Abstract
Background. Congenital cytomegalovirus (CMV) infection is a leading cause of disabilities in children, yet the general public appears to have little awareness of CMV. Methods. Women were surveyed about newborn infections at 7 different geographic locations. Results. Of the 643 women surveyed, 142 (22%) had heard of congenital CMV. Awareness increased with increasing levels of education (P < .0001). Women who had worked as a healthcare professional had a higher prevalence of awareness of CMV than had other women (56% versus 16%, P < .0001). Women who were aware of CMV were most likely to have heard about it from a healthcare provider (54%), but most could not correctly identify modes of CMV transmission or prevention. Among common causes of birth defects and childhood illnesses, women's awareness of CMV ranked last. Conclusion. Despite its large public health burden, few women had heard of congenital CMV, and even fewer were aware of prevention strategies.
BACKGROUND
CMV is the most common congenital infection in the United States, affecting as many as 40 000 newborns each year [1]. Approximately, 10% of these infants are symptomatic at birth and most of these will suffer permanent neurologic sequelae such as neurodevelopmental delays, motor disabilities, deafness, and blindness [2–5]. Although most infants appear asymptomatic at birth, 10% to 15% of them will develop progressive hearing loss [6]. More children are affected by congenital CMV-related disabilities than by other, better-known childhood diseases, and syndromes, such as fetal alcohol syndrome, Down's syndrome, and neural tube defects [2, 7].
Most congenital CMV infections and related disabilities result from primary (ie, first-time) infections in pregnant women [8]. Many maternal CMV infections might be prevented by simple hygienic precautions, such as frequent and thorough hand washing [7, 9]. Despite this opportunity to prevent infection in mothers and subsequent disability in their children, anecdotal evidence suggests that the general public has little awareness or knowledge of CMV. To further investigate this evidence, and to improve the knowledge base for developing effective interventions, we designed a survey to evaluate awareness and knowledge of CMV among women.
METHODS
We conducted a survey of congenital CMV awareness at 7 different geographic locations: Atlanta, GA; Birmingham, AL; Cleveland, OH; Provo, UT; Richmond, VA; Chicago, IL; and Houston, TX. At the first four sites, women were recruited from pediatric outpatient clinic waiting rooms. In Richmond, women were recruited from an obstetrics/gynecology clinic. In Chicago, women were recruited from a university's student union center. In Houston, the women who participated in the survey were medical students and support staff in a hospital. At each site, we asked all women aged ≥ 18 years, who were literate in English or Spanish, to complete the short, self-administered written survey. Women were told that the survey would assess their knowledge of newborn infections but not that it was designed specifically to assess knowledge of congenital CMV. The survey assessed demographic information, awareness of CMV, risk factors, modes of transmission, prevention of CMV infection, and symptoms of CMV disease. The survey also collected information about healthcare and prenatal visits, parenting behaviors, and awareness of other birth defects and childhood illnesses. When the women returned their completed surveys, they were given a brochure about congenital CMV. The study was approved by the human subjects review boards of the institutions involved.
RESULTS
CMV awareness
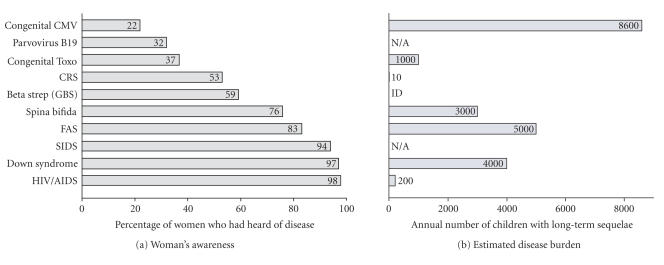
We aimed to survey approximately 100 women at each of the study sites (Table 1). Of the 643 women surveyed, 142 (22%) had heard of congenital CMV. Among other birth defects and childhood illnesses that were included in the survey, women's awareness of congenital CMV ranked last (Figure 1(a)).
Table 1.
Awareness of congenital CMV by characteristics of women. Note that not all questions had responses from all participants.
| Characteristic | Aware of CMV | Unaware of CMV | Odds ratio | 95% CI (a) | P-value (b) | ||
| n = 142 | Percentage | n = 497 | Percentage | ||||
|
| |||||||
| Site | |||||||
| Chicago, IL (reference) | 8 | 7 | 100 | 93 | 1 | ||
| Provo, UT | 5 | 12 | 38 | 88 | 1.6 | (0.5–5.3) | .41 |
| Richmond, VA | 16 | 18 | 73 | 82 | 2.7 | (1.1–6.7) | .02 |
| Cleveland, OH | 21 | 21 | 79 | 79 | 3.3 | (1.4–7.9) | .005 |
| Atlanta, GA | 28 | 26 | 81 | 74 | 4.3 | (1.9–10.0) | .0003 |
| Birmingham, AL | 26 | 30 | 62 | 70 | 5.2 | (2.2–12.3) | < .0001 |
| Houston, TX | 38 | 37 | 64 | 63 | 7.4 | (3.3–16.9) | < .0001 |
| Race | |||||||
| Whites (reference) | 82 | 23 | 278 | 77 | 1 | ||
| Blacks | 39 | 22 | 137 | 78 | 1.0 | (0.6–1.5) | .87 |
| Hispanics | 12 | 24 | 37 | 76 | 1.1 | (0.6–2.2) | .79 |
| Asians | 6 | 16 | 31 | 84 | 0.7 | (0.3–1.6) | .36 |
| Other | 3 | 19 | 13 | 81 | 0.8 | (0.2–2.8) | .71 |
| Age | |||||||
| Under 20 (reference) | 4 | 15 | 22 | 85 | 1 | .02 | |
| 20–29 | 64 | 21 | 245 | 79 | 1.4 | (0.5–4.3) | |
| 30–39 | 41 | 22 | 147 | 78 | 1.5 | (0.5–4.7) | |
| 40–49 | 25 | 27 | 69 | 73 | 2.0 | (0.6–6.4) | |
| Over 49 | 8 | 47 | 9 | 53 | 4.9 | (1.2–20.4) | |
| Level of education | |||||||
| Less than high school (reference) | 1 | 4 | 24 | 96 | 1 | < .0001 | |
| High-school diploma or GED | 33 | 17 | 166 | 83 | 4.8 | (0.6–36.5) | |
| Some college | 43 | 21 | 158 | 79 | 6.5 | (0.9–49.7) | |
| bachelor's degree or more | 65 | 31 | 145 | 69 | 10.8 | (1.4–81.2) | |
| Level of income | |||||||
| Less than $20 000 (reference) | 28 | 24 | 91 | 76 | 1 | .62 | |
| $20 000–49 999 | 42 | 24 | 131 | 76 | 1.0 | (0.6–1.8) | |
| $50 000–74 999 | 25 | 21 | 94 | 79 | 0.9 | (0.5–1.6) | |
| $75 000–100 000 | 21 | 25 | 62 | 75 | 1.1 | (0.6–2.1) | |
| More than $100 000 | 23 | 21 | 89 | 79 | 0.8 | (0.5–1.6) | |
| Ever worked as a healthcare professional | |||||||
| No (reference) | 83 | 16 | 443 | 84 | 1 | < .0001 | |
| Yes | 58 | 56 | 46 | 44 | 6.7 | (4.3–10.6) | |
| Ever worked as a daycare worker | |||||||
| No (reference) | 108 | 21 | 405 | 79 | 1 | .18 | |
| Yes | 32 | 27 | 88 | 73 | 1.4 | (0.9–2.2) | |
| Location where healthcare received | |||||||
| private doctor or HMO (reference) | 89 | 22 | 310 | 78 | 1 | .81 | |
| Other | 53 | 23 | 176 | 77 | 1.1 | (0.7–1.5) | |
| Ever been pregnant | |||||||
| No (reference) | 39 | 19 | 166 | 81 | 1 | .15 | |
| Yes | 103 | 24 | 321 | 76 | 1.4 | (0.9–2.1) | |
(a)CI: confidence interval.
(b) P-value of association or trend.
Figure 1.
(a) Awareness of congenital CMV and other birth defects and childhood illnesses. (b) Estimates of the annual burden of prominent childhood diseases and syndromes in the US (from [7]). Assumes 4 million live births per year and 20 million children <5 years of age. Childhood deaths were defined as those occurring <1 year after birth except for Haemophilus influenzae type B (Hib) (<5 years) and HIV/AIDS (<13 years). Where applicable, numbers represent means of published estimates. All estimates should be considered useful for rough comparisons only since surveillance methodology and diagnostic accuracy varied over different studies. CMV: cytomegalovirus; Toxo: toxoplasmosis; CRS: congenital rubella syndrome; GBS: group B strep; FAS: fetal alcohol syndrome; SIDS: sudden infant death syndrome; N/A: not applicable because long-term sequelae are not normally associated with the condition; ID: insufficient data.
In univariate analyses, awareness of CMV increased with higher levels of education (P-value for trend < .0001), older age (P-value for trend = .02), and varied by study site, with awareness being highest in Houston and Birmingham and lowest in Chicago (Table 1). In addition, women who were currently or previously employed in healthcare professions were more likely to have heard of CMV than those who had never worked in the health field (56% versus 16%, OR = 6.7 [4.3−10.6]). On the other hand, there was no significant difference in awareness of CMV between women who were currently or previously employed as a daycare worker. There was also no significant difference in CMV awareness between women who had never been pregnant and women who had been pregnant. There were no significant differences in awareness of CMV by income or race/ethnicity. After adjusting for other covariates in multivariate analyses, awareness was still associated with higher level of education and having been a healthcare professional, but was no longer associated with older age (Table 2).
Table 2.
Logistic regression summary: awareness of congenital CMV among women. Some categories were collapsed in the multivariate analysis because of small numbers in the categories.
| Characteristic | Odds ratio | 95% CI (a) | P-value (b) |
|
| |||
| Site | |||
| Chicago, IL (reference) | 1 | — | .58 |
| Provo, UT | 1.4 | (0.3–6.7) | |
| Richmond, VA | 4.6 | (1.2–16.7) | |
| Cleveland, OH | 2.3 | (0.6–8.2) | |
| Atlanta, GA | 4.4 | (1.3–15.6) | |
| Birmingham, AL | 7.6 | (1.9–30.6) | |
| Houston, TX | 5.3 | (1.8–15.8) | |
| Race | |||
| Whites (reference) | 1 | — | .66 |
| Blacks | 0.8 | (0.4–1.5) | |
| Hispanics | 0.9 | (0.4–2.1) | |
| Other | 1.1 | (0.4–2.9) | |
| Age | |||
| Under 30 (reference) | 1 | — | .90 |
| 30–39 | 0.6 | (0.3-1.0) | |
| 40 and over | 1.0 | (0.5–1.9) | |
| Level of education | |||
| High-school diploma or less | 1 | — | .03 |
| Some college | 1.5 | (0.8–2.7) | |
| bachelor's degree or more | 2.1 | (1.1–4.1) | |
| Level of income | |||
| less than $20 000 (reference) | 1 | — | .82 |
| $20 000–49 999 | 1.1 | (0.6–2.1) | |
| $50 000–74 999 | 0.9 | (0.4–1.9) | |
| $75 000–100 000 | 1.3 | (0.5–3.0) | |
| More than $100 000 | 0.9 | (0.4–2.1) | |
| Ever worked as a healthcare professional | |||
| No (reference) | 1 | — | < .0001 |
| Yes | 6.8 | (3.9–11.7) | |
| Ever worked as a daycare worker | |||
| No (reference) | 1 | — | .99 |
| Yes | 0.9 | (0.5–1.6) | |
| Location where healthcare received | |||
| private doctor or HMO (reference) | 1 | — | .97 |
| Other | 1.0 | (0.6–1.7) | |
| Ever been pregnant | |||
| No (reference) | 1 | — | .39 |
| Yes | 1.2 | (0.5–2.5) | |
(a) CI: confidence interval.
(b) P-value of association or trend.
CMV knowledge among women who had heard of CMV
Among the 142 (22%) women who had heard of CMV, there was a low level of accurate knowledge about CMV. The majority of these respondents could not correctly identify the symptoms associated with congenital CMV disease (Table 3). Approximately, one third (36%, 48/133) also indicated that congenital CMV could cause congenital heart defect, a symptom not associated with congenital CMV.
Table 3.
Percentage of women responding to questions regarding which of the following clinical manifestations were caused by congenital CMV in newborns. Note that these figures are among the 22% of the women who have heard of CMV.
| Congenital CMV in newborns can cause | Yes (%) | No (%) | Do not know (%) |
|
| |||
| Hearing loss | 48* | 8 | 44 |
| Mental retardation | 47* | 5 | 48 |
| Jaundice | 24* | 13 | 63 |
| Seizures | 34* | 6 | 60 |
| Microcephaly | 30* | 8 | 63 |
| Death | 35* | 7 | 58 |
| Club foot | 8 | 21* | 71 |
| Congenital heart defect | 36 | 7* | 57 |
*Correct answers.
Although women who had heard of CMV appeared to lack knowledge about CMV and its symptoms, most women indicated (78%, 109/140) that a pregnant woman could pass CMV to her unborn baby. More than half (57%, 78/138) indicated that the spread of CMV could be reduced by frequent hand washing. However, nearly one quarter (23%, 83/137) incorrectly believed that CMV could be prevented by avoiding cleaning cat litter boxes. Concerning source of knowledge, 54% of women indicated that they had heard about congenital CMV from a healthcare professional (Table 4).
Table 4.
Source of CMV awareness or knowledge. Note that multiple answers were accepted so the percentages add to more than 100%.
| Source | Number | Percentage |
|
| ||
| Healthcare provider | 79 | 54 |
| School or class | 46 | 32 |
| Magazine, book, or newspaper | 23 | 16 |
| Family or friends | 17 | 12 |
| Other | 14 | 10 |
| Internet | 7 | 5 |
| Radio or TV | 5 | 3 |
DISCUSSION
To our knowledge, this was the first survey to examine women's knowledge of congenital CMV. Of the women surveyed, only 22% had heard of congenital CMV and very few had specific knowledge about clinical symptoms, modes of transmission, or prevention. There was a tremendous gap between CMV knowledge and congenital CMV disease burden (Figure 1)—women's awareness of CMV ranked last among other birth defects and common childhood illnesses despite CMV being one of the most common and most serious causes of birth defects and disabilities [7].
In order to bridge this gap, women should be educated about congenital CMV. Our survey indicated that healthcare professionals play the most important role in informing women about CMV (Table 4). Yet, only a little over half of women who were working or had worked in the healthcare field were aware of congenital CMV. Women did not specify what type of healthcare work they had done, and many might have done work that required no CMV-related knowledge or training. Nevertheless, the lack of awareness among healthcare professionals shows that there is considerable room for improvement. The curricula of medical, nursing, and midwifery schools should emphasize the importance of educating pregnant women about congenital CMV prevention through improved hand hygiene, as recommended by the American College of Obstetrics and Gynecology (ACOG) [10]. Surveys should be conducted of healthcare providers' knowledge and practices relating to congenital CMV, including how well providers adhere to these ACOG recommendations.
The survey revealed that women who were currently working or had worked in daycare centers were no more aware of congenital CMV than those who had never worked in a daycare setting. Prevalence of CMV in daycare centers is relatively high due to horizontal spread [11], and women who work with children in this setting have a higher risk of acquiring CMV infection. Day care workers should be informed of the risk of acquiring CMV infection and possible effects on the unborn child, as well as strategies for reducing risk of infection.
Many women also indicated that they were informed about CMV through school or class. Information about CMV should be included in secondary-school health curricula and in childbirth courses for expecting parents. Although educational messages need to target all women, a special effort should be made to reach women of lower educational levels, since their awareness was the lowest.
It is important that books and magazines—another key source of CMV information identified by our survey—contain better CMV information than is currently available. Many pregnancy books contain little information on CMV, and sometimes their information is inaccurate. For example, although studies show relatively high rates of transmission from young children to parents [12], one popular pregnancy book states that “Pregnant women with toddlers of their own need not worry about catching CMV; the possibility is extremely remote.” Such inaccuracies might be reduced by consulting physicians who are experts on congenital CMV infection, or by including information from other reliable sources, such as ACOG [10] or the Centers for Disease Control and Prevention (CDC).
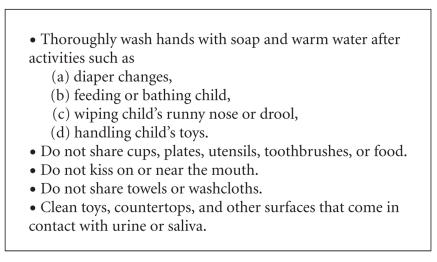
The CMV prevention guidelines that pregnant women should receive from healthcare providers, books, magazines, websites, and other media should be straightforward and have a special focus on improved hand hygiene (Figure 2) [7]. Examples of these guidelines can be found at websites such as http://www.cdc.gov/cmv and http://www.bcm.edu/pedi/infect/cmv. Risk of CMV infection is likely to be reduced by adherence to these guidelines [7], and pregnant women have proven receptive to other behavior changes that protect their babies [9, 13–19]. In our survey, for example, nearly all women reported that during their latest pregnancy, they took prenatal vitamins on a regular basis (90%) and did not drink alcohol (94%). Further research is needed to assess which prevention messages work best for CMV and which educational interventions are most effective.
Figure 2.
Hygienic practices to reduce risk of CMV infection for women who are pregnant or planning to become pregnant. When interacting with young children, women should assume the children are excreting CMV in their urine and saliva (from [7]).
Our survey was subject to several limitations. The questionnaire was not pretested to eliminate ambiguous questions, and some of the respondents did not follow directions when answering questions. Another limitation was that the survey was a convenience sample that may not represent all women in the US. This type of sampling led to significant variation in awareness at different sites. For example, the lower awareness in Chicago was probably due to the women being young, college students, whereas the higher awareness in Houston was probably due to the women being medical students and hospital support staff. Nevertheless, the seven different geographical locations included a diverse population of women, so the results should be reasonably applicable to women of childbearing age. Another study limitation was that guessing may have played a role in answering specific knowledge questions about CMV. For example, many women incorrectly answered that CMV can cause congenital heart defects. This implies that some women may have guessed correctly about other questions. Hence, our survey may overestimate women's knowledge about CMV. Selection bias may also have affected our results. The majority of the surveys were administered in a clinic setting, and women attending a healthcare clinic may be more likely to be aware of health issues than other women. Such bias may have led to overestimates of women's awareness of CMV.
Raising awareness among women and their healthcare providers will be an important first step for preventing congenital CMV. Such awareness can lead to improvement in hygiene behaviors among pregnant women, immediately impacting the congenital CMV disease burden. Furthermore, as women and their healthcare providers become educated about congenital CMV, they will better appreciate the potential for interventions such as prenatal screening and diagnosis [20], newborn screening [21], and antiviral [22] or hyperimmuneglobulin treatments [23], and they will see the urgent need for the development of an effective CMV vaccine [24].
ACKNOWLEDGMENTS
This survey would not have been possible without the support and contributions of many people. We thank Ardyth Cannon for her enthusiasm and for assistance with collection in Provo, UT, and also thank Jessica Blackham at Keith J. Clayton Pediatrics and Casey Galt at Utah Valley Pediatrics. We also thank Dr Ray Rosenberg of Northlake Pediatric Associates and Dr Athanasios Verras of Northlake Parkway and their staff for support in Atlanta, GA. In Birmingham, we would like to thank Drs Carolyn Ashworth and Cason Benton and the staff of the UAB Primary Care Clinic. At the Children's Hospital Cleveland Clinic in Cleveland, Ohio, we thank Uzma Siddiqui. From Baylor College of Medicine, we thank Carol Griesser, RN, who participated in recruitment of subjects, database management, filing, mailings, communications, and contributed greatly to the success in Houston. We also thank Brittany Ruddell for her assistance. In Virginia, sincere thanks go to Anne-Marie Manganello. This study was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention, administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the US Department of Energy and the CDC.
References
- 1.Gaytant MA, Steegers EAP, Semmekrot BA, Merkus HMMW, Galama JMD. Congenital cytomegalovirus infection: review of the epidemiology and outcome. Obstetrical and Gynecological Survey. 2002;57(4):245–256. doi: 10.1097/00006254-200204000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Dobbins JG, Stewart JA, Demmler G. Surveillance of congenital cytomegalovirus disease, 1990-1991. Collaborating Registry Group. Morbidity and Mortality Weekly Report. CDC Surveillance Summaries. 1992;41(2):35–39. [PubMed] [Google Scholar]
- 3.Boppana SB, Fowler K, Britt WJ, Stagno S, Pass RF. Symptomatic congenital cytomegalovirus infection in infants born to mothers with preexisting immunity to cytomegalovirus. Pediatrics. 1999;104(1, part 1):55–60. doi: 10.1542/peds.104.1.55. [DOI] [PubMed] [Google Scholar]
- 4.Fowler K, Stagno S, Pass RF, Britt WJ, Boll TJ, Alford CA. The outcome of congenital cytomegalovirus infection in relation to maternal antibody status. New England Journal of Medicine. 1992;326(10):663–667. doi: 10.1056/NEJM199203053261003. [DOI] [PubMed] [Google Scholar]
- 5.Demmler G. Infectious Diseases Society of America and Centers for Disease Control: summary of a workshop on surveillance for congenital cytomegalovirus disease. Reviews of Infectious Diseases. 1991;13(2):315–329. doi: 10.1093/clinids/13.2.315. [DOI] [PubMed] [Google Scholar]
- 6.Stagno S, Whitley RJ. Herpesvirus infections of pregnancy. Part II. Herpes simplex virus and varicella-zoster virus infections. New England Journal of Medicine. 1985;313(21):1327–1330. doi: 10.1056/NEJM198511213132105. [DOI] [PubMed] [Google Scholar]
- 7.Cannon MJ, Davis KF. Washing our hands of the congenital cytomegalovirus disease epidemic. BMC Public Health. 2005;5:70. doi: 10.1186/1471-2458-5-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stagno S, Pass RF, Cloud G, et al. Primary cytomegalovirus infection in pregnancy. Incidence, transmission to fetus, and clinical outcome. Journal of the American Medical Association. 1986;256(14):1904–1908. [PubMed] [Google Scholar]
- 9.Adler SP, Finney JW, Manganello AM, Best ALM. Prevention of child-to-mother transmission of cytomegalovirus by changing behaviors: a randomized controlled trial. Pediatric Infectious Disease Journal. 1996;15(3):240–246. doi: 10.1097/00006454-199603000-00013. [DOI] [PubMed] [Google Scholar]
- 10.ACOG practice bulletin. Perinatal viral and parasitic infections. Number 20, September 2000. (Replaces educational bulletin number 177, February 1993). American College of Obstetrics and Gynecologists. International Journal of Gynaecology and Obstetrics. 2002;76(1):95–107. [PubMed] [Google Scholar]
- 11.Pass RF, August AM, Dworsky M, Reynolds DW. Cytomegalovirus infection in a day-care center. New England Journal of Medicine. 1982;307(8):477–479. doi: 10.1056/NEJM198208193070804. [DOI] [PubMed] [Google Scholar]
- 12.Pass RF, Hutto C, Ricks R, Cloud GA. Increased rate of cytomegalovirus infection among parents of children attending day-care centers. New England Journal of Medicine. 1986;314(22):1414–1418. doi: 10.1056/NEJM198605293142204. [DOI] [PubMed] [Google Scholar]
- 13.Chang G, Wilkins-Haug L, Berman S, Goetz MA. Brief intervention for alcohol use in pregnancy: a randomized trial. Addiction. 1999;94(10):1499–1508. doi: 10.1046/j.1360-0443.1999.941014996.x. [DOI] [PubMed] [Google Scholar]
- 14.Carter AO, Gelmon SB, Wells GA, Toepell AP. The effectiveness of a prenatal education programme for the prevention of congenital toxoplasmosis. Epidemiology and Infection. 1989;103(3):539–545. doi: 10.1017/s0950268800030934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pawlowski ZS, Gromadecka-Sutkiewicz M, Skommer J, et al. Impact of health education on knowledge and prevention behavior for congenital toxoplasmosis: the experience in Poznań, Poland. Health Education Research. 2001;16(4):493–502. doi: 10.1093/her/16.4.493. [DOI] [PubMed] [Google Scholar]
- 16.Chang G, Goetz MA, Wilkins-Haug L, Berman S. A brief intervention for prenatal alcohol use. An in-depth look. Journal of Substance Abuse Treatment. 2000;18(4):365–369. doi: 10.1016/s0740-5472(99)00105-1. [DOI] [PubMed] [Google Scholar]
- 17.Hankin JR. Fetal alcohol syndrome prevention research. Alcohol Research and Health. 2002;26(1):58–65. [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC). Spina bifida and anencephaly before and after folic acid mandate - United States, 1995-1996 and 1999-2000. Morbidity and Mortality Weekly Report. 2004;53(17):362–365. [PubMed] [Google Scholar]
- 19.Adler SP, Finney JW, Manganello AM, Best AM. Prevention of child-to-mother transmission of cytomegalovirus among pregnant women. Journal of Pediatrics. 2004;145(4):485–491. doi: 10.1016/j.jpeds.2004.05.041. [DOI] [PubMed] [Google Scholar]
- 20.Revello MG, Gerna G. Diagnosis and management of human cytomegalovirus infection in the mother, fetus, and newborn infant. Clinical Microbiology Reviews. 2002;15(4):680–715. doi: 10.1128/CMR.15.4.680-715.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bailey DB., Jr Newborn Screening for Fragile X Syndrome. Mental Retardation and Developmental Disabilities Research Reviews. 2004;10(1):3–10. doi: 10.1002/mrdd.20002. [DOI] [PubMed] [Google Scholar]
- 22.Maine GT, Lazzarotto T, Landini M-P. New developments in the diagnosis of maternal and congenital CMV infection. Expert Review of Molecular Diagnostics. 2001;1(1):19–29. doi: 10.1586/14737159.1.1.19. [DOI] [PubMed] [Google Scholar]
- 23.Nigro G, Adler SP, La Torre R. Passive immunization during pregnancy for congenital cytomegalovirus infection. New England Journal of Medicine. 2005;353(13):1350–1362. doi: 10.1056/NEJMoa043337. [DOI] [PubMed] [Google Scholar]
- 24.Arvin AM, Fast P, Myers M, Plotkin S, Rabinovich R, National Vaccine Advisory Committee Vaccine development to prevent cytomegalovirus disease: report from the National Vaccine Advisory Committee. Clinical Infectious Diseases. 2004;39(2):233–239. doi: 10.1086/421999. [DOI] [PubMed] [Google Scholar]