Abstract
OBJECTIVE
To examine evidence for the role of omega-3 fatty acids in cardiovascular disease.
QUALITY OF EVIDENCE
PubMed was searched for articles on the role of omega-3 fatty acids in cardiovascular disease. Level I and II evidence indicates that omega-3 fatty acids are beneficial in improving cardiovascular outcomes.
MAIN MESSAGE
Dietary intake of omega-3 fatty acids has declined by 80% during the last 100 years, while intake of omega-6 fatty acids has greatly increased. Omega-3 fatty acids are cardioprotective mainly due to beneficial effects on arrhythmias, atherosclerosis, inflammation, and thrombosis. There is also evidence that they improve endothelial function, lower blood pressure, and significantly lower triglycerides.
CONCLUSION
There is good evidence in the literature that increasing intake of omega-3 fatty acids improves cardiac outcomes. Physicians need to integrate dietary recommendations for consumption of omega-3 fatty acids into their usual cardiovascular care.
Abstract
OBJECTIF
Relever les données sur le rôle des acides gras oméga-3 dans les maladies cardiovasculaires.
QUALITÉ DES PREUVES
On a consulté PubMed, à la recherche d’articles sur le rôle des oméga-3 dans les maladies cardiovasculaires. Il existe des preuves de niveaux I et II indiquant que les oméga-3 ont un effet favorable sur les issues cardiovasculaires.
PRINCIPAL MESSAGE
Au cours des 100 dernières années, la consommation des acides gras oméga-3 a diminué de 80%, pendant que celle des oméga-6 augmentait considérablement. Les oméga-3 sont cardioprotecteurs en raison surtout de leurs effets bénéfiques sur les arythmies, l’athérosclérose, l’inflammation et la thrombose. Selon certaines données, ils améliorent aussi l’activité endothéliale, diminuent la tension artérielle et causent une baisse significative des triglycérides.
CONCLUSION
Il existe dans la littérature des preuves convaincantes indiquant qu’une consommation accrue d’acides gras oméga-3 améliore les issues cardiaques. Le médecin devrait incorporer aux soins cardiovasculaires habituels des recommandations pour encourager la consommation des oméga-3.
EDITOR’S KEY POINTS.
Historically, the human diet was high in omega-3 fatty acids. The ratio of omega-6 to omega-3 fatty acids in the diet was 1-2:1. During the last 100 years, there has been a marked increase in consumption of omega-6 and a decrease in consumption of omega-3 fatty acids.
There appears to be good evidence (level I and II) of a lower incidence of hypertension, cardiac disease, all-cause mortality, and familial hypertriglyceridemia in patients who consume adequate amounts of omega-3 fatty acids.
Canada was the first country to adopt guidelines to reduce consumption of omega-6 and increase consumption of omega-3 fatty acids, with a target ratio of 6:1 in the diet. Most Canadians will not achieve this goal.
Family doctors can be confident that promoting a diet with increased intake of omega-3 fatty acids is an important preventive measure.
POINTS DE REPÈRE DU RÉDACTEUR.
Historiquement, l’alimentation humaine contenait beaucoup d’acides gras oméga-3 et il y avait un rapport de 1-2:1 entre les oméga-6 et les oméga-3 consommés. Au cours des 100 dernières années, la consommation des oméga-6 a fortement augmenté tandis que celle des oméga-3 diminuait.
Il y a des preuves de niveau I et II suggérant que la consommation d’une quantité adéquate d’acides gras oméga-3 réduit la mortalité globale et l’incidence d’hypertension, de maladies cardiaques et d’hypertriglycéridémie familiale.
Le Canada a été le premier pays à adopter des directives pour réduire la consommation des oméga-6 et augmenter celle des oméga-3, avec comme objectif un rapport de 6:1 dans l’alimentation. La plupart des canadiens n’atteindront toutefois pas cet objectif.
Le médecin de famille a raison de croire que le fait de préconiser un régime plus riche en oméga-3 est une importante mesure préventive.
During the last decade, the amount of research on omega-3 fatty acids has increased substantially. As a result, new guidelines recommend that patients at risk of cardiovascular (CV) disease increase their dietary intake of omega-3 fatty acids. This article looks at the role of omega-3 fatty acids of marine (eicosapentenoic acid [EPA], docosahexaenoic acid [DHA]) and plant (alpha-linolenic acid [ALA]) origin in CV health in order to bring family physicians up-to-date on current evidence.
Quality of evidence
Studies providing level I, II, and III evidence of the benefits of omega-3 fatty acids are reviewed in this article. MEDLINE was searched using the words “omega-3 fatty acids” and “fish oil” combined with “hypertension,” “coronary artery disease,” and “hypertriglyceridemia.” Trials involving humans were chosen.1-16
Omega-3 and omega-6 fatty acids
The lipids essential for health are the omega-3 and omega-6 polyunsaturated fatty acids (PUFA).17 Interest in omega-3 fatty acids began in 1972. Studies by Bang and Dyerberg3 showed that Greenland Inuit who consumed a diet high in protein and fat (mainly from fish) had significantly lower total cholesterol (P < .005), low-density lipoprotein (LDL)(P < .02), and triglyceride (P < .005) levels than most other people had.
Since then, much has been learned about the interaction of omega-6 and omega-3 fatty acids in CV disease and about the ratio between omega-6 and omega-3 fatty acids.18,19 Dietary intake of omega-3 fatty acids has decreased, and dietary intake of omega-6 fatty acids has substantially increased during the last 100 years due to greater use of vegetable oils high in omega-6 fatty acids.18,20 The ratio of omega-6 to omega-3 was about 1.5:1 as recently as 200 years ago and now is estimated at 16:1 in the average North American diet.18 This has resulted in a diet high in omega-6 fatty acids and deficient in omega-3 fatty acids.21
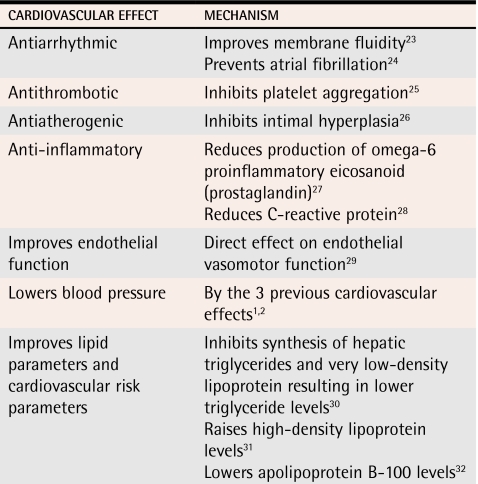
Omega-6 and omega-3 fatty acids compete for the same enzymes. An increase in the diet of one decreases metabolism of the other.22 Omega-6 fatty acid metabolites result in prostaglandins that are inflammatory; omega-3 fatty acids result in prostaglandins that are anti-inflammatory. The actions of omega-3 fatty acids on the CV system are listed in Table 1.1,2,23-33 Omega-3 fatty acids have antiarrhythmic effects, including preventing atrial fibrillation23,24; antithrombotic action25; antiatherogenic effects26; anti-inflammatory effects27,28; and the ability to improve endothelial function,29 lower blood pressure,1,2 lower triglyceride levels,30 increase high-density lipoprotein (HDL) levels,31 and decrease apolipoprotein B-100.32
Table 1.
Cardiovascular effects of omega-3 fatty acids
Data from Din et al.33
Hypertension
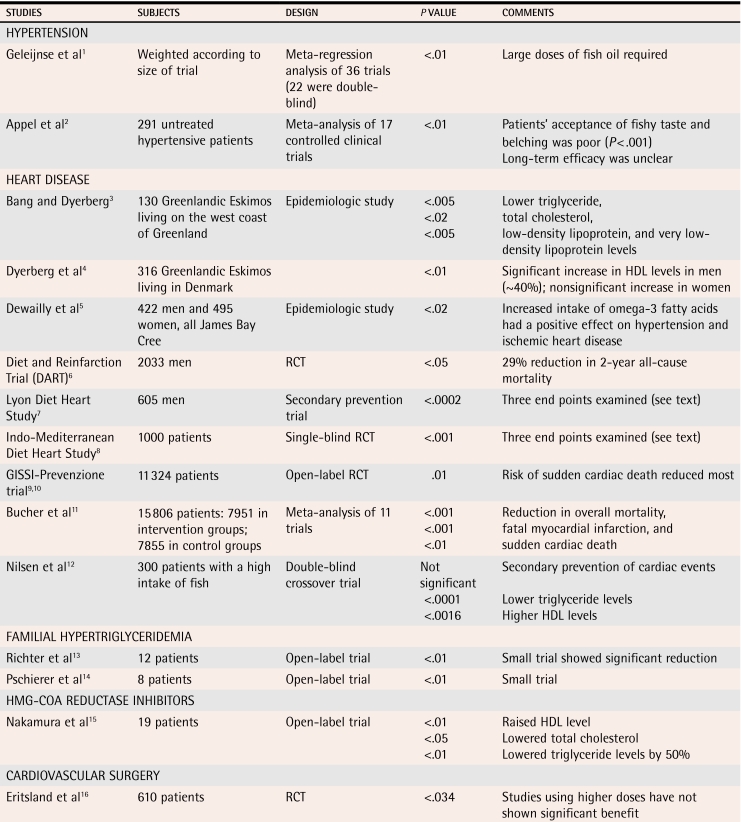
Trials are listed in Table 2.1-16 Geleijnse et al1 did a meta-analysis of 36 randomized trials (22 of which were double blind) carried out between 1966 and 2001 (level I evidence). The meta-analysis showed that consuming an average of 3.7 g/d of fish oil reduced systolic blood pressure (BP) by 2.1 mm Hg (P < .01) and diastolic BP by 1.6 mm Hg (P < .01). The BP-lowering effects were greater in people older than 45 years and in those whose BP was higher than 140/90 mm Hg.
Table 2.
Characteristics of studies on use of fish oil
HDL—high-density lipoprotein, RCT—randomized controlled trial.
A meta-analysis (level I evidence) done by Appel et al2 found a significant reduction in BP (5.5 mm Hg systolic BP and 3.5 mm Hg diastolic BP) in untreated hypertensive patients taking supplements of more than 3 g/d of omega-3 PUFA. High doses were required to achieve these results, and patients’ acceptance of the fishy taste and subsequent belching was poor (P < .001). Most trials lasted less than 3 months, so the long-term benefits are unclear.
Heart disease
Bang and Dyerberg3 and Dyerberg et al4 did epidemiologic studies (level II evidence) to establish the cardioprotective effects of omega-3 fatty acids from marine sources in the Inuit people of Greenland in the 1970s. Despite a high-fat diet, the incidence of CV disease was exceptionally low among these people. A Canadian study5 looking at James Bay Cree people reported fewer CV risk factors and higher levels of plasma omega-3 fatty acids in adult Cree living along the coast than in those living inland (level II evidence).
In September 1989, the Diet and Reinfarction Trial (DART)6 (level II evidence) was the first study to show that subjects who followed advice to eat fatty fish (high in omega-3 fatty acids) had a 29% reduction in 2-year all-cause mortality (P < .05). The study allocated 2033 men to 3 groups: group 1 reduced their fat intake and increased their intake of PUFA, group 2 increased their fatty fish intake, and group 3 increased their cereal fibre intake.
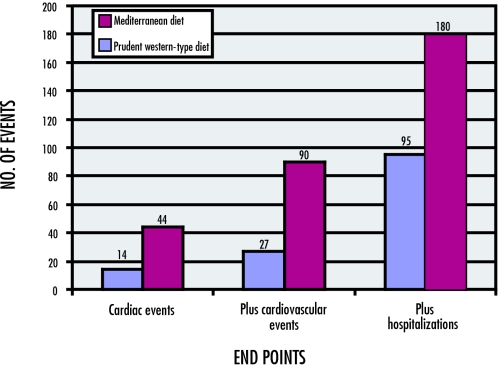
The Lyon Diet Heart Study,7 a secondary prevention trial (level I evidence), followed 605 men after myocardial infarction (MI) for 4 years. One group (n = 303) received a diet rich in omega-3 and omega-9 fatty acids and low in both omega-6 fatty acids and saturated fats (the Mediterranean diet). The second group (n = 302) followed the Prudent Heart Diet, which is similar to the American Heart Association diet. Three end points were used: cardiac death or non-fatal MI; cardiac death or non-fatal MI plus secondary end points including unstable angina, stroke, heart failure, and pulmonary or peripheral embolism; and all of the preceding plus minor events requiring hospital admission. The experimental group following the Mediterranean diet had fewer events at all end points. For the first end point, the first group had 14 events, and the second group 44 events (P < .0002). For the second end point, the first group had 27 events, and the second group had 90 events (P < .0002). For the third end point, the first group had 95 events, and the second group had 180 events (P < .0002)34 (Figure 17). The control group had an omega-6–to–omega-3 ratio of 10:1; the experimental group had a ratio of 4:1. A striking protective effect was reported with a 50% to 70% reduction in risk of recurrence of CV events after 4 years’ follow up.
Figure 1.
Data from the final report of the Lyon Diet Health Study7
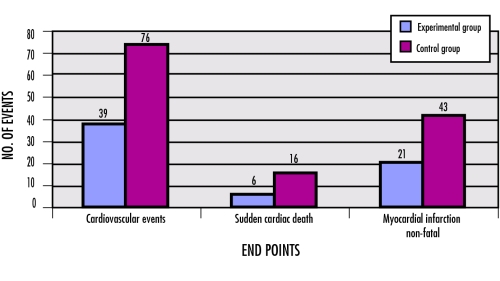
In the Indo-Mediterranean Diet Heart Study (1000 patients)8 (level I evidence), those in the experimental group (diet high in ALA) had fewer CV events than those in the control group (39 vs 76, P < .001). Also reduced were sudden cardiac death (6 vs 16, P < .015) and non-fatal MI (21 vs 43, P < .001) (Figure 27,34). Omega-6–to–omega-3 ratios were 38:1 before the trial and 33:1 before the intervention; after 2 years in the trial, ratios were 9:1 in the experimental group and 21:1 among controls. The prevalence of coronary artery disease was 2% to 3% in rural areas of India and 9% to 14% in urban populations. The high incidence in urban areas is thought to be due to intake of Indian ghee or clarified butter (rich in cholesterol oxides) and high omega-6–to–omega-3 ratios.35,36
Figure 2.
The GISSI-Prevenzione trial (level I evidence)9,10 randomly assigned 11 324 patients surviving a recent MI into 4 groups: one took a capsule containing 850 mg/d of omega-3 fatty acids each day, another took 300 IU of vitamin E daily, a third group took both each day, and the control group took nothing. After 3.5 years, overall mortality was reduced by 20% and CV mortality was reduced by 30% in the group taking capsules of omega-3 fatty acids. No benefit was apparent from taking vitamin E alone. A 45% reduction in sudden cardiac death (P = .01) accounted for most of the benefit. Omega-3 fatty acids seem to be able to stabilize contractile heart cells electrically and thus prevent ventricular arrhythmias.23
A meta-analysis by Bucher et al11 (level I evidence) identified 11 trials published between 1966 and 1999 with a total of 7951 patients in intervention groups and 7855 in control groups. They found that intake of fish or fish oil reduced rates of overall mortality (P < .001), fatal MI (P < .001), and sudden cardiac death (P < .01). Mortality from coronary artery disease was reduced by 40% to 60% with consumption of 40 to 60 g of fish daily.
Several studies, including the Cardiovascular Health Study,37 the Family Heart Study,38 the Health Professionals Follow-up Study,39 the Multiple Risk Factor Intervention Trial,40 and the Nurses’ Health Study,41 showed benefit of ALA in CV disease. The Zutphen Elderly Study,42 however, found a modest link between ALA and increased risk of CV disease. Excessive consumption of trans fatty acids might have contributed to this.
Although most studies have shown that omega-3 fatty acids are useful for secondary prevention of CV disease, some have shown no statistical benefit. A study done by Nilsen et al12 (level I evidence) showed no benefit for prevention of further cardiac events in 300 patients from Norway. Those patients had significantly lower triglyceride levels (P < .0001) and significantly higher HDL levels (P < .0016) than most people. It is thought that no further benefit was possible among these people who already consumed a great deal of fish in their diet. This study was also shorter than many of the studies listed above.
Severe familial hypertriglyceridemia
Supplementation with omega-3 fatty acids has been shown to be of benefit in severe familial hypertriglyceridemia. Richter et al13 (level II evidence) demonstrated that adding 4.32 g/d of omega-3 fatty acids to the diet for 8 weeks reduced serum triglycerides from 18.29 to 10.1 mmol/L. Pschierer et al14 (level II evidence) showed that serum triglycerides had decreased significantly from 16.9 to 11.2 mmol/L after 1 month, and further decreased after 11 months to 10.1 mmol/L on average with supplementation with omega-3 fatty acids.
Fish oil and HMG-CoA reductase inhibitors
The effectiveness of statins can be improved by adding omega-3 fatty acids to the diet.43,44 A small study looked at combining statins and fish oil (level II evidence).15 Adding 900 to 1800 mg of EPA to the diet of patients already taking HMG-CoA reductase inhibitors resulted in a further decrease in total cholesterol from 5.63 to 5.02 mmol/L (P < .05) and in triglycerides from 2.07 to 1.08 mmol/L (P < .01). Serum HDL increased significantly from 1.23 to 1.34 mmol/L (P < .01).
Cardiovascular surgery
In a study done by Eritsland et al16 (level I evidence), 610 patients who underwent coronary artery bypass grafting were assigned to a fish-oil group (4 g/d of fish oil) or to a control group. The end point was patency of the graft at 1 year. A year later, vein graft occlusion was 27% in the experimental group and 33% in the control group (P = .034). Vein graft occlusion was inversely related to the relative change in serum omega-3 fatty acid levels. Initial studies done on coronary angioplasty patients45 showed that fish oil had promise for reducing recurring stenosis, but later studies using higher doses did not show any statistically significant reduction.46
Dietary suggestions, discussion, and recommendations
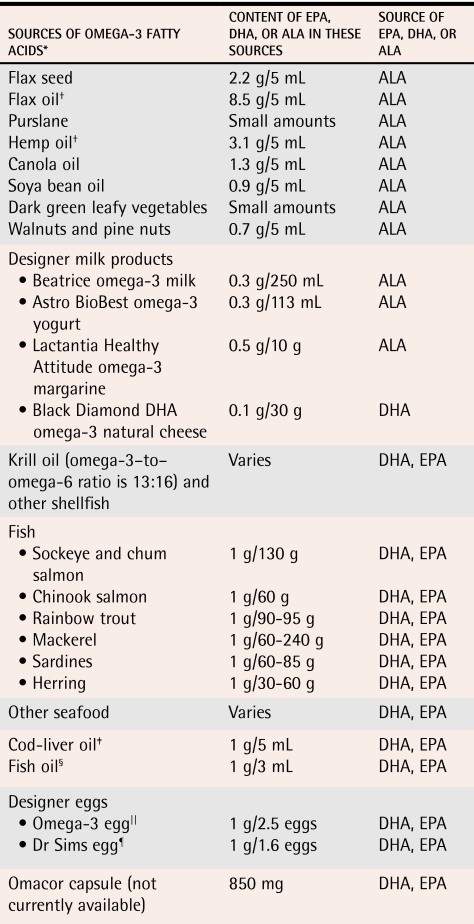
In 1990, Canada was the first country to provide separate dietary recommendations for omega-6 and omega-3 fatty acids for people of all ages.47 For adults between 25 and 49 years old, Health Canada suggests 1500 mg of omega-3 and 9000 mg of omega-6 polyunsaturates daily for men and 1100 mg of omega-3 and 7000 mg of omega-6 fatty acids daily for women. This results in an omega-6–to–omega-3 ratio of 6:1. It is thought that most Canadians do not have this modest daily intake of omega-3 fatty acids. Dietary sources of omega-3 fatty acids and some instructions for making them palatable are shown in Table 3.48 Side effects and interactions associated with consumption of fish oil are listed in Table 4.49-53
Table 3. Sources of omega-3 essential fatty acids.
To consume the minimum daily amount of 1200 mg of omega-3 fatty acids, people can choose a variety of food from the list in this table or take 3-4 fish oil capsules daily.
ALA—alpha-linolenic acid, DHA—docosahexaenoic acid, EPA—eicosapentenoic acid.
*Includes long-chain polyunsaturated fatty acids, EPA and DHA, and plant-source omega-3 fatty acid, ALA.
†Flax oil and hemp oil can be mixed into salad dressings and other food. These oils oxidize easily and should never be used for cooking.
‡Also a good source of vitamins A and D.
§Fish-oil flavours are milder in capsules, especially if capsules are swallowed cold from the refrigerator.
||Each designer omega-3 egg has 0.38 g of DHA and EPA (omega-6–to–omega-3 ratio is 1.6:1), 7 times as much vitamin E as, and less cholesterol than, a normal egg.
¶A Dr Sims designer egg has 0.6 g of DHA and EPA (omega-6–to–omega-3 ratio is 1:1). A normal egg has 0.05 g of DHA and EPA.
Data from Kris-Etherton et al.48
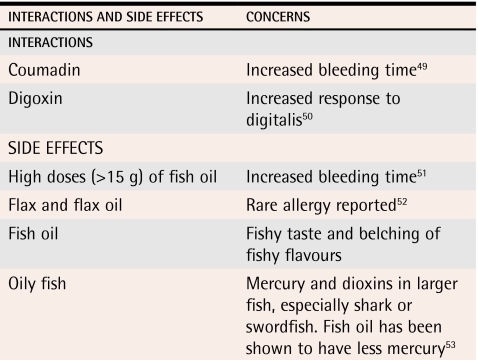
Table 4.
Fish-oil interactions and side effects
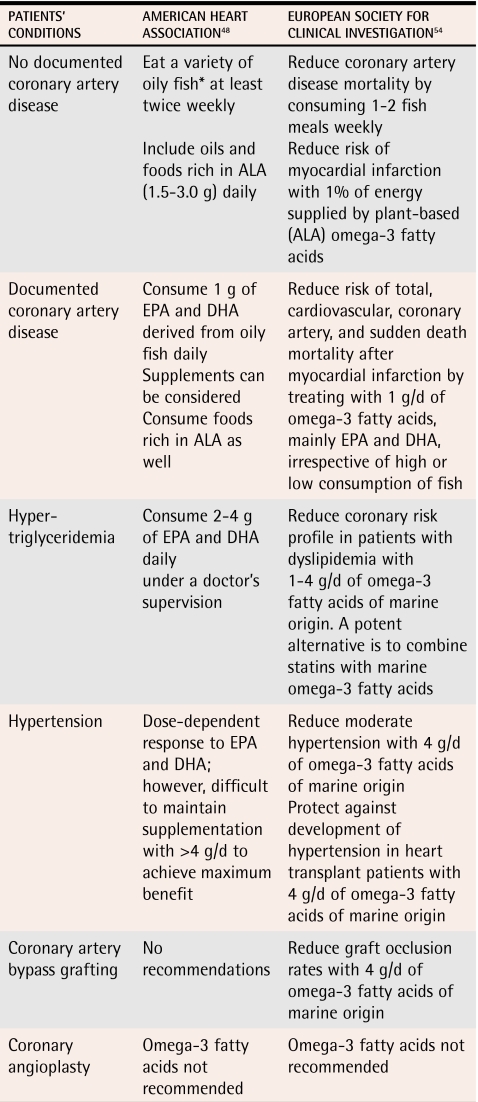
The American Heart Association issued new recommendations on consumption of omega-3 fatty acids in 2003.48 These are listed in Table 548,54 along with recommendations from an expert round-table discussion at the 34th Annual Scientific Meeting of the European Society for Clinical Investigation.54
Table 5.
Recommendations of the American Heart Association48 and the European Society for Clinical Investigation54 regarding consumption of omega-3 fatty acids
ALA—alpha-linolenic acid, DHA—docosahexaenoic acid, EPA—eicosapentenoic acid.
*Lean fish have smaller amounts of omega-3 fatty acids; fried fish (frozen breaded fish products or fish from fast-food outlets) have minimal amounts of omega-3 fatty acids
Conclusion
There is now solid evidence that omega-3 fatty acids favourably modulate disease processes, such as hypertension, coronary artery disease, and hypertriglyceridemia. Increasing dietary intake of omega-3 fatty acids and bringing the ratio of omega-3 to omega-6 fatty acids into a healthy balance would improve Canadians’ cardiovascular health.
Levels of evidence.
Level I: At least one properly conducted randomized controlled trial, systematic review, or meta-analysis
Level II: Other comparison trials, non-randomized, cohort, case-control, or epidemiologic studies, and preferably more than one study
Level III: Expert opinion or consensus statements
Biography
Dr Schwalfenberg is a family physician in full-time solo practice. He is a member of the Department of Family Practice at the Misericordia Hospital in Edmonton, Alta.
Footnotes
Competing interests: None declared
References
- 1.Geleijnse JM, Giltay EJ, Grobbee DE, Donders AR, Kok FJ. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens. 2002;20(8):1493–1499. doi: 10.1097/00004872-200208000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Appel LJ, Miller ER, III, Seidler AJ, Whelton PK. Does supplementation of diet with ‘fish oil’ reduce blood pressure? A meta-analysis of controlled clinical trials. Arch Intern Med. 1993;153(12):1429–1438. [PubMed] [Google Scholar]
- 3.Bang HO, Dyerberg J. Plasma lipids and lipoproteins in Greenlandic west coast Eskimos. Acta Med Scand. 1972;192(1-2):85–94. doi: 10.1111/j.0954-6820.1972.tb04782.x. [DOI] [PubMed] [Google Scholar]
- 4.Dyerberg J, Bang HO, Hjorne N. Fatty acid composition of the plasma lipids in Greenland Eskimos. Am J Clin Nutr. 1975;28(9):958–966. doi: 10.1093/ajcn/28.9.958. [DOI] [PubMed] [Google Scholar]
- 5.Dewailly E, Blanchet C, Gingras S, Lemieux S, Holub BJ. Cardiovascular disease risk factors and n-3 fatty acid status in the adult population of James Bay Cree. Am J Clin Nutr. 2002;76(1):85–92. doi: 10.1093/ajcn/76.1.85. [DOI] [PubMed] [Google Scholar]
- 6.Burr ML, Fehily AM, Gilbert JF, Rogers S, Holliday RM, Sweetnam PM, et al. Effects of changes in fat, fish, and fibre intakes on death and myocardial reinfarction: diet and reinfarction trial (DART). Lancet. 1989;2:757–761. doi: 10.1016/s0140-6736(89)90828-3. [DOI] [PubMed] [Google Scholar]
- 7.Leaf A. Dietary prevention of coronary heart disease: the Lyon Diet Heart Study. Circulation. 1999;99(6):733–735. doi: 10.1161/01.cir.99.6.733. [DOI] [PubMed] [Google Scholar]
- 8.Singh RB, Dubnov G, Niaz MJ, Ghosh S, Singh R, Rastogi SS, et al. Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients (Indo-Mediterranean Diet Heart Study): a randomised single-blind trial. Lancet. 2002;360(9344):1455–1461. doi: 10.1016/S0140-6736(02)11472-3. [DOI] [PubMed] [Google Scholar]
- 9.Stone NJ. The Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardio (GISSI)-Prevenzione Trial on fish oil and vitamin E supplementation in myocardial infarction survivors. Curr Cardiol Rep. 2000;2(5):445–451. doi: 10.1007/s11886-000-0059-5. [DOI] [PubMed] [Google Scholar]
- 10.Marchioli R, Schweiger C, Tavazzi L, Valagussa F. Efficacy of n-3 polyunsaturated fatty acids after myocardial infarction: results of GISSI-Prevenzione trial. Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto Miocardico. Lipids. 2001;36(Suppl):119–126. doi: 10.1007/s11745-001-0694-8. [DOI] [PubMed] [Google Scholar]
- 11.Bucher HC, Hengstler P, Schindler C, Meier G. N-3 polyunsaturated fatty acids in coronary heart disease: a meta-analysis of randomized controlled trials. Am J Med. 2002;112(4):298–304. doi: 10.1016/s0002-9343(01)01114-7. [DOI] [PubMed] [Google Scholar]
- 12.Nilsen DW, Albreksten G, Landmark K, Moen S, Aarsland T, Woie L. Effects of a high-dose concentrate of n-3 fatty acids or corn oil introduced early after an acute myocardial infarction on serum triacylglycerol and HDL cholesterol. Am J Clin Nutr. 2001;74(1):50–56. doi: 10.1093/ajcn/74.1.50. [DOI] [PubMed] [Google Scholar]
- 13.Richter WO, Jacob BG, Ritter MM, Schwandt P. Treatment of primary chylomicronemia due to familial hypertriglyceridemia by omega-3 fatty acids. Metabolism. 1992;41(10):1100–1105. doi: 10.1016/0026-0495(92)90293-j. [DOI] [PubMed] [Google Scholar]
- 14.Pschierer V, Richter WO, Schwandt P. Primary chylomicronemia in patients with severe familial hypertriglyceridemia responds to long-term treatment with (n-3) fatty acids. J Nutr. 1995;125(6):1490–1494. doi: 10.1093/jn/125.6.1490. [DOI] [PubMed] [Google Scholar]
- 15.Nakamura N, Ohta M, Okuda K, Urakazi M, Sawazaki S, Yamazaki K, et al. Joint effects of HMG-CoA reductase inhibitors and eicosapentaenoic acids on serum lipid profile and plasma fatty acid concentrations in patients with hyperlipidemia. Int J Clin Lab Res. 1999;29(1):22–25. doi: 10.1007/s005990050057. [DOI] [PubMed] [Google Scholar]
- 16.Eritsland J, Arnesen H, Gronseth K, Fjeld NB, Abdelnoor M. Effect of dietary supplementation with n-3 fatty acids on coronary artery bypass graft patency. Am J Cardiol. 1996;77(1):31–36. doi: 10.1016/s0002-9149(97)89130-8. [DOI] [PubMed] [Google Scholar]
- 17.Lichtenstein AH, Kennedy E, Barrier P, Danford D, Ernst ND, Grundy SM, et al. Dietary fat consumption and health. Nutr Rev. 1998;56(5 Pt 2):3–19. doi: 10.1111/j.1753-4887.1998.tb01728.x. [DOI] [PubMed] [Google Scholar]
- 18.Simopoulos AP. The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomed Pharmacother. 2002;56(8):365–379. doi: 10.1016/s0753-3322(02)00253-6. [DOI] [PubMed] [Google Scholar]
- 19.Connor WE. Importance of n-3 fatty acids in health and disease. Am J Clin Nutr. 2000;71(1 Suppl):171–175. doi: 10.1093/ajcn/71.1.171S. [DOI] [PubMed] [Google Scholar]
- 20.Simopoulos AP. Human requirement for N-3 polyunsaturated fatty acids. Poult Sci. 2000;79(7):961–970. doi: 10.1093/ps/79.7.961. [DOI] [PubMed] [Google Scholar]
- 21.Simopoulos AP. Omega-3 fatty acids in health and disease and in growth and development. Am J Clin Nutr. 1991;54(3):438–463. doi: 10.1093/ajcn/54.3.438. [DOI] [PubMed] [Google Scholar]
- 22.De Gomez Dumm IN, Brenner RR. Oxidative desaturation of alpha-linoleic, linoleic, and stearic acids by human liver microsomes. Lipids. 1975;10(6):315–317. doi: 10.1007/BF02532451. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberg IH. Fish—food to calm the heart. N Engl J Med. 2002;346(15):1102–1103. doi: 10.1056/NEJM200204113461502. [DOI] [PubMed] [Google Scholar]
- 24.Harris WS. Are omega-3 fatty acids the most important nutritional modulators of coronary heart disease risk? Curr Atheroscler Rep. 2004;6(6):447–452. doi: 10.1007/s11883-004-0085-7. [DOI] [PubMed] [Google Scholar]
- 25.Mori TA, Beilin LJ, Burke V, Morris J, Ritchie J. Interactions between dietary fat, fish, and fish oils and their effects on platelet function in men at risk of cardiovascular disease. Arterioscler Thromb Vasc Biol. 1997;17(2):279–286. doi: 10.1161/01.atv.17.2.279. [DOI] [PubMed] [Google Scholar]
- 26.Thies F, Garry JM, Yaqoob P, Rerkasem K, Williams J, Shearman CP, et al. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomised controlled trial. Lancet. 2003;361(9356):477–485. doi: 10.1016/S0140-6736(03)12468-3. [DOI] [PubMed] [Google Scholar]
- 27.Heller A, Koch T. Schmeck K, van Ackem K. Lipid mediators in inflammatory disorders. Drugs. 1998;55(4):487–496. doi: 10.2165/00003495-199855040-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao G, Etherton TD, Martin KR, West SG, Gillies PJ, Kris-Etherton PM. Dietary alpha-linolenic acid reduces inflammatory and lipid cardiovascular risk factors in hypercholesterolemic men and women. J Nutr. 2004;134(11):2991–2997. doi: 10.1093/jn/134.11.2991. [DOI] [PubMed] [Google Scholar]
- 29.Fleischhauer FJ, Yan WD, Fischell TA. Fish oil improves endothelium-dependent coronary vasodilation in heart transplant recipients. J Am Coll Cardiol. 1993;21(4):982–989. doi: 10.1016/0735-1097(93)90357-7. [DOI] [PubMed] [Google Scholar]
- 30.Harris WS. Fish oils and plasma lipid and lipoprotein metabolism in humans: a critical review. J Lipid Res. 1989;30(6):785–807. [PubMed] [Google Scholar]
- 31.Calabresi L, Villa N, Canavesi M, Sirtori CR, James RW, Bernini F, et al. An omega-3 polyunsaturated fatty acid concentrate increases plasma high-density lipoprotein 2 cholesterol and paraoxonase levels in patients with familial combined hyperlipidemia. Metabolism. 2004;53(2):153–158. doi: 10.1016/j.metabol.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 32.Herrmann W, Biermann J, Kostner GM. Comparison of effects of N-3 to N-6 fatty acids on serum level of lipoprotein(a) in patients with coronary artery disease. Am J Cardiol. 1995;76(7):459–462. doi: 10.1016/s0002-9149(99)80130-1. [DOI] [PubMed] [Google Scholar]
- 33.Din JN, Newby DE, Flapan AD. Omega 3 fatty acids and cardiovascular disease—fishing for a natural treatment. BMJ. 2004;328(7430):30–35. doi: 10.1136/bmj.328.7430.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Lorgeril M, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999;99(6):779–785. doi: 10.1161/01.cir.99.6.779. [DOI] [PubMed] [Google Scholar]
- 35.Pella D, Dubnov G, Singh RB, Sharma R, Berry EM, Manor O. Effects of an Indo-Mediterranean diet on the omega-6/omega-3 ratio in patients at high risk of coronary artery disease: the Indian paradox. World Rev Nutr Diet. 2003;92:74–80. doi: 10.1159/000073793. [DOI] [PubMed] [Google Scholar]
- 36.Jacobson MS. Cholesterol oxides in Indian ghee: possible cause of unexplained high risk of atherosclerosis in Indian immigrant populations. Lancet. 1987;2(8560):656–658. doi: 10.1016/s0140-6736(87)92443-3. [DOI] [PubMed] [Google Scholar]
- 37.Lemaitre RN, King IB, Mozaffarian D, Kuller LH, Tracy RP, Siscovick DS. n-3 Polyunsaturated fatty acids, fatal ischemic heart disease, and nonfatal myocardial infarction in older adults: the Cardiovascular Health Study. Am J Clin Nutr. 2003;77(2):319–325. doi: 10.1093/ajcn/77.2.319. [DOI] [PubMed] [Google Scholar]
- 38.Ellison RC; National Heart, Lung, and Blood Institute Family Heart Study. Djousse L, Folsom AR, Province MA, Hunt SC. Dietary linolenic acid and carotid atherosclerosis: the National Heart, Lung, and Blood Institute Family Heart Study. Am J Clin Nutr. 2003;77(4):819–825. doi: 10.1093/ajcn/77.4.819. [DOI] [PubMed] [Google Scholar]
- 39.Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. BMJ. 1996;313(7049):84–90. doi: 10.1136/bmj.313.7049.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dolecek TA. Epidemiological evidence of relationships between dietary polyunsaturated fatty acids and mortality in the Multiple Risk Factor Intervention Trial. Proc Soc Exp Biol Med. 1992;200(2):177–182. doi: 10.3181/00379727-200-43413. [DOI] [PubMed] [Google Scholar]
- 41.Hu FB, Stampfer MA, Manson JE, Rimm EB, Wolk A, Colditz GA, et al. Dietary intake of alpha-linolenic acid and risk of fatal ischemic heart disease among women. Am J Clin Nutr. 1999;69(5):890–897. doi: 10.1093/ajcn/69.5.890. [DOI] [PubMed] [Google Scholar]
- 42.Oomen CM, Ocke MC, Feskens EJ, Kok FJ, Kromhout D. Alpha-Linolenic acid intake is not beneficially associated with 10-y risk of coronary artery disease incidence: the Zutphen Elderly Study. Am J Clin Nutr. 2001;74(4):457–463. doi: 10.1093/ajcn/74.4.457. [DOI] [PubMed] [Google Scholar]
- 43.Das UN. Essential fatty acids as possible mediators of the actions of statins. Prostaglandins Leukot Essent Fatty Acids. 2001;65(1):37–40. doi: 10.1054/plef.2001.0285. [DOI] [PubMed] [Google Scholar]
- 44.Nakamura N, Hamazaki T, Jokaji H, Minami S, Kobayashi M. Effect of HMG-CoA reductase inhibitors on plasma polyunsaturated fatty acid concentrations in patients with hyperlipidemia. Int J Clin Lab Res. 1998;28(3):192–195. doi: 10.1007/s005990050043. [DOI] [PubMed] [Google Scholar]
- 45.Dehmer GJ, Popma JJ, van den Berg EK, Eichhom EJ, Prewitt JB, Campbell WB, et al. Reduction in the rate of early restenosis after coronary angioplasty by a diet supplemented with n-3 fatty acids. N Engl J Med. 1988;319(12):733–740. doi: 10.1056/NEJM198809223191201. [DOI] [PubMed] [Google Scholar]
- 46.Johansen O, Brekke M, Seljeflot I, Abdelnoor M, Arnesen H. N-3 fatty acids do not prevent restenosis after coronary angioplasty: results from the CART study. Coronary Angioplasty Restenosis Trial. J Am Coll Cardiol. 1999;33(6):1619–1626. doi: 10.1016/s0735-1097(99)00054-6. [DOI] [PubMed] [Google Scholar]
- 47.Scientific Review Committee. Nutritional recommendations. (Document H49-42/1990E). Ottawa, Ont: National Health and Welfare Canada; 1990. [Google Scholar]
- 48.Kris-Etherton PM, Harris WS, Appel LJ. Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2003;23(2):20–30. doi: 10.1161/01.atv.0000038493.65177.94. [DOI] [PubMed] [Google Scholar]
- 49.Buckley MS, Goff AD, Knapp WE. Fish oil interaction with warfarin. Ann Pharmacother. 2004;38(1):50–52. doi: 10.1345/aph.1D007. [DOI] [PubMed] [Google Scholar]
- 50.Bernard M, Gerbi A, Barbey O, Jamme I, Cozzone PJ, Maixent JM. Dietary fish oil promotes positive inotropy and efficiency of digitalis. Lipids. 1999;34(Suppl):195. doi: 10.1007/BF02562286. [DOI] [PubMed] [Google Scholar]
- 51.Eritsland J, Arnesen H, Seljeflot I, Kierulf P. Long-term effects of n-3 polyunsaturated fatty acids on haemostatic variables and bleeding episodes in patients with coronary artery disease. Blood Coagul Fibrinolysis. 1995;6(1):17–22. doi: 10.1097/00001721-199502000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Lezaun A, Fraj J, Colas C, Duce F, Dominguez MA, Cuevas M, et al. Anaphylaxis from linseed. Allergy. 1998;53(1):105–106. doi: 10.1111/j.1398-9995.1998.tb03785.x. [DOI] [PubMed] [Google Scholar]
- 53.Foran SE, Flood JG, Lewandrowski KB. Measurement of mercury levels in concentrated over-the-counter fish oil preparations: is fish oil healthier than fish? Arch Pathol Lab Med. 2003;127(12):1603–1605. doi: 10.5858/2003-127-1603-MOMLIC. [DOI] [PubMed] [Google Scholar]
- 54.Nordoy A, Marchioli R, Arnesen H, Videbaek J. n-3 polyunsaturated fatty acids and cardiovascular diseases. Lipids. 2001;36(Suppl):127–129. doi: 10.1007/s11745-001-0695-7. [DOI] [PubMed] [Google Scholar]