Abstract
Problem A Scottish national health service ophthalmic facility was unable to cope with increasing demand for cataract surgery.
Design Multifaceted approach to redesign hospital space to accommodate a cataract unit; to invest in cataract nursing staff to allow more operations under local anaesthesia and as day cases; and to enhance input by general practitioners and optometrists to streamline and reduce false positive cataract referrals. A prospective audit for productivity was undertaken in 2004 (two years after the redesign) and compared against the national cataract surgery audit data for Fife from 1997.
Setting District general hospital serving a population of 400 000 in south east Scotland.
Key measures for improvement Increasing throughput of cataract surgery while assessing quality of care provided against predefined evidence and Royal College of Ophthalmologists' guidelines, and evaluating training standards for ophthalmic surgical trainees against higher surgical training requirements.
Strategies for change Cataract services were redesigned to increase throughput and to reduce waiting times while preserving the quality of patient care. A secondary end point was to maintain surgical case load mix thus allowing trainees to continue to fulfil the number of operations required to acquire higher surgical training standards.
Effects of change In the same three month period 237 cataract operations were carried out in 1997 and 374 in 2004, representing an increase of productivity by 60%. The waiting time for surgery decreased from more than one year to three months. The redesign resulted in almost complete preoperative and postoperative assessment by nursing staff, thus freeing medical time and allowing for more operations. Optometrists' referrals with reports increased significantly (P<0.0001). The number of operations carried out as day cases under local anaesthesia increased, with fewer intraoperative complications and postoperative visits (P<0.0001). The number of operations carried out by trainees more than doubled, from 43 to 100 cases, thus improving training opportunities.
Lessons learnt Modest capital investment in rebuilding space and in staff for cataract services can improve the quality and volume of cataract surgery. Enhancing existing NHS services provides for future need while maintaining training standards, thus potentially obviating the need for independent treatment centres. This model could be used throughout the United Kingdom.
Context
The significant improvement in quality of life measures in elderly people after cataract surgery is undisputed worldwide.1 2 3 Cataract is a common cause of visual impairment, and cataract surgery is the most common elective surgical procedure carried out in the United Kingdom.4 Thirty per cent of those aged 65 in the United Kingdom have visually impairing cataract.5 Visual impairment is nationally defined as a best visual acuity of less than 6/12, below the criterion required for driving.5
Improving the quantity and quality of care for cataract surgery is currently a major focus for UK government policy for ophthalmic services. As life expectancy increases so will the demand for cataract surgery. The extent of this unmet need was highlighted by an epidemiological survey in 2000, which provided estimates of the shortfall by using holistic modelling.6 At that time the elderly population in the United Kingdom were often waiting for more than one year for cataract surgery.6 7 International studies suggest that not only do patients lose further visual acuity while on a waiting list but that this wait has important effects on rehabilitation and life expectancy.8
In 2000 the UK Department of Health produced a white paper titled “Action on cataracts,” giving guidance on the reorganisation of cataract services.9 This encouraged trust managers and ophthalmic consultants of the United Kingdom's national health service to investigate methods of reorganising their service to achieve the targets set by the government. The key end point was that by 2003 patients with cataract were to be treated within six months of referral. To achieve this, the projected increase in productivity was 43%. Consultants had the continued responsibility of maintaining quality of care and protecting training opportunities while increasing throughput.
The difficulty with keeping up with demand within the NHS led to the opening of independent sector treatment centres in England, with cataract surgery being the most common operation carried out by them.10 Although the centres contributed to reduced waiting time concerns remained about the absence of data on quality, continuity of care, and management of postoperative complications.11 Concerns were also expressed, that the centres have detracted from NHS investment to develop long term services for patients.12 13 Finally the centres may also result in dramatic reductions in training opportunities in certain districts.10
Background
The Queen Margaret Hospital in Fife serves a population of 400 000 and carries out all cataract surgery for the region. The staff component in 1997 consisted of four consultants, two specialist registrars, three senior house officers, and four cataract nurses. The four consultants were responsible for specialist services that included glaucoma, diabetes, paediatrics, and oculoplastics. In 1997 the hospital took part in a prospective three month national survey of cataract surgery carried out by the Royal College of Ophthalmologists.14 15 The individual results for the hospital were comparable to those of the survey. In the survey 86% of cataract surgery was carried out under local anaesthesia compared with 87% in the hospital. Seventy seven per cent of patients in the survey had phacoemulsification cataract surgery compared with 67% in the hospital. At final postoperative outcome 86% of patients in the survey achieved a visual acuity of 6/12 or better compared with 89% in the hospital. Listing practices were comparable, with 69% of patients in the survey having a preoperative vision worse than 6/12 compared with 65% in the hospital. We therefore knew that we were in line with national practice and not functioning suboptimally compared with other units. We also had no reason to believe that our patient population was anything other than a standard one.
Outline of problem
The Queen Margaret Hospital was beginning to experience the national trend of greater demand for cataract surgery from an ageing population.16 As with other national centres the waiting time for cataract surgery was more than a year. As a result the quality of care delivered to patients was affected. The long wait resulted in over 20% of patients having vision of counting fingers in the cataractous eye on the day of surgery. The long wait also resulted in changes in the patient's general health, thus resulting in more preoperative visits for repeated assessment. Although we made no formal assessment, we were aware that patients had important problems with transport for multiple hospital visits while dealing with the effects of major visual impairment during the wait for cataract surgery.
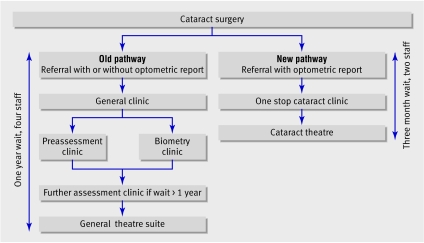
Trust management acknowledged that the unit was functioning at maximum capacity, given the limitations of space and medical and nursing time as well as the patients' circuitous journey through various departments of the hospital. At this time patients were largely assessed before and after surgery by doctors. The patients' journey for cataract surgery was initially through general outpatients, where they had their first consultation with the ophthalmologist, then day case assessment areas and biometry clinics, where they had their second or third consultation with either a doctor or a nurse, and finally the general theatre suite.,Patients could have between two and four hospital appointments, depending on the length of wait for cataract surgery.
Redesign and strategies for change
In 1997, 863 cataract operations were carried out at the Queen Margaret Hospital. Population estimates suggested that 1280 cataract operations were required per annum in a population of 400 000 for visually impairing cataract (best visual acuity worse than 6/12).16 This implied that the hospital had to increase its throughput by at least 50%. To tackle this problem a multidisciplinary team was set up, consisting of the unit's consultant ophthalmologists, senior cataract nursing staff, and the trust's business manager. This team was in continuous communication with lead members of the local general practitioner and optometry committees.
One stop cataract clinics
We decided to pilot the feasibility of one stop cataract clinics. A grant of £20 000 (€29 556; $38 851) was obtained from the Scottish Executive Office in 2000 to enable the pilot study to be carried out. These clinics were organised so that cataract nursing staff would initially assess patients and then the consultant would make a decision on the same day as to the necessity and suitability of the patients for day care surgery. This would reduce the number of preoperative assessments and waiting time for surgery. The initial experience and study in 2000 of 100 patients showed the clinics to be cost effective. The cost of a hospital appointment to the Queen Margaret Hospital in 2000 was estimated at £68; therefore the saving of even one extra hospital appointment per 100 patients resulted in a saving of £6800.17 From these clinics 85% of patients were listed for cataract surgery. The waiting time for patients to be seen at the clinic never exceeded 12 weeks. A patient satisfaction questionnaire showed that over 97% were extremely satisfied with the clinic's service.
Optometry and general practitioner support
Patients who attended the one stop cataract clinic would previously have been routed towards cataract surgery from general ophthalmic clinics. The waiting time for these clinic appointments varied from 6-12 months. Some priority was given to patients with profoundly reduced vision, but this was not consistent practice. Patients were referred to these clinics by their general practitioners, and inclusion of an optometry report was variable. An optometry report was invaluable as it informed the ophthalmologist of the best corrected visual acuity with updated refraction. This was crucial in the decision to operate. In addition the report gave important information on other ophthalmic disease that might have been contributing towards visual impairment. This would allow the patient to be appointed to the appropriate specialist ophthalmic clinic.
To reduce false positive referrals and streamline cataract referrals we decided on a strategy that only patients with optometrists' reports would be seen at the one stop cataract clinic. The local general practitioner and optometry committees were canvassed for their support with oral presentations and written information on the new clinic's service. Both parties were encouraged to send an optometrist's report with their cataract referrals.
Specialist cataract nurses
On the basis of our pilot data with the one stop clinic it was apparent that patients' care and throughput were also enhanced by continuity of nursing assessment for patients before and after surgery. For this reason we sought to deploy a fixed pool of nurses for this process.
Theatre journey
Despite all the advantages of the one stop clinic we recognised that the patient's journey on the day of surgery was suboptimal. A general theatre suite was being used and staffed by non-ophthalmic staff. This meant that the handing over and transfer procedure was an important limitation in patient turnover time between operations.
Redesign build
After the success of our one stop clinic the Scottish Executive Office granted the trust a one-off payment of £250 000, which was matched by the Fife NHS Trust. In December 2002 a rebuild at a cost of £500 000 (capital) was completed in a vacated area of the Queen Margaret Hospital. The new cataract unit had the feasibility for complete preoperative and postoperative assessment and surgery. Four extra cataract nursing staff, at a cost of £100 000 per annum, were also employed (recurrent trust annual expenditure). In addition a subsection of the general theatre suite nursing staff were appointed solely for ophthalmic surgery. Patient appointments were prioritised on the basis of degree of visual impairment. All patients with a vision of 6/60 or worse had surgery within 12 weeks of referral.
Data collection and statistics
The Queen Margaret Hospital took part in the data collected by the national cataract surgery survey in 1997, which involved 100 UK hospitals.14 15 The survey set predefined preoperative and postoperative data, which were collected prospectively by experienced senior cataract nursing staff at the Queen Margaret Hospital. Identical data were collected prospectively in 2004 using the same methodology as the national audit. The data were entered and analysed using Microsoft Office Excel and Microsoft Office Access. Statistical analysis was carried out using a two sample t test.
Effects of change
Process outcome
The table outlines the results from a prospective three month survey of consecutive cases of cataract surgery carried out in 1997 at the Queen Margaret Hospital and again in 2004 in the second year of the cataract unit. Overall, 863 cataract operations were carried out in 1997 compared with 1473 in 2004, representing an increase of 71%. Of the 15 Scottish health boards, Fife achieved the highest increase in rates of cataract surgery between 1997 and 2004.18 In 2004 there was significantly more optometric input into cataract referrals (P<0.0001). The number of operations carried out by trainees more than doubled between 1997 and 2004.
Results of three month audit of consecutive cases of cataract surgery carried out in 1997 at Queen Margaret Hospital, Fife, and in 2004 in the second year of the cataract unit. Values are numbers (percentages) unless stated otherwise
| Variables | 1997 | 2004 | P value |
|---|---|---|---|
| No of cataract operations | 237 | 374 | — |
| Retrieval rate | 222 (94) | 374(100) | |
| Input by optometrists | 124 (56) | 296 (79) | <0.0001 |
| Patients aged over 85 years | 53 (24) | 28 (8) | <0.0001 |
| Vision at listing: | — | ||
| Counting fingers or worse | 49 (22) | 29 (8) | <0.0001 |
| 6/18-6/60 | 96 (43) | 200 (54) | 0.016 |
| 6/12 or better | 69 (31) | 145 (39) | 0.059 |
| Second eye listing | 84 (38) | 158 (42) | 0.29 |
| Day case admission | 141 (64) | 344 (92) | <0.0001 |
| Local anaesthesia | 191 (87) | 361 (98) | <0.0001 |
| Phacoemulsification | 146 (67) | 361 (98) | <0.0001 |
| Intraoperative complications | 36 (16) | 22 (6) | <0.0001 |
| Grade of surgeons: | |||
| Senior house officer | 7 (3) | 38 (10) | 0.043 |
| Specialist registrar | 36 (16) | 62 (17) | — |
| Associate specialist | 22 (10) | 0 | — |
| Consultant | 154 (69) | 270 (72) | — |
| Cancelled on day | 3 | 4 | — |
| Postoperative visits: | |||
| ≤2 | 32 (15) | 312 (84) | <0.0001 |
| 1 | 13 (6) | 91(25) | <0.0001 |
| Postoperative vision 6/12 or better | 194 (89) | 343(93) | 0.089 |
Clinical outcome
Significantly more patients were aged 85 or more in 1997 at the time of cataract surgery (P<0.001). Over 20% of patients had profoundly reduced vision at counting fingers before cataract surgery, and this was significantly more than in 2004 (P<0.001). More operations were carried out as day cases with local anaesthesia using the phacoemulsification technique (P<0.001). Significantly fewer intraoperative complications (posterior capsule rupture, vitreous loss, zonular dehiscence, and iris prolapse) led to fewer postoperative complications and postoperative visits before discharge in 2004 (P<0.0001). More patients achieved a postoperative visual acuity of 6/12 or better in 2004 compared with 1997. Neither group had cases of endophthalmitis, retinal tear, or return to theatre.
Lessons learnt
Streamlining referrals, general practitioners, and optometric input
We found that streamlining cataract referrals significantly reduced waiting times (fig). The general practitioners and optometrists were canvassed and were in full support of providing an updated optometry report. This was crucial in reducing false positive referrals. Twenty per cent of patients still had no optometry report. We believe this was because of a small group of transient trainees in both general practice and optometry who are not familiar with local referral practices. This problem has been circumvented by the cataract nurses telephoning the patient, general practitioner, or optometrist for an updated optometry report.
Cataract pathway; changes over time for cataract surgery at Queen Margaret Hospital, Dunfermline
Specialist nurse role
The recruitment of nurses who specialise in cataract surgery, working to protocol in accordance with Royal College of Ophthalmologists guidelines, has dramatically increased the numbers of patients assessed for cataract surgery.19 Postoperative care has traditionally been the remit of medical staff, but in our centre this was almost completely devolved to specialist nurses. In turn this allowed more operations to be carried out.
Purpose built cataract unit
The redesign helped shorten the patients' journey through the hospital thus allowing for more operations in the same theatre session. Critical to this was the time previously lost in between operations by the patients' travel and transfer between different groups of nurses.
The cost of tendering the 600 extra cataract operations (carried out in 2004 compared with 1997) to outside contractors would have been £360 000 at a costing of £600 per operation. Thus over two years we have recouped the capital cost of the rebuild.
Medical staff and training issues
No net increase occurred in senior medical ophthalmology staff during this period. The increased surgical training opportunities attracted an extra specialist registrar. High turnover has not been at the expense of compromising training or surgical standards. Over three months in 1997 trainees carried out 43 operations compared with 100 in 2004, thus more than doubling our training opportunities. Our goals were helped by the almost complete conversion to small incision phacoemulsification cataract surgery resulting in fewer intraoperative complications and postoperative visits.
Vision at time of listing for surgery is the single most important feature in threshold for cataract surgery.16 Studies have estimated that 1280 cataract operations are required per annum for a population of 400 000 with a listing vision of 6/18 or worse. We have exceeded this number and are therefore now in a position to increase our trainee numbers and offer our services to neighbouring trusts.
Improvements in quality of care
The redesign has meant that quality of care has improved for patients requiring cataract surgery in Fife. The waiting time for cataract surgery decreased from 72 to 14 weeks in 2004. Twenty per cent of our patient cohort were aged 85 years or more and 20% had a preoperative vision of counting fingers before cataract surgery in 1997 compared with less than 8% for both indices in 2004. We interpret this as elderly people in Fife now having cataract surgery earlier in their lifespan with fewer presentations of dense cataracts.
We strive towards continuous quality improvement. This year we achieved a further target—patients having cataract surgery 18 weeks from their optometry visit. We hope soon to pilot electronic optometric referral directly to the one stop cataract clinic. We audit all aspects of our cataract surgery and this year we were able to show the trust our performance data and secure additional theatre sessions.
We have shown that modest, long sighted investment in the NHS can have a dramatic effect on the quality and throughput of cataract surgery while maintaining surgical training standards and consolidating continuity of care without recourse to provision of care from sources outside the NHS. Patients with cataracts may benefit from surgery earlier in their lifespan and before they reach severe visual impairment. This study provides an example to other trusts of excellence that can be achieved within the NHS providing cataract surgery, the commonest elective surgical procedure carried out in elderly people.4
Key learning points
Increased productivity for cataract surgery can be achieved by streamlining referrals with optometric input, specialist nurse clinics, and space rebuild
Modest NHS investment in redesign can increase throughput for cataract surgery by 60%, with maintenance of quality of care and training opportunities
Contributors: AT and RS proposed the study. AT and BG carried out data collection and interpreted the data. BG, DH, SS, PK, and RS formed part of the redesign committee and think tank for the redesign of the cataract service.
Funding: None.
Competing interest: None declared.
References
- 1.Raferty J, Stevens A, eds. Cataract surgery. London: NHS Executive, 1994.
- 2.Desai P, Reidy A, Minassian DC, Vafidis G, Bolger J. Gains from cataract surgery: visual function and quality of life. Br J Ophthalmol 1996;80:868-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brenner MH, Curbow B, Javitt JC, Legro MW, Sommer A. Vision change and quality of life in the elderly. Response to cataract surgery and treatment of other chronic ocular conditions. Arch Of Ophthalmol 1993;111:680-5. [DOI] [PubMed] [Google Scholar]
- 4.UK Department of Health. Hospital activity and episode statistics. www.doh.gov.uk/public/stats1.htm.
- 5.Reidy A, Minassian DC, Vafidis G, Joseph J, Farrow S, Wu J, et al. Prevalence of serious eye disease and visual impairment in a north London population: population-based, cross sectional study. BMJ 1998;316:1643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minassian DC, Reidy A, Desai P, Farrow S, Vafidis G, Minnassian A. The deficit in cataract surgery in England and Wales and the escalating problem of visual impairment: epidemiological modelling of the population dynamics of cataract. Br J Ophthalmol 2000;84:4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray CS, Crabtree HL, O'Connell JE. Waiting in the dark: cataract surgery in older people. BMJ 1999;318:1367-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jakko L, Laatikainen L. The decrease of visual acuity in cataract patients waiting for surgery. Acta Ophthalmol Scand 1999;77:681-4. [DOI] [PubMed] [Google Scholar]
- 9.UK Department of Health. Action on cataracts: good practice guidance. Jan 2000 www.dh.gov.uk.
- 10.Guly C, Sidebottom R, Hakin K, Bates K. Treatment centres and their effect on surgical training. BMJ 2005;331:1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferris JD. Independent sector treatment centres (ISTCS): early experience from an ophthalmology perspective. Eye 2005;19:1090-8. [DOI] [PubMed] [Google Scholar]
- 12.Harrad R. Local funding would reduce waiting lists for cataracts. BMJ 2002;325:1033. [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly SP. Recurring policy errors: blind spots over cataracts. Lancet 2005;366:1691. [DOI] [PubMed] [Google Scholar]
- 14.Desai P, Reidy A, Minassian DC. Profile of patients presenting for cataract surgery in the UK: national data collection. Br J Ophthalmol 1999;83:893-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Desai P, Minassian DC, Reidy A. National cataract surgery survey 1997-8: a report of the results of the clinical outcomes. Br J Ophthalmol 1999;83:1336-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Taylor H. Cataract: how much surgery do we have to do? Br J Ophthalmol 2000;84:1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fife Acute Hospitals Trust. http://intranet.faht.fife .
- 18.Information and Statistics Department, Scotland. www.isdscotland.org/isd .
- 19.Royal College of Ophthalmologists. Cataract surgery guidelines. London: RCO, 2004.