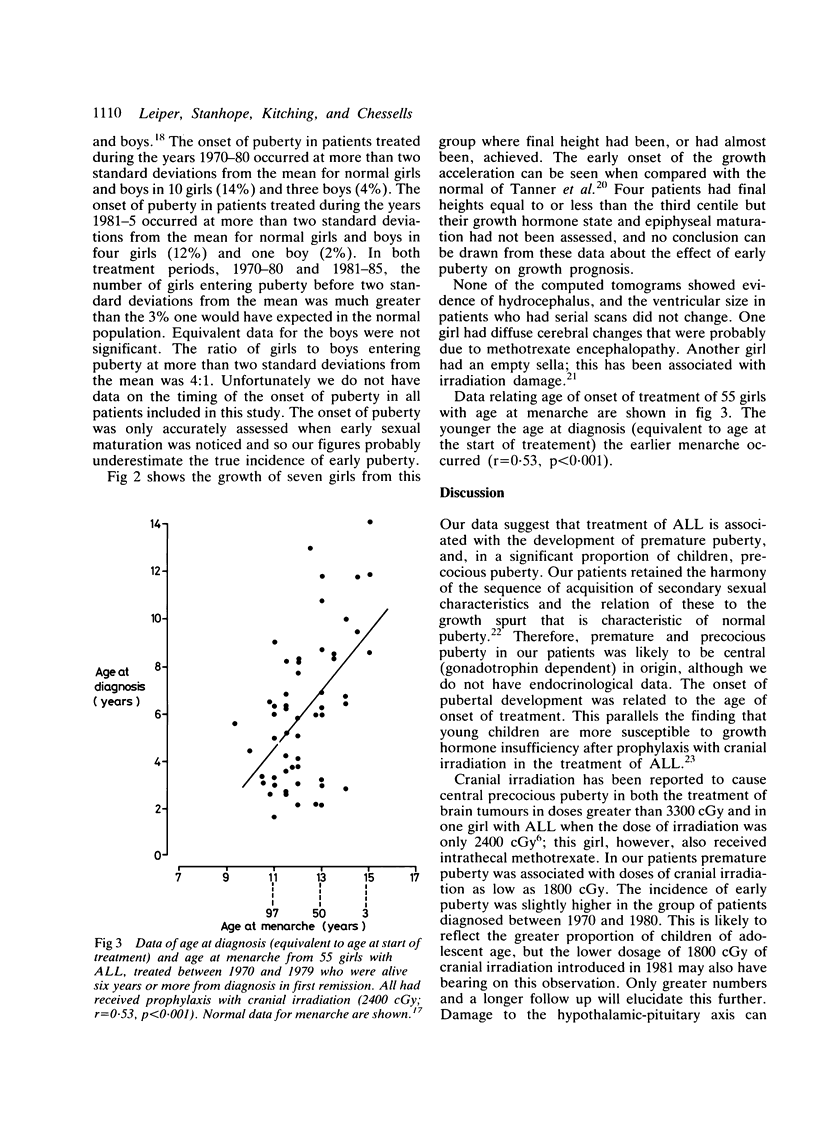
Early puberty in 28 children (23 girls, five boys) treated for acute lymphoblastic leukaemia (ALL) at a mean age of 4.0 years (range 1.4-7.8) is described. All but one had received prophylactic cranial irradiation (1800-2400 cGy) and three children had received additional cranial or craniospinal irradiation as treatment for relapse of their leukaemia. Mean age for the onset of puberty was 8.8 (SD 0.8) years in the girls and 9.3 (0.8) years in the boys; this is greater than two standard deviations from the mean for normal girls and boys. Five children (three girls, two boys) had precocious puberty. The onset of puberty occurred at greater than two standard deviations from the mean for normal girls and boys in 14(13%) girls and 4(3%) boys treated at less than eight years of age between 1970 and 1985. In a group of 55 girls treated for ALL who had survived in first remission for six years or more from diagnosis, there was a relation between young age at onset of treatment and early menarche. We suggest that premature activation of the hypothalamic-pituitary-gonadal axis occurs as a consequence of hypothalamic dysfunction due to cranial irradiation. Precocious and premature puberty in children treated for ALL may be an important factor in contributing to short stature.
Full text
PDF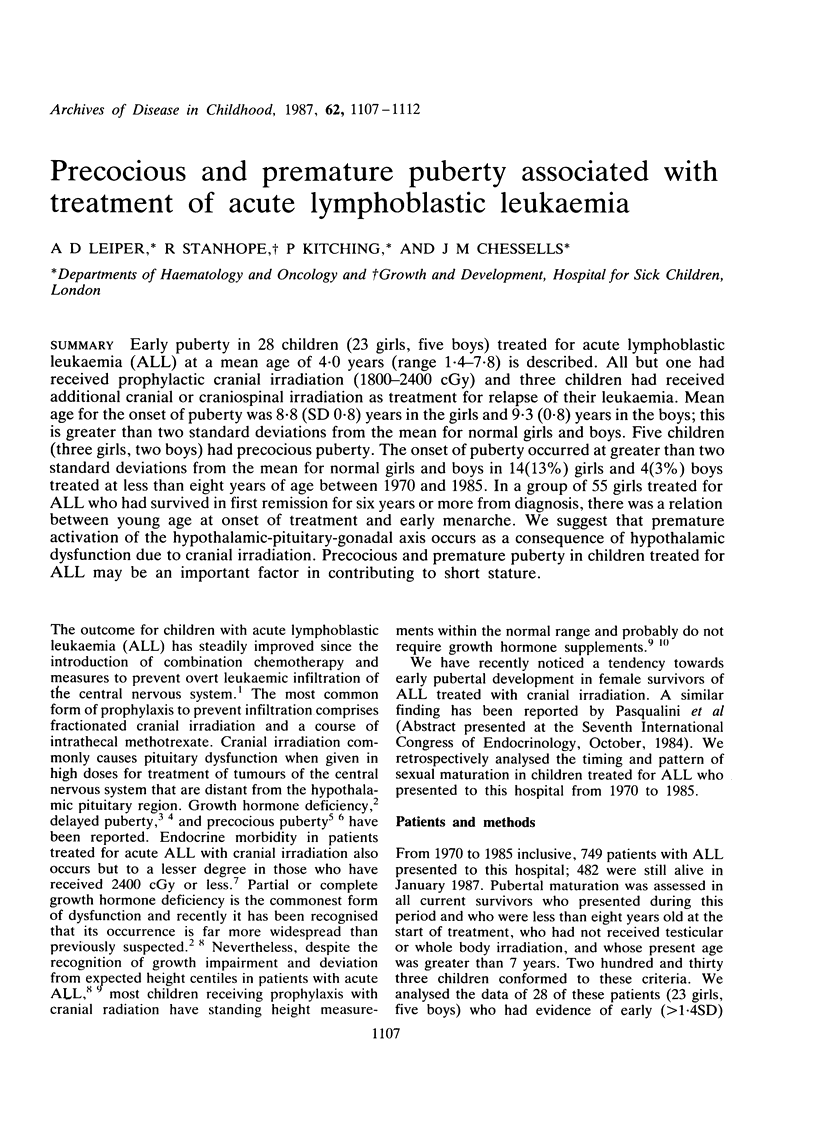

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brauner R., Czernichow P., Rappaport R. Greater susceptibility to hypothalamopituitary irradiation in younger children with acute lymphoblastic leukemia. J Pediatr. 1986 Feb;108(2):332–332. doi: 10.1016/s0022-3476(86)81027-7. [DOI] [PubMed] [Google Scholar]
- Brauner R., Czernichow P., Rappaport R. Precocious puberty after hypothalamic and pituitary irradiation in young children. N Engl J Med. 1984 Oct 4;311(14):920–920. doi: 10.1056/NEJM198410043111414. [DOI] [PubMed] [Google Scholar]
- Brauner R., Rappaport R. Precocious puberty secondary to cranial irradiation for tumors distant from the hypothalamo-pituitary area. Horm Res. 1985;22(1-2):78–82. doi: 10.1159/000180076. [DOI] [PubMed] [Google Scholar]
- Chessells J. M., Ninane J., Tiedemann K. Present problems in management of childhood lymphoblastic leukaemia: experience from the Hospital for Sick Children, London. Haematol Blood Transfus. 1981;26:108–114. doi: 10.1007/978-3-642-67984-1_16. [DOI] [PubMed] [Google Scholar]
- Marshall W. A., Tanner J. M. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969 Jun;44(235):291–303. doi: 10.1136/adc.44.235.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall W. A., Tanner J. M. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970 Feb;45(239):13–23. doi: 10.1136/adc.45.239.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkerton C. R., Bowman A., Holtzel H., Chessells J. M. Intensive consolidation chemotherapy for acute lymphoblastic leukaemia (UKALL X pilot study). Arch Dis Child. 1987 Jan;62(1):12–18. doi: 10.1136/adc.62.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rappaport R., Brauner R., Czernichow P., Thibaud E., Renier D., Zucker J. M., Lemerle J. Effect of hypothalamic and pituitary irradiation on pubertal development in children with cranial tumors. J Clin Endocrinol Metab. 1982 Jun;54(6):1164–1168. doi: 10.1210/jcem-54-6-1164. [DOI] [PubMed] [Google Scholar]
- Robison L. L., Nesbit M. E., Jr, Sather H. N., Meadows A. T., Ortega J. A., Hammond G. D. Height of children successfully treated for acute lymphoblastic leukemia: a report from the Late Effects Study Committee of Childrens Cancer Study Group. Med Pediatr Oncol. 1985;13(1):14–21. doi: 10.1002/mpo.2950130105. [DOI] [PubMed] [Google Scholar]
- Shalet S. M., Beardwell C. G., Twomey J. A., Jones P. H., Pearson D. Endocrine function following the treatment of acute leukemia in childhood. J Pediatr. 1977 Jun;90(6):920–923. doi: 10.1016/s0022-3476(77)80559-3. [DOI] [PubMed] [Google Scholar]
- Shalet S. M. Irradiation-induced growth failure. Clin Endocrinol Metab. 1986 Aug;15(3):591–606. doi: 10.1016/s0300-595x(86)80011-1. [DOI] [PubMed] [Google Scholar]
- Stanhope R., Adams J., Brook C. G. Disturbances of puberty. Clin Obstet Gynaecol. 1985 Sep;12(3):557–577. [PubMed] [Google Scholar]
- Stanhope R., Adlard P. Empty sella syndrome. Dev Med Child Neurol. 1987 Jun;29(3):397–399. doi: 10.1111/j.1469-8749.1987.tb02494.x. [DOI] [PubMed] [Google Scholar]
- Stanhope R., Brook C. G. Clinical diagnosis of disorders of puberty. Br J Hosp Med. 1986 Jan;35(1):57–58. [PubMed] [Google Scholar]
- Werder E. A., Mürset G., Zachmann M., Brook C. G., Prader A. Treatment of precocious puberty with cyproterone acetate. Pediatr Res. 1974 Apr;8(4):248–256. doi: 10.1203/00006450-197404000-00006. [DOI] [PubMed] [Google Scholar]
- Winter J. S., Faiman C. Pituitary-gonadal relations in male children and adolescents. Pediatr Res. 1972 Feb;6(2):126–135. doi: 10.1203/00006450-197202000-00006. [DOI] [PubMed] [Google Scholar]
- Zachmann M., Prader A., Kind H. P., Häfliger H., Budliger H. Testicular volume during adolescence. Cross-sectional and longitudinal studies. Helv Paediatr Acta. 1974 Apr;29(1):61–72. [PubMed] [Google Scholar]


