Abstract
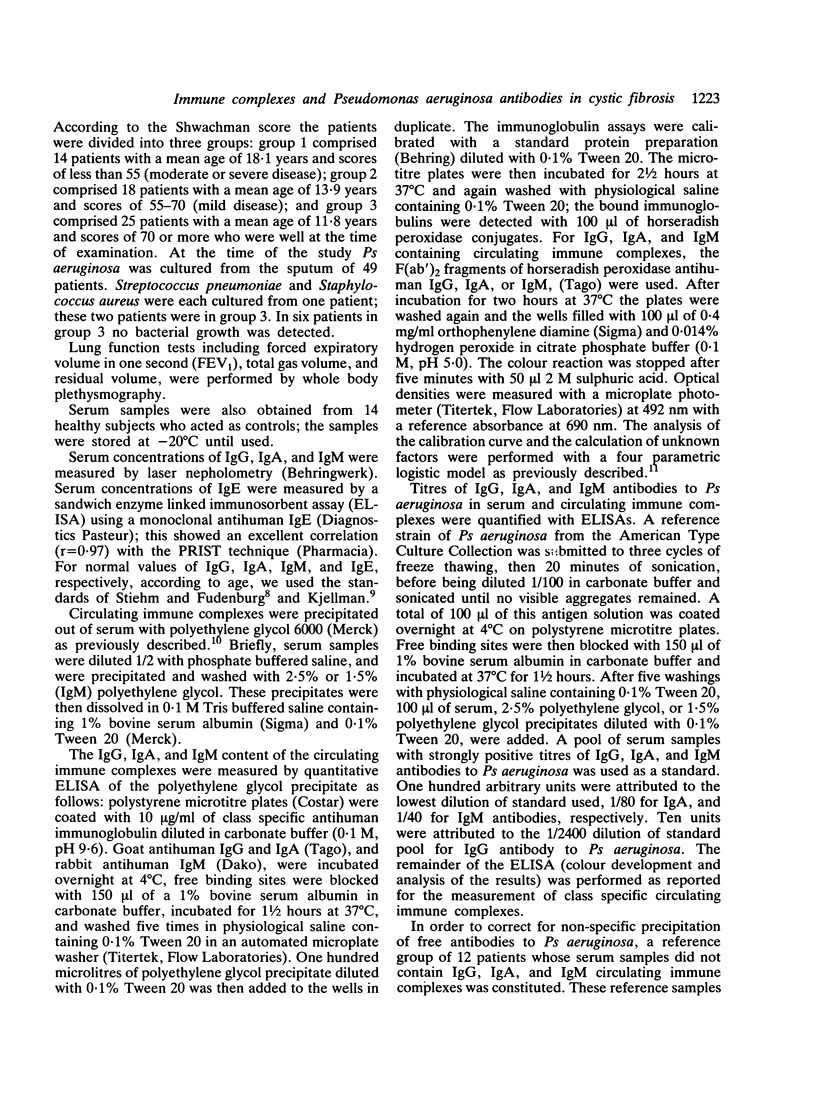
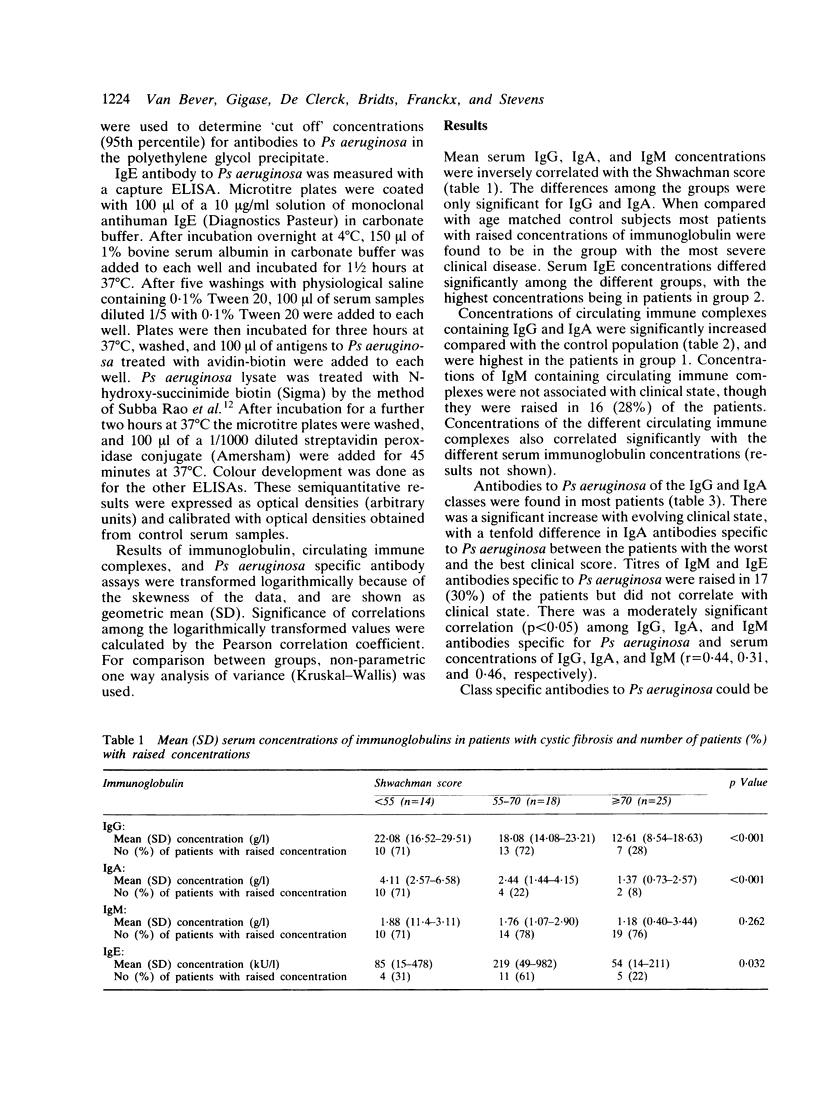
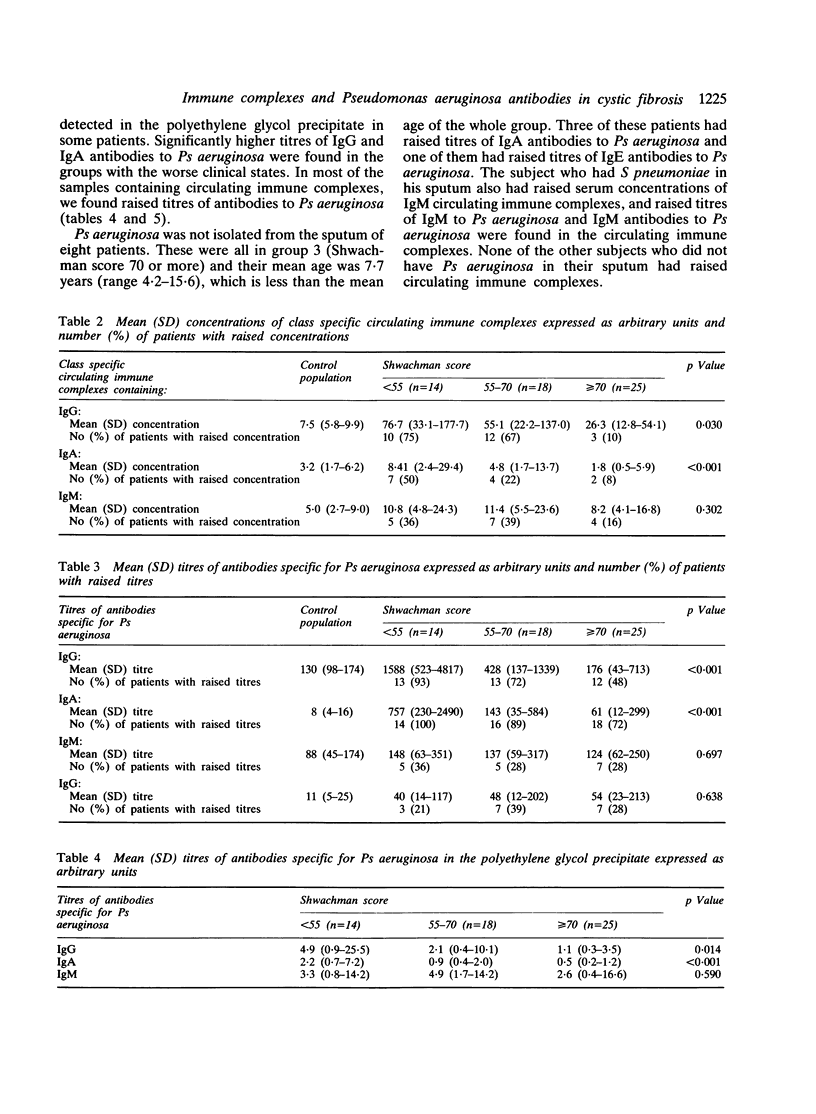
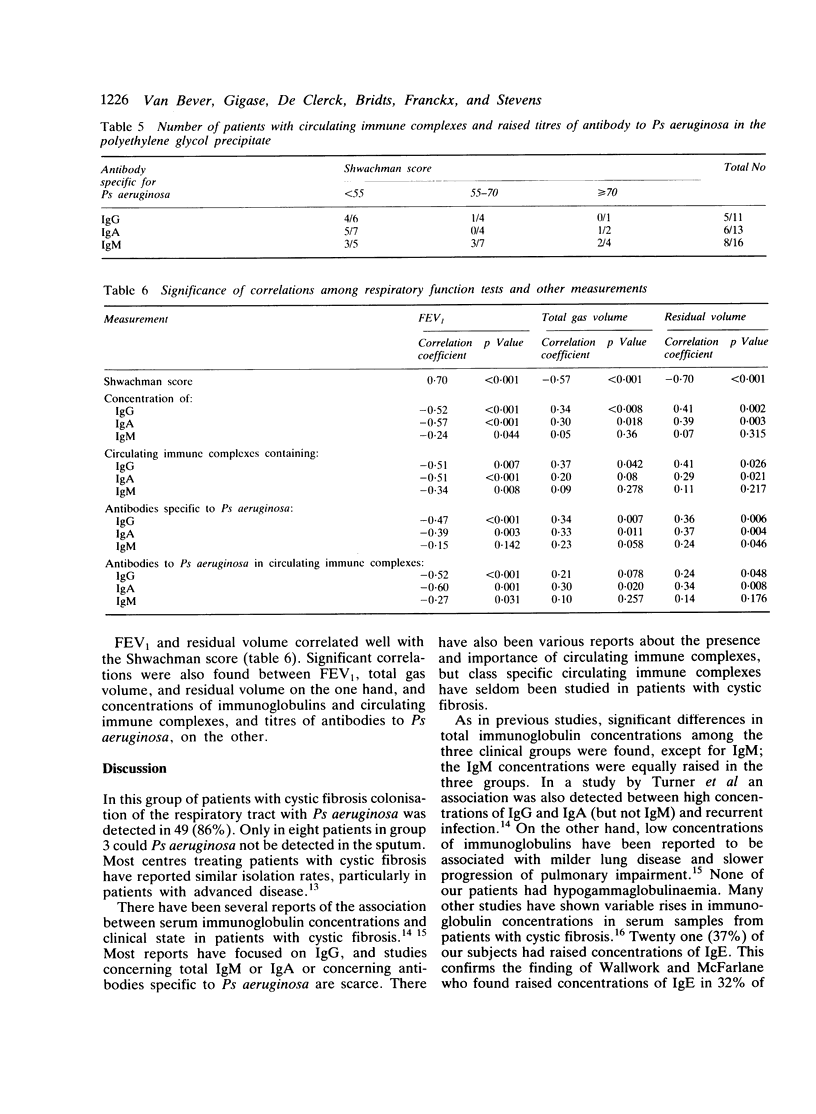
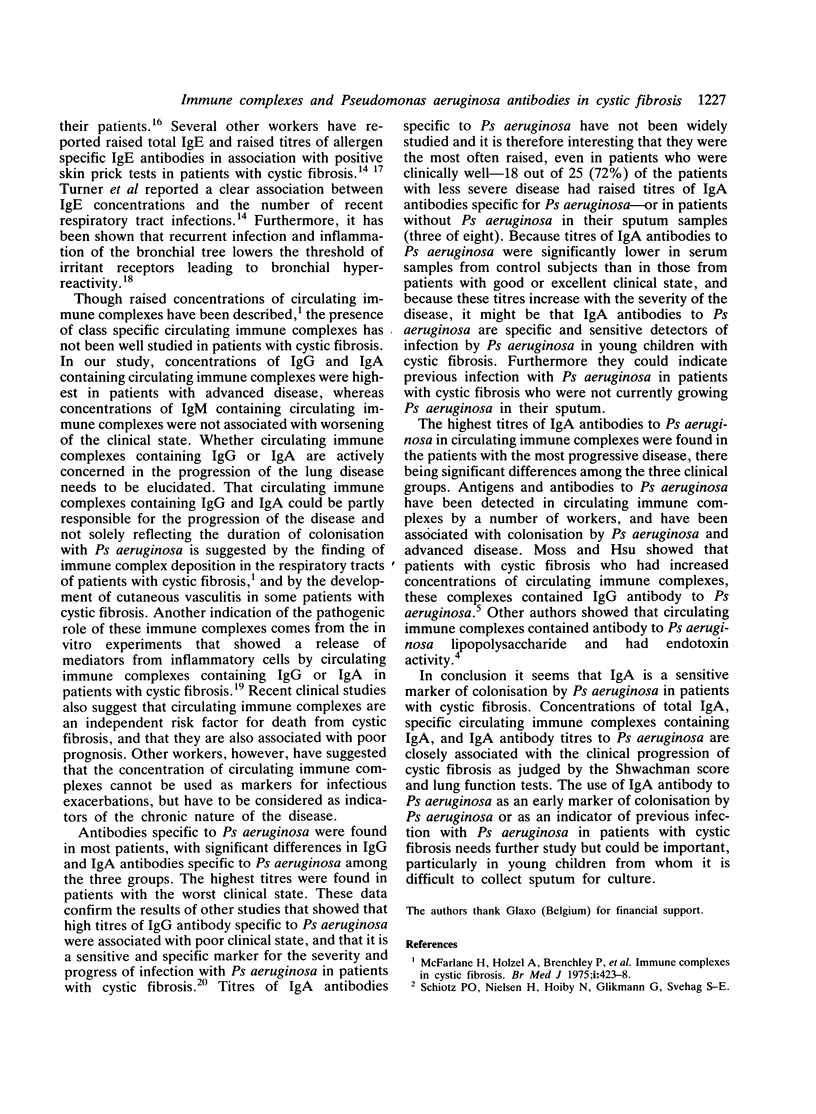
Serum samples from 57 patients with cystic fibrosis were tested for the presence of IgG, IgA, IgM, IgE, and circulating immune complexes containing IgG, IgA, and IgM. Titres of class specific antibodies to Pseudomonas aeruginosa, and class specific antibodies to Ps aeruginosa in circulating immune complexes, were also measured. According to the Shwachman score the patients were divided into three clinical groups: group 1-moderate and severe disease, group 2-mild disease, and group 3-well. The results of the immunological investigations were correlated with the clinical state of the patients as assessed by the Shwachman score. Serum concentrations of IgG, IgA, and IgM were inversely correlated with the Shwachman score, but the differences between the groups were only significant for IgG and IgA. The same correlations were found for circulating immune complexes containing IgG and IgA. Antibodies to Ps aeruginosa could be detected in most of the patients' serum samples. IgA antibody specific to Ps aeruginosa was the most often raised, even in patients in group 3. It is therefore suggested that IgA antibody specific to Ps aeruginosa could be an early marker of colonisation by Ps aeruginosa and a sensitive measurement of infection with Ps aeruginosa in young children with cystic fibrosis. Moreover, in the circulating immune complexes, class specific antibodies to Ps aeruginosa were found in nearly half the patients. The highest titres of IgG and IgA antibodies specific to Ps aeruginosa in the circulating immune complexes were detected in the patients with the worst clinical state (group 1).
Full text
PDF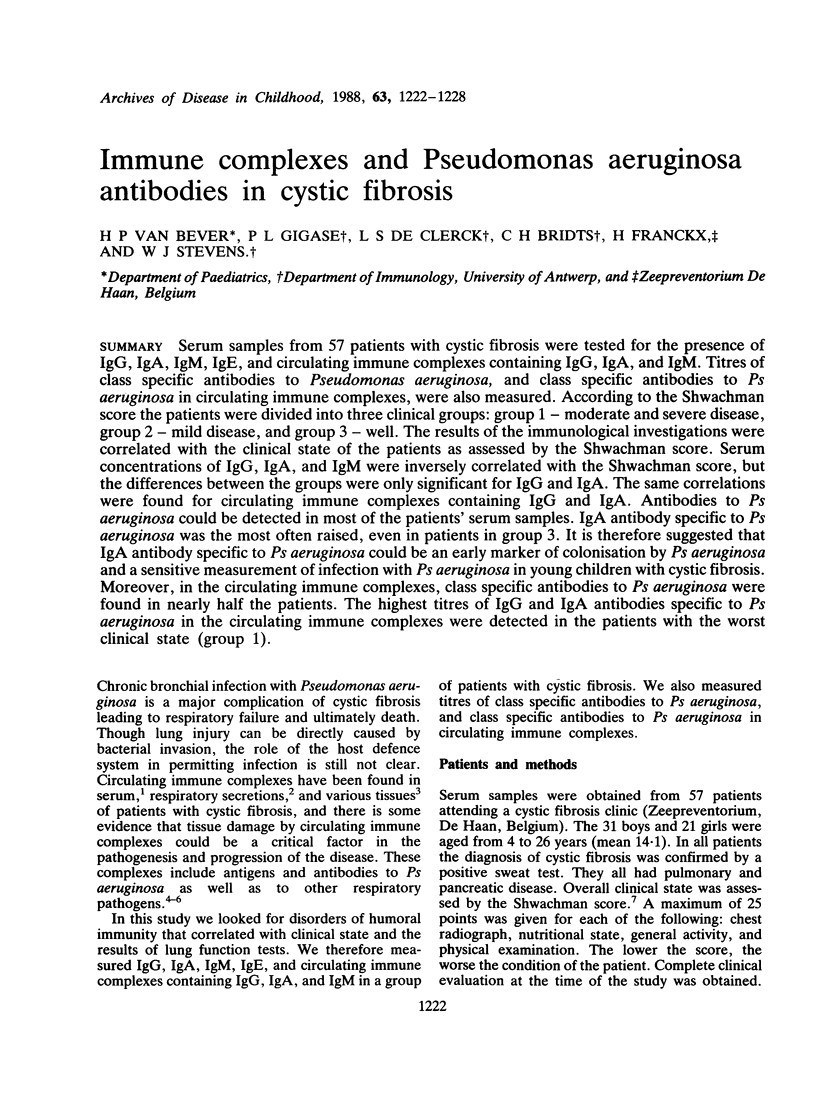

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allan J. D., Moss A. D., Wallwork J. C., McFarlane H. Immediate hypersensitivity in patients with cystic fibrosis. Clin Allergy. 1975 Sep;5(3):255–261. doi: 10.1111/j.1365-2222.1975.tb01860.x. [DOI] [PubMed] [Google Scholar]
- Berdischewsky M., Pollack M., Young L. S., Chia D., Osher A. B., Barnett E. V. Circulating immune complexes in cystic fibrosis. Pediatr Res. 1980 Jun;14(6):830–833. doi: 10.1203/00006450-198006000-00011. [DOI] [PubMed] [Google Scholar]
- Dasgupta M. K., Zuberbuhler P., Abbi A., Harley F. L., Brown N. E., Lam K., Dossetor J. B., Costerton J. W. Combined evaluation of circulating immune complexes and antibodies to Pseudomonas aeruginosa as an immunologic profile in relation to pulmonary function in cystic fibrosis. J Clin Immunol. 1987 Jan;7(1):51–58. doi: 10.1007/BF00915425. [DOI] [PubMed] [Google Scholar]
- Davis C. A., Abramowsky C. R., Swinehart G. Circulating immune complexes and the nephropathy of cystic fibrosis. Hum Pathol. 1984 Mar;15(3):244–247. doi: 10.1016/s0046-8177(84)80187-2. [DOI] [PubMed] [Google Scholar]
- Kjellman N. I. Predictive value of high IgE levels in children. Acta Paediatr Scand. 1976 Jul;65(4):465–471. doi: 10.1111/j.1651-2227.1976.tb04915.x. [DOI] [PubMed] [Google Scholar]
- McFarlane H., Holzel A., Brenchley P., Allan J. D., Wallwork J. C., Singer B. E., Worsley B. Immune complexes in cystic fibrosis. Br Med J. 1975 Feb 22;1(5955):423–428. doi: 10.1136/bmj.1.5955.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell I., Corey M., Woenne R., Krastins I. R., Levison H. Bronchial hyperreactivity in cystic fibrosis and asthma. J Pediatr. 1978 Nov;93(5):744–748. doi: 10.1016/s0022-3476(78)81070-1. [DOI] [PubMed] [Google Scholar]
- Moss R. B., Hsu Y. P. Isolation and characterization of circulating immune complexes in cystic fibrosis. Clin Exp Immunol. 1982 Feb;47(2):301–308. [PMC free article] [PubMed] [Google Scholar]
- Permin H., Skov P. S., Norn S., Høiby N., Schiøtz P. O. Platelet 3H-serotonin releasing immune complexes induced by Pseudomonas aeruginosa in cystic fibrosis. Allergy. 1982 Feb;37(2):93–100. doi: 10.1111/j.1398-9995.1982.tb01882.x. [DOI] [PubMed] [Google Scholar]
- Pitcher-Wilmott R. W., Levinsky R. J., Matthew D. J. Circulating soluble immune complexes containing pseudomonas antigens in cystic fibrosis. Arch Dis Child. 1982 Aug;57(8):577–581. doi: 10.1136/adc.57.8.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHWACHMAN H., KULCZYCKI L. L. Long-term study of one hundred five patients with cystic fibrosis; studies made over a five- to fourteen-year period. AMA J Dis Child. 1958 Jul;96(1):6–15. doi: 10.1001/archpedi.1958.02060060008002. [DOI] [PubMed] [Google Scholar]
- Stevens W. J., Bridts C. H. IgG-containing and IgE-containing circulating immune complexes in patients with asthma and rhinitis. J Allergy Clin Immunol. 1984 Feb;73(2):276–282. doi: 10.1016/s0091-6749(84)80020-2. [DOI] [PubMed] [Google Scholar]
- Stiehm E. R., Fudenberg H. H. Serum levels of immune globulins in health and disease: a survey. Pediatrics. 1966 May;37(5):715–727. [PubMed] [Google Scholar]
- Subba Rao P. V., McCartney-Francis N. L., Metcalfe D. D. An avidin--biotin microELISA for rapid measurement of total and allergen-specific human IgE. J Immunol Methods. 1983 Feb 25;57(1-3):71–85. doi: 10.1016/0022-1759(83)90066-2. [DOI] [PubMed] [Google Scholar]
- Turner M. W., Warner J. O., Stokes C. R. Immunological studies in cystic fibrosis. Arch Dis Child. 1978 Aug;53(8):631–638. doi: 10.1136/adc.53.8.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallwork J. C., McFarlane H. The SIgA system and hypersensitivity in patients with cystic fibrosis. Clin Allergy. 1976 Jul;6(4):349–358. doi: 10.1111/j.1365-2222.1976.tb01915.x. [DOI] [PubMed] [Google Scholar]
- Wheeler W. B., Williams M., Matthews W. J., Jr, Colten H. R. Progression of cystic fibrosis lung disease as a function of serum immunoglobulin G levels: a 5-year longitudinal study. J Pediatr. 1984 May;104(5):695–699. doi: 10.1016/s0022-3476(84)80946-4. [DOI] [PubMed] [Google Scholar]


