Abstract
Background
Despite well-known benefits of physical activity for older adults, about two thirds are underactive. Community-based programs are needed to facilitate increased physical activity. We examine the effectiveness of CHAMPS II, an inclusive, choice-based physical activity promotion program to increase lifetime physical activity levels of seniors. CHAMPS guided participants to choose activities that took into account their health, preferences, and abilities. It offered information on ways for them to exercise safely, motivate themselves, overcome barriers, and develop a balanced exercise regimen.
Methods
A 1-year randomized controlled trial was conducted with physically underactive seniors in a multispecialty group practice. Changes in self-reported physical activity by group were evaluated using ANCOVA, controlling for age and sex.
Results
Of 173 randomized subjects, 164 (95%) completed the trial. Subjects were aged 65 to 90 years (M = 74, SD = 6); 66% were female. The intervention group increased estimated caloric expenditure by 487 calories/week in moderate (or greater) intensity activities (MET ≥3.0; p < .001) and by 687 calories/week in physical activities of any intensity (p = .001). Control group changes were negligible. Between-group analyses found that the changes were significantly different in both measures (p values < .05). Overweight persons especially benefited from this program. The program was as effective for women, older adults (75+), and those who did not set aside time to exercise at baseline.
Conclusions
The program led to meaningful physical activity increases. Individually tailored programs to encourage lifestyle changes in seniors may be effective and applicable to health care and community settings.
THE increasing burden of health problems and health care costs of our burgeoning older population requires more preventive approaches. Regular physical activity is a prominent strategy, based on a large body of evidence that it contributes substantially to the health, functioning, and quality of life of older adults (1–3). Physical activity may also be associated with less frequent utilization of health services (4–7).
One is never too old to derive benefits from regular physical activity. Indeed, those who are sedentary or weak often gain the most health benefit by becoming more active (8–10). Further, moderate-intensity physical activity is beneficial (11,12) and easier for older adults to adhere to than vigorous activity (13).
Most older adults, however, remain significantly underactive (2). Only about 25% of men and 20% of women aged 65 years and older meet the national guidelines for regular physical activity (2). In three national data sets, among those aged 65 to 74, 28% to 37% of women and 18% to 33% of men reported no participation (2). Among those aged 75 and older, 38% to 54% of women and 27% to 38% of men reported no participation in any leisure time physical activity.
A critical next step is to implement practical and inclusive community-based programs to increase the physical activity levels of sedentary and underactive older adults. Most physical activity studies of older adults focus on examining health or fitness outcomes of various physical activity prescriptions or protocols, with physical activity as the independent variable. Very few have been designed specifically to change the lifestyle of older adults, that is, to help participants make regular physical activity and/or exercise a routine part of their lives (14). In such studies, the independent variable is whether or not they received a program of support for lifestyle changes (15). Participants in such programs choose the activity or set of activities they would like to do (with guidance) and set their own goals for increasing activity. This feature of choice enables individual preferences, which vary among older adults (16,17), to be taken into account, as well as readiness to change (18).
This article examines the effectiveness of the Community Healthy Activities Model Program for Seniors (CHAMPS II) a lifestyle program based on the personal choice model that promotes increased physical activity levels. We evaluate the physical activity outcomes of this program using a randomized design and determine whether the program worked equally well for subgroups likely to have more difficulty changing their physical activity behavior (e.g., completely sedentary, overweight participants).
METHODS
Subjects/Setting
CHAMPS II was offered to members of two Medicare health maintenance organizations (HMOs) through a large multispecialty group practice. Eligibility included: (1) being sedentary or underactive (not engaging in moderate-intensity physical activity at least three times weekly for at least 20 minutes per time and for at least 3 months); (2) having no serious medical conditions that could limit participation in light-to-moderate physical activity (unstable angina, uncontrolled hypertension, type I diabetes, or diagnosed with or hospitalized for chest pain, heart attack, or heart surgery in the past 6 months); (3) no severe functional impairment due to multiple medical or psychiatric diseases; (4) not planning to move from the area within 2 years; (5) English speaking and cognitively intact; (6) not a participant in CHAMPS I (19); and (7) living in a community near the group practice. Only one person per household was eligible.
Design
A randomized controlled trial was used; eligible subjects were randomized to the 1-year physical activity promotion intervention or to a wait-list control group (program offered at the end of the year). To identify eligible persons and define the population, an enumeration survey of a random sample of HMO enrollees was conducted. Eligible persons were invited to attend an informational meeting where the program was explained and they were invited to enroll. All methods were approved by the appropriate internal review boards.
Methods of Recruitment
A two-phased proactive recruitment strategy was used. Initial contact letters (from a group-practice geriatrician) were sent to 1381 randomly sampled Medicare HMO enrollees aged 65 and older. Of the 1134 (82%) directly contacted, 1053 were eligible for the survey, and 893 responded (85% of those contacted and eligible for the survey). Persons eligible for the intervention were invited to attend an informational meeting at which the program and study were described and they were invited to join. Those signing up were given a packet containing the informed consent, baseline questionnaires, and a baseline assessment appointment. Informed consent was obtained at the baseline assessment. Recruitment details are described elsewhere (20,21).
Screening for medical safety
Because CHAMPS involved individual choice of physical activity, including “on their own” options, medical screening was conducted to avoid enrolling individuals who should not initiate an unsupervised physical activity program. A study nurse measured blood pressure and reviewed a self-report medical history with each participant. A study physician then reviewed the medical history and discussed special issues with the nurse; where questions of safety remained, the participant’s personal physician was involved in the final approval (22). Letters were sent to the physicians of all who passed this screen, notifying them of the program and their patient’s participation, and asking them to contact study staff if they had any concerns. Medical history updates were obtained at each subsequent assessment. No adverse events associated with the program occurred during the study.
Method of randomization
During a personal enrollment meeting following baseline, subjects were randomized. The Efron procedure (23) was used, which promotes randomization that assures near-equal sample sizes and good representation on variables of interest (e.g., gender, age) in both groups at all stages of randomization.
CHAMPS Physical Activity Promotion Program
CHAMPS II was based on an earlier version of CHAMPS conducted in congregate housing settings. The first version was a 6-month program encouraging participation in existing community-based physical activity classes and programs as a way to increase physical activity. It was successful in increasing class participation (19).
CHAMPS II was a public health model program that included people with a range of health problems on the premise that there is some beneficial type of physical activity for everyone. It was based on social cognitive theory and included principles of self-efficacy enhancement and readiness to change, as well as motivational techniques (24–26). It also drew from the intervention experiences of researchers at Stanford University (12).
The program goals were to encourage and support long-term increases in physical activity of sedentary and under-active older adults. Although each participant was instructed to start slowly and increase gradually from their current activity levels, the long-term goal was at least 30 minutes of moderate-intensity activity most or all days of the week (2,13,27). Participants were also encouraged to develop a balanced program (endurance, strength training, flexibility, balance, and coordination).
Trained staff assisted participants to develop and maintain a physical activity regimen that participants would be capable of sticking with and could participate in throughout their lives. Program staff used client-centered motivational, behavioral, and cognitive techniques to encourage participants to join classes and programs in the community and/or to develop a regimen on their own. The program was individually tailored; that is, participants were encouraged to develop a program or regimen for themselves that took into account their health problems, preferences for type of activity, ability, and other factors. Thus, activities varied across individuals. Participants explored ways to motivate themselves, overcome barriers, exercise safely, progress slowly to avoid injury, and engage in appropriate levels of physical activity in the presence of various chronic conditions and limitations without hurting themselves. Information, support, and opportunities for skill building were provided through an informational meeting, an individual planning session, monthly group workshops, physical activity diaries, regular staff-initiated telephone calls from a counselor, monthly newsletters, and functional fitness assessments.
The individual physical activity planning session included discussion of the participant’s readiness to increase physical activity, general safety considerations, disease-specific precautions, and physical activity options and preferences. Two booklets were provided: Pep Up Your Life (28) and Exercise and Your Heart (29).
Each participant had the opportunity to attend ten unique group workshops. Two initial workshops covered the basics of exercising safely and exercises to improve cardiorespiratory fitness, strength, and flexibility. Attendance at these two workshops was strongly encouraged. For those unable to attend, this information was provided by telephone and handouts were mailed. Additional optional workshops covered topics such as fall prevention, nutrition, and stress management; a walking clinic was also offered.
Measures
Because of the policy emphasis on moderate-intensity activity, the main outcome measure was estimated calories expended per week in at least moderate-intensity physical activities (e.g., walking briskly, swimming, using a stationary cycle, and heavy gardening) having a metabolic equivalent (MET) value of ≥3.0. One MET is the amount of energy expended sitting at rest (3.5 ml of oxygen per kilogram of body weight per minute for the average adult). Activities classified as at least moderate intensity require at least three times the amount of energy expended sitting (30). We also examined the effectiveness in terms of estimated caloric expenditure in exercise-related physical activities of all intensities. This is because many underactive older adults will benefit from increases in lighter forms of activity (e.g., leisurely walking, stretching, general conditioning). We present results on both measures.
The measures of physical activity, obtained from the self-report CHAMPS Physical Activity Questionnaire for Older Adults, are described elsewhere (31,32). These other studies provide evidence of reliability and construct validity; reliability and validity findings for an earlier version of these measures are also available(19).
Methods of Analysis
To examine program effectiveness over 1 year in terms of physical activity (primary study outcome), we conducted analysis of covariance (ANCOVA) using general linear models to predict each 1-year physical activity outcome as a function of group assignment (intervention vs control), controlling for baseline level of physical activity, age, and sex.
To explore whether the program was equally effective for important subgroups, we used the same approach but added an interaction term for subgroup membership by group assignment. Four subgroup analyses were conducted for each physical activity measure. Each included one interaction for the following subgroups: older age (≥75 years), overweight (body mass index ≥27.0), female, and sedentary (did not set aside time for exercise or recreational sports at screening). All analyses were performed using SAS 6.12 (SAS Institute, Cary, NC).
RESULTS
Subject Characteristics
Over the 5-month recruitment period, we enrolled 173 individuals (33% of those who were eligible, 60% of those attending an informational meeting). Of the 173 randomized persons, 164 (95%) completed the trial. Of the 9 lost to follow-up at 1 year, 4 died and 5 dropped out (4 in the intervention and 5 controls). Reasons included serious illness unrelated to the program and lack of interest in participating and completing activity diaries. Final subjects (n = 164) ranged in age from 65 to 90 years (mean = 74 ± 6), with 66% female and 9% minority (see Table 1). Nearly half of the subjects were sedentary (did not set aside time for exercise or recreational sports) at baseline. No differences between those who completed the trial and those who did not were observed in demographic, health, or physical activity level variables. As a public health model program, we aimed to be as inclusive as possible by including those with a variety of chronic conditions. Thus, subjects had a range of health conditions.
Table 1.
Sample Characteristics at Baseline
| Randomized Group* |
|||
|---|---|---|---|
| Characteristic | Total Sample (N = 164) | Intervention (n = 81) | Control (n = 83) |
| Age | |||
| Mean, SD | 74.4 (5.9) | 74.3 (5.9) | 74.6 (5.8) |
| Range | 65–90 | 65–90 | 65–87 |
| Education (%) | |||
| High school or less | 18.9 | 18.5 | 19.3 |
| Some college | 25.0 | 23.5 | 26.5 |
| College degree | 27.4 | 28.4 | 26.5 |
| Some graduate school | 6.7 | 7.4 | 6.0 |
| Graduate degree | 22.0 | 22.2 | 21.7 |
| Female (%) | 65.9 | 69.1 | 62.7 |
| Income (%) | |||
| Less than $20,000 | 19.1 | 15.8 | 22.4 |
| $20,000 to $40,000 | 46.1 | 48.7 | 43.4 |
| More than $40,000 | 34.9 | 35.5 | 34.2 |
| Minority (%) | 8.5 | 8.6 | 8.4 |
| Married (%) | 56.1 | 59.3 | 53.0 |
| Employed full or part time (%) | 15.2 | 14.8 | 15.7 |
| Self-rated health fair or poor (%) | 11.6 | 11.1 | 12.0 |
| Hypertension (%) | 39.6 | 42.0 | 37.4 |
| Arthritis or joint problems (%) | 64.6 | 70.4 | 59.0 |
| Cardiovascular problems (%) | 15.9 | 19.8 | 12.0 |
| Asthma, chronic bronchitis, or emphysema (%) | 9.8 | 7.4 | 12.0 |
| Diabetes (%) | 7.3 | 8.6 | 6.0 |
| Does not set aside time for exercise (sedentary) (%) | 44.5 | 43.2 | 45.8 |
None of the measures differed significantly between the intervention and control group.
No significant differences were observed between the intervention and control group on any baseline demographic, health, or physical activity variable, supporting the adequacy of the randomization process.
Physical Activity Outcomes
Main effects
Those in the intervention group increased their estimated caloric expenditure in moderate-intensity (or greater) activities more than those in the control group: F(1,159) = 8.84, p = .003. Using the same approach, the intervention group also increased their caloric expenditure in all activities significantly more than the control group: F(1,159) = 9.06, p = .003. Within-group analyses indicated that those in the intervention group increased their estimated caloric expenditure in moderate-intensity activities by 487 calories per week (p < .001) whereas the control group changes were negligible (+5 calories/week; see Figure 1). Similarly, estimated caloric expenditure in all activities was increased by 687 calories/week in the intervention group (p < .001). Again, the control group did not change (−10 calories/week).
Figure 1.
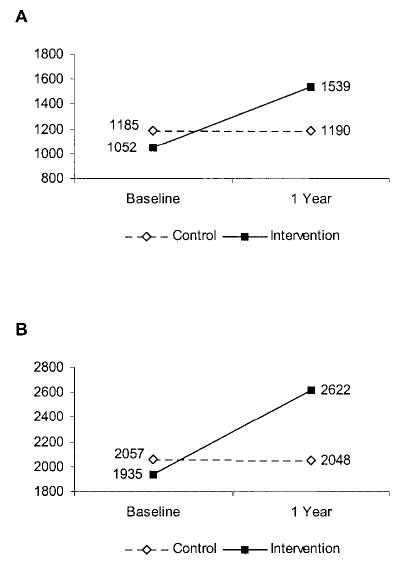
A, Estimated caloric expenditure per week in moderate-intensity physical activities, baseline and 1-year. F(1,168) = 8.84, p = .003; +487, p < .001; +5, not significant. B, Estimated caloric expenditure per week in all physical activities, baseline and 1-year. F(1,168) = 9.06, p = .003; +687, p < .001, −10, not significant
For both physical activity measures, residuals were examined with regard to outliers, distributions, and fit, conditional on each of the four variables in the model (group, baseline physical activity level, age, and gender). On the basis of these findings, we judged that the models fit well. A sensitivity analysis using a more conservative “intention to treat” approach, in which the last known value of physical activity level was used for the 1-year value in the ANCOVA, produced virtually identical results.
Interactions
Results of the interaction tests indicated that the program was as effective for women, the older age group, and the sedentary as it was for their counterparts (p > .10 for moderate-intensity (or greater) activity and p > .25 for all activities). For persons who were overweight, the interaction was significant for both moderate-intensity activities: F(1,157) = 6.21, p < .05) and all activities: F(1,157) = 7.38, p < .01. Overweight persons in the intervention group increased their physical activity (in a way similar to the non-overweight); overweight persons in the control group decreased their physical activity levels (in contrast to non-overweight people in the control group who did not change). The interaction is plotted in Figure 2 for “all activities.” The pattern for moderate-intensity activities (not presented) is nearly identical.
Figure 2.
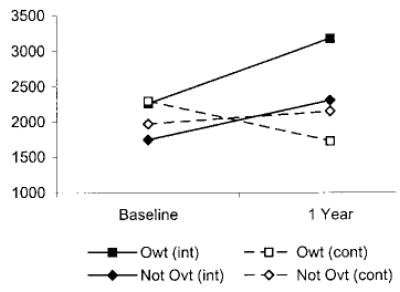
Estimated caloric expenditure per week in all physical activities by overweight category and group. F(1,157) = 7.38.
To explore whether this interaction was observed when using a caloric expenditure measure that was not adjusted for weight, we repeated the tests using a measure of METS/kilogram of body weight/week. The interaction remained significant for all activities (p < .05) and showed a trend for moderate-intensity activities (p = .07).
Because of the overweight interactions, we explored whether the trial was associated with any weight loss. Within-group analyses indicated that those in the intervention group reduced their body mass index (BMI), based on self-reported weight and height, by .496 (p = .0001), whereas those in the control group did not change (.004, NS). The weight loss in the intervention group is equivalent to approximately 3 lb. For between-group comparisons, we used ANCOVA, predicting BMI at 1 year as a function of baseline BMI, controlling for age and sex. Between-group comparisons indicated that these differences between groups were significant: F(1,154) = 8.45, p < .01.
DISCUSSION
The fact that the CHAMPS II program achieved a substantial and meaningful level of increased physical activity participation over 1 year is very encouraging. The magnitude of increase of nearly 500 cal expended per week in moderate-intensity or more vigorous activities is equivalent to adding approximately a 1-mile (i.e., about 20 minutes) brisk walk 5 times a week to a person’s previous physical activity regimen. Similarly, the increase of nearly 700 cal expended per week in all activities is equivalent to adding five 1-mile brisk walks per week along with additional activities such as leisurely walking, general conditioning exercises (e.g., calisthenics), stretching, or gardening. The types of physical activities in which enrollees in the intervention group participated at the end of the year varied; the most prevalent were walking leisurely, gardening, stretching/flexibility, heavy housework, and walking briskly.
As noted earlier, the CHAMPS II approach falls under the rubric of “lifestyle” physical activity interventions (15). The main feature of lifestyle interventions is that individuals choose their own form of activity rather than having the types and/or intensities of activities prescribed by the study. This feature makes lifestyle approaches particularly appealing for achieving the public health goals of increased activity for the older adult population. One of the few programs for older adults that is similar to CHAMPS II is the Groningen Active Living Model (GALM) developed in The Netherlands (33). The GALM program uses behavioral change strategies to stimulate leisure-time physical activity participation. The Dutch program includes a 12-week introductory phase and a 1-year follow-up phase. As in CHAMPS II, the program uses an individually tailored approach in which the type, format, intensity, frequency, and location of the activity is based on the participants’ needs. The GALM program has not yet been evaluated fully. There are only a few other studies in which the type and intensity of physical activity were chosen by participants, with guidance from study staff, but none of these focused on older adults (15,34,35).
Because of the paucity of information on how well physical activity interventions work to increase physical activity for subgroups, our findings that the program appeared to be as effective for women, the sedentary, and older age groups help to fill this gap. The little evidence available pertains to program effectiveness by gender and is inconsistent (14). In Project Active, aimed at adults aged 35 to 60, men were more likely to increase their physical activity at the 6-month assessment (36); however, this was not true at the 24-month follow-up (37).
Even more interesting is the finding that the intervention was particularly useful in increasing physical activity for overweight persons. Others have found that overweight persons assigned to at-home exercise were more likely to adhere than those assigned to group-based exercise (38). It is possible that their increased participation in this study was facilitated by the individually tailored focus of CHAMPS in which overweight persons chose their own form of activities.
Our exploratory finding that those in the intervention group reduced their BMI significantly was unexpected. A reduction of BMI equivalent to a loss of 3 pounds, although not large, is consistent with the findings that overweight enrollees increased their activity as much as they did. One randomized trial of younger overweight women found that a lifestyle approach to physical activity focusing on incorporating short bouts of activity into their daily schedules, as opposed to structured aerobic exercise, helped women maintain their weight loss longer (both approaches were combined with diet changes) (39).
Limitations of the CHAMPS II study from a public health perspective are that the sample was fairly well educated and did not include many minority participants (due to their limited representation in the local population), as well as the fact that the study was conducted in a high quality health care setting. Thus, the program may not be generalizable to more vulnerable populations. On the other hand, offering the program to a well-defined population such as members of an HMO is practical, allowing us to use outreach recruitment methods. An outreach approach enables better representation of the target population than would be possible through advertisements at local venues.
Strengths include the randomized controlled design and the high level of subject retention (95%). We attribute the minimal subject loss to the fact that subjects were not pressured to participate in physical activity, but were encouraged to complete the assessments. Another strength is the relatively high rate of enrollment from those in the HMOs who were eligible (33%). This rate is considered high relative to other studies that have used population-based recruitment strategies (12) because it required a 1-year commitment to complete monthly forms and quarterly assessments. We represented a broad range of ages (65–90 years) and had inclusive eligibility criteria, particularly with respect to health. Indeed, the proportion of those with various chronic diseases is roughly comparable to the proportion in the older adult population (40). These features make this program appropriate for most older Americans.
Future research could test the program’s effectiveness in more diverse settings and communities, particularly settings that include more minority groups and persons with lower socioeconomic status. The program would probably need to be adapted to match the needs, interests, and resources of other communities and settings. Future studies could test the mechanisms by which the program is effective, for example, through enhanced self-efficacy or reduction of barriers to exercise (41). Finally, information on whether this program or others like it can reduce the costs of health care (7,42) will aid decisions about adopting such programs in health care settings. In sum, results indicate that the program was successful in promoting meaningful increases in physical activity. We believe that one of the major strengths of this program is its ability to be translated into other health care and community settings.
Acknowledgments
This work was supported by National Institute on Aging Grant AG09931. We gratefully acknowledge the valuable contributions of Judy Goldstein and Drs. Dianne Christopherson, William L. Haskell, Patricia Painter, Leslie Pruitt, and June Flora. In addition, the assistance of numerous staff members at the Palo Alto Medical Foundation where the program was conducted was invaluable. The work presented here was approved by the institutional review boards of the University of California San Francisco and Stanford University and informed consent was obtained from all subjects.
Footnotes
Decision Editor: Jhon E. Morley, MB, BCh
References
- 1.American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 1998;30:992–1008. [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. pp. 85–172. [Google Scholar]
- 3.U.S. Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. Washington, DC: U.S. Department of Health and Human Services; Nov, 2000. [Google Scholar]
- 4.Wetzler HP, Cruess DF. Self-reported physical health practices and health care utilization: findings from the National Health Interview Survey. Am J Public Health. 1985;75:1329–1330. doi: 10.2105/ajph.75.11.1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shephard RJ. Economic Benefits of Enhanced Fitness. Champaign, IL: Human Kinetics Publishers; 1986. [Google Scholar]
- 6.Harris SS, Caspersen CJ, DeFriese GH, Estes EH. Physical activity counseling for healthy adults as a primary preventive intervention in the clinical setting. JAMA. 1989;261:3590–3598. [PubMed] [Google Scholar]
- 7.Pronk NP, Goodman MJ, O’Connor PJ, Martinson BC. Relationship between modifiable health risks and short-term health care changes. JAMA. 1999;282:2235–2239. doi: 10.1001/jama.282.23.2235. [DOI] [PubMed] [Google Scholar]
- 8.Paffenbarger RS, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328:538–545. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- 9.Buchner DM, deLateur BJ. The importance of skeletal muscle strength to physical function in older adults. Ann Behav Med. 1991;13:91–98. [Google Scholar]
- 10.Haskell WL, Montoye HJ, Orenstein DR. Physical activity and exercise to achieve health-related physical fitness components. Public Health Rep. 1985;100:202–212. [PMC free article] [PubMed] [Google Scholar]
- 11.Blair SN, Goodyear NN, Gibbons LW, Cooper KH. Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA. 1984;252:487–490. [PubMed] [Google Scholar]
- 12.King AC, Haskell WL, Taylor CB, Kraemer HC, DeBusk RF. Group-vs home-based exercise training in healthy older men and women: a community-based clinical trial. JAMA. 1991;266:1535–1542. [PubMed] [Google Scholar]
- 13.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273:402–407. doi: 10.1001/jama.273.5.402. [DOI] [PubMed] [Google Scholar]
- 14.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults: a critical review and recommendations. Am J Prev Med. 1998;15:316–333. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 15.Dunn AL, Andersen RE, Jakicic JM. Lifestyle physical activity interventions: history, short- and long-term effects, and recommendations. Am J Prev Med. 1998;15:398–412. doi: 10.1016/s0749-3797(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 16.Wilcox S, King AC, Brassington GS, Ahn DK. Physical activity preferences of middle-aged and older adults: a community analysis. J Aging Phys Activity. 1999;7:386–399. [Google Scholar]
- 17.Mills KM, Stewart AL, Sepsis PG, King AC. Consideration of older adults’ preferences for format of physical activity. J Aging Phys Activity. 1997;5:50–58. [Google Scholar]
- 18.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11:257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 19.Stewart AL, Mills KM, Sepsis PG, et al. Evaluation of CHAMPS, a physical activity promotion program for older adults. Ann Behav Med. 1997;19:353–361. doi: 10.1007/BF02895154. [DOI] [PubMed] [Google Scholar]
- 20.McLellan BY, Stewart AL, Mills KM, Verboncoeur CJ, Sperber N, Ritter PL. Using motivational interviewing techniques to recruit older adults into a physical activity study. Ann Behav Med. 1997;19(Suppl):S103. [Google Scholar]
- 21.Mills KM, Stewart AL, McLellan BY, Verboncoeur CJ, King AC, Brown BW. Evaluation of enrollment bias in a physical activity promotion program for seniors. J Aging Phys Activity. In press. [Google Scholar]
- 22.Christopherson D, Gillis D, Bortz WM, II, King AC, Ritter P, Stewart AL. Health screening procedures for a Medicare HMO physical activity promotion program. Med Sci Sports Exerc. 1997;29(Suppl):S103. [Google Scholar]
- 23.Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–417. [Google Scholar]
- 24.Bandura A. Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 25.Rollnick S, Bell A. Brief motivational interviewing for use by the nonspecialist. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People to Change Addictive Behavior. New York: The Guilford Press; 1991. [Google Scholar]
- 26.Prochaska JO. A transtheoretical model of behavior change: learning from mistakes with majority populations. In: Becker DM, Hill DR, Jackson JS, Levine DM, Stillman FA, Weiss SM, editors. Health Behavior Research in Minority Populations: Access, Design, and Implementation. Bethesda, MD: National Institutes of Health; 1992. pp. 105–111. [Google Scholar]
- 27.NIH Consensus Development Panel on Physical Activity and Cardiovascular Health. Physical activity and cardiovascular health. JAMA. 1996;276:241–246. [PubMed] [Google Scholar]
- 28.American Association of Retired Persons. Pep Up Your Life. Washington, DC: American Association of Retired Persons; 1994. [Google Scholar]
- 29.American Heart Association. Exercise and Your Heart: A Guide to Physical Activity. Dallas, TX: American Heart Association; 1993. [Google Scholar]
- 30.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS Physical Activity Questionnaire for Older Adults: outcomes for interventions. Med Sci Sports Exerc. doi: 10.1097/00005768-200107000-00010. In press. [DOI] [PubMed] [Google Scholar]
- 32.Harada ND, Chiu V, King AC, Stewart AL. An evaluation of three self-report physical activity instruments for older adults. Med Sci Sports Exerc. doi: 10.1097/00005768-200106000-00016. In press. [DOI] [PubMed] [Google Scholar]
- 33.Stevens M, Bult P, de Greef ML, Lemmink KA, Rispens P. Groningen Activity Living Model (GALM): stimulating physical activity in sedentary older adults. Prev Med. 1999;29:267–276. doi: 10.1006/pmed.1999.0545. [DOI] [PubMed] [Google Scholar]
- 34.King AC, Sallis JF, Dunn AL, et al. Overview of the Activity Counseling Trial (ACT) intervention for promoting physical activity in primary health care settings. Med Sci Sports Exerc. 1998;30:1086–1096. doi: 10.1097/00005768-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally tailored physical activity intervention. Ann Behav Med. 1998;20:174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 36.Dunn AL, Garcia ME, Marcus BH, Kampert JB, Kohl HW, Blair SN. Six-month physical activity and fitness changes in Project Active, a randomized trial. Med Sci Sports Exerc. 1998;30:1076–1083. doi: 10.1097/00005768-199807000-00009. [DOI] [PubMed] [Google Scholar]
- 37.Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA. 1999;281:327–334. doi: 10.1001/jama.281.4.327. [DOI] [PubMed] [Google Scholar]
- 38.King AD, Kiernan M, Oman RF, Kraemer HC, Hull M, Ahn D. Can we identify who will adhere to long-term physical activity? Signal detection methodology as a potential aid to clinical decision making. Health Psychol. 1997;16:380–389. doi: 10.1037//0278-6133.16.4.380. [DOI] [PubMed] [Google Scholar]
- 39.Andersen RE, Wadden TA, Bartlett SJ, Zemel B, Verde TJ, Franckowiak SC. Effects of lifestyle activity vs structured aerobic exercise in obese women: a randomized trial. JAMA. 1999;281:335–340. doi: 10.1001/jama.281.4.335. [DOI] [PubMed] [Google Scholar]
- 40.Benson V, Marano MA. Current estimates from the National Health Interview Survey, 1995. Vital and Health Statistics Series 10. 1998;(199):10. National Center for Health Statistics. [PubMed] [Google Scholar]
- 41.Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. How are we doing? How might we do better? Am J Prev Med. 1998;15:266–297. doi: 10.1016/s0749-3797(98)00080-4. [DOI] [PubMed] [Google Scholar]
- 42.Buchner DM, Cress ME, deLateur BJ, et al. The effect of strength and endurance training on gait, balance, fall risk, and health services use in community-living older adults. J Gerontol Med Sci. 1997;52A:M218–M224. doi: 10.1093/gerona/52a.4.m218. [DOI] [PubMed] [Google Scholar]


