Abstract
OBJECTIVE
To compare family physicians’ reports of their experiences managing patients with psychiatric disorders in settings with and without access to collaborative mental health services.
DESIGN
Survey using a questionnaire adapted from a similar study in Australia. Family physicians were asked about their knowledge, skills, and degree of comfort in managing the following psychiatric disorders derived from the primary care version of the 10th edition of the International Classification of Diseases: psychosis, depression, anxiety, childhood disorders, and stress-related disorders. We also compared the 2 groups of physicians regarding their satisfaction with mental health services in general.
SETTING
The Capital District Health Authority (CDHA) in Nova Scotia.
PARTICIPANTS
All family physicians practising in the CDHA.
MAIN OUTCOME MEASURES
Self-reported knowledge, skills, and degree of comfort in managing psychiatric problems; satisfaction with mental health services, adjusted for family physicians’ demographics; and stated interest in mental health.
RESULTS
We received 101 responses (37 from physicians with access to collaborative care and 64 from physicians without access) from 7 communities in the CDHA. Family physicians who had access to collaborative care reported significantly greater knowledge in the areas of psychosis, alcohol or substance use, and childhood behavioural problems; and better skills in managing psychosis, alcohol or substance use, childhood depression or anxiety, childhood behavioural disorders, and relationship problems. Their comfort levels in managing relationship problems and childhood behavioural disorders were also significantly higher. Family physicians with access to collaborative care were significantly more satisfied with mental health services, over and above shared care. All these differences remained significant after controlling for sex, level of interest in mental health, and years in practice.
CONCLUSION
Family physicians with access to collaborative care reported greater knowledge, better skills, and more comfort in managing psychiatric disorders and greater satisfaction with mental health services. Further work is needed to establish why this is so and to determine any effect on patient outcomes, such as symptoms, quality of life, and psychosocial functioning.
Abstract
OBJECTIF
Comparer les rapports des médecins de famille sur leurs expériences du traitement des patients souffrant de troubles psychiatriques, selon qu’ils ont accès ou non à des services de soins de santé mentale en collaboration.
TYPE D’ÉTUDE
Questionnaire adapté d’une étude australienne similaire. On interrogeait les médecins sur leurs connaissances, habiletés et degré de confort concernant le traitement de patients souffrant des troubles psychiatriques suivants, tirés de la 10e édition de la Classification internationale des maladies, psychoses, dépression, anxiété, troubles de l’enfance et conditions reliées au stress. On a également comparé la satisfaction des 2 groupes de médecins de famille à l’égard des services de santé mentale en général.
CONTEXTE
Le Capital District Health Authority (CDHA) de Nouvelle-Écosse.
PARTICIPANTS
Tous les médecins de famille exerçant au sein de la CDHA.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Auto-évaluation des connaissances, des habiletés et du degré de confort concernant le traitement des problèmes psychiatriques; satisfaction à l’égard des services de santé mentale, ajustée en fonction des caractéristiques démographiques des participants et de leur intérêt déclaré pour la santé mentale.
RÉSULTATS
Nous avons reçu 101 réponses (37 médecins ayant accès à des services en collaboration et 64 n’y ayant pas accès) de 7 collectivités servies par la CDHA. Ceux qui avaient accès à des soins en collaboration déclaraient avoir une connaissance considérablement meilleure des psychoses, de l’alcoolisme et de la toxicomanie, et des troubles de comportement des enfants, et être plus habiles et à l’aise pour traiter ces troubles et la dépression, l’anxiété ainsi que les problèmes relationnels. Les médecins ayant accès aux soins en collaboration rapportaient un degré de satisfaction considérablement plus élevé à l’égard des services de santé psychiatriques, abstraction faite des soins partagés. Toutes ces différences demeuraient significatives après corrections en fonction du sexe, du niveau d’intérêt pour la santé mentale et des années de pratique des répondants.
CONCLUSION
Les médecins de famille ayant accès à des soins en collaboration déclaraient avoir des connaissances et des habiletés plus grandes, se disaient plus à l’aise de traiter les troubles psychiatriques, et rapportaient plus de satisfaction à l’égard des services de santé mentale. D’autres études seront nécessaires pour établir les raisons de cette situation et pour déterminer les effets éventuels sur les résultats pour les patients, dont les symptômes, la qualité de vie et le fonctionnement psychosocial.
EDITOR’S KEY POINTS.
This study in Nova Scotia compares physicians’ knowledge, skills, and comfort in managing psychiatric patients; and the satisfaction with mental health services among physicians who have formal collaboration with mental health teams and physicians who do not.
The collaborative model allowed family doctors better access to mental health workers, including psychiatrists, nurses, social workers, and psychologists. Twice-yearly educational meetings were also part of the package.
For most diagnoses, physicians reported greater knowledge, skills, and comfort when they were involved in collaborative care, and these physicians were more satisfied with mental health services. The findings remained true after controlling for sex, level of interest in mental health, and years in practice.
POINTS DE REPÈRE DU RÉDACTEUR.
Cette étude néo-écossaise compare les connaissances, les habiletés et le degré de confort des médecins de famille concernant le traitement des patients souffrant de troubles psychiatriques ainsi que la satisfaction à l’égard des services de santé mentale des médecins qui ont, ou qui n’ont pas, l’occasion de collaborer avec une équipe de santé mentale.
Les médecins travaillant en collaboration avaient un meilleur accès aux professionnels de la santé mentale, y compris les psychiatres, les infirmières, les travailleurs sociaux et les psychologues. Le programme comprenait des séances de formation bisannuelles.
Pour la majorité des diagnostics, les médecins travaillant en collaboration déclaraient posséder plus de connaissances et d’habiletés, et être plus à l’aise; ils se disaient aussi plus satisfaits des services de santé mentale. Ces résultats demeuraient vrais corrections faites quant au sexe des participants, à leur niveau d’intérêt pour la santé mentale et à leurs années de pratique.
There is growing interest in collaboration between family physicians and mental health professionals, as up to 40% of patients seen in primary care have mental health problems.1,2 Family physicians were the sole sources of mental health care for 35% of respondents in the Ontario Mental Health Survey.3 The severity and duration of patients’ problems managed in primary care are similar to those of patients’ in specialized care.4
Studies of collaborative care have reported contradictory results because of variations in case mix, setting, and interventions.5-7 Approaches to collaborative care have ranged from improved communication between primary care and specialist services,5 through “shifted outpatient” models involving psychiatrists,6 to consultation-liaison models involving multidisciplinary teams.7
Because of difficulties in measuring patient outcomes, some studies use proxy measures, such as changes in family practitioners’ knowledge and practice. When using these measures, it is important to adjust for confounders, such as demographics and years in practice.7 There have been several qualitative studies of shared mental health care in Canada8,9 and 1 quantitative study of family physicians’ overall satisfaction with mental health services, which did not control for possible confounding.3
We compared the self-reported knowledge, skills, and comfort of family physicians with access to collaborative care and family physicians without access to collaborative care. We used multivariate analyses to control for confounders. We also compared the 2 groups’ satisfaction with mental health services in general.
METHOD
Setting
We evaluated collaborative care in the Capital District Health Authority (CDHA), which covers 40% of Nova Scotia’s population and includes Halifax and surrounding rural areas. The program involves 46 family physicians in 10 clinics and offers a consultation-liaison service for mental health care of children and adolescents as well as adults. The program focuses on clinics serving socially deprived areas and populations less likely to gain access to mental health services. The service includes liaison with shelters, hostels, and drop-in centres.
Three clinics volunteered to participate in the program 7 years ago, and more joined as resources allowed, including 2 clinics in rural sites. No clinics have refused to participate in the program, and we plan to include all clinics in the CDHA eventually. Working arrangements are covered by memorandums of understanding between the collaborative care program and each clinic that covers referral, documentation, charting, and administrative support.
The 18 participating mental health professionals (psychiatrists, nurses, social workers, and psychologists) are mostly part-time, combining collaborative duties with outpatient work. Each clinic has a long-term working relationship with 1 or 2 mental health professionals who have office space at the site. Patients are referred either directly for clinical care or indirectly through consultation, education, or case conferencing. Areas covered include diagnosis, medication, and management. Mental health professionals can offer a maximum of 6 face-to-face sessions, if required, and facilitate referrals to specialist services if these 6 sessions are insufficient. Patients’ reports, summaries, and investigation results remain on their charts at the primary care practices.
There is an orientation program for mental health workers who join the service, which includes shadowing existing collaborative care workers. There are also educational retreats every 6 months for both primary care teams and mental health professionals.
Design and sample
We evaluated the effect of collaborative care on physicians’ self-reported knowledge, skills, and comfort in managing mental health problems, as well as their satisfaction with mental health services in general. We also documented any informal arrangements physicians had outside the program.
We used a questionnaire derived from a similar study done in Australia by one of the authors (S.K.)7 to conduct a pilot study with 15 physicians at 3 sites, 2 sites with access to collaborative care and 1 site without.10 We then faxed the questionnaire to all family physicians in the CDHA. We followed this with a mailing that was included in newsletters sent by the CDHA’s primary care program to all family physicians. There were no exclusion criteria. This paper includes findings from both the pilot and subsequent larger study.
Survey instrument
We collected data on participants’ sex, age, and length of time practising in Nova Scotia. We asked about knowledge, skills, and comfort in managing the following psychiatric disorders derived from the primary care version of the 10th edition of the International Classification of Diseases (ICD-10)11: psychosis, depression, anxiety, drug or alcohol use, personality disorders, sexual disorders, eating disorders, and adjustment disorders. We also asked about managing relationship problems. This gave a total of 33 items. By knowledge we meant theoretical and experiential learning, by skills we meant the practical application of knowledge to management of psychiatric problems, and by comfort we meant the level of ease with which physicians undertake management.7 We provided these descriptions on the survey form. We asked participants to rate their knowledge, skills, and comfort on a 4-point Likert scale (0—none, 1—minimum, 2—moderate, 3—high). We also collected information on referrals to, and satisfaction with, mental health services over and above collaborative care. We again used a 4-point Likert scale ranging from strongly disagree to strongly agree. Unlike the Australian study, we included childhood disorders and services for children and adolescents among the mental health conditions.7
The Australian study had indicated that this survey form was acceptable and feasible and that differences in self-reported knowledge, skills, and comfort were associated with differences in referral behaviour of physicians with access, and physicians without access, to collaborative care.7 Our pilot study confirmed that the survey form was acceptable and feasible to use in Canada.10
Analysis strategy and sample-size estimation
We used forward stepwise logistic regression to control for possible confounding variables (eg, demographic factors and interest in mental health) associated with provision of mental health services, knowledge of psychiatry, or participation in collaborative care.7,12,13 We assessed significance using the likelihood ratio statistic, which has a chi-square distribution with 1 df.
As the Australian study showed a 30% difference in knowledge, skills, and comfort between the 2 groups,7 power calculations indicated we needed at least 94 subjects (ie, approximately 47 in each group) to have an 80% chance of detecting a statistically significant difference with 95% confidence. The study design was approved by the Research Ethics Board of the Capital District Health Authority.
RESULTS
Demographic characteristics of the sample
We received 101 responses: 37 from physicians with access to formal collaborative care and 64 from physicians without such access from the following communities in the CDHA: Halifax, Hubbards, Westphal, Bedford-Sackville, Hantsport, Fall River, and Middle Musquodoboit. We identified 272 family physicians from the Nova Scotia College of Physicians and Surgeons’ register as practising in those 7 communities,14 giving an overall response rate of 37.1%. The response rate from physicians who had access to formal collaborative care was much higher, at approximately 80% (37/46).
Given the low response rate of the physicians without access to collaborative care, we compared their demographics with those of physicians on the College register. As the survey was anonymous, this was the only way of checking how representative our sample of family practitioners was. Of the 272 physicians identified from the register, 157 (57.7%) were male and 115 (42.3%) were female. This was not significantly different from our sample (52.4% male and 47.6% female) (chi-square = 0.54, df = 1, P = .46). Mean years in practice was 21.5 (standard deviation [SD] 9.6) in our sample and 20.9 among the 272 physicians identified from the register. The 95% confidence interval for the mean of our sample was 19.1 to 23.9, suggesting there was no statistically significant difference between the 2 groups. Average age of physicians in the register was 39.9 years (range 30 to 51, SD 6.45). Professional experience ranged from 1 to 52 years, with an average of 19.5 years (SD 9.9).
Among our 101 participants, 41 (40.4%) were men and 60 (59.6%) were women. Physicians who had access to collaborative care were overwhelmingly female (81%) (Table 1). A further 16 physicians (15.8%) had access to informal collaborative care (56% men and 44% women). This meant that, although they did not participate in the collaborative care program, they had close working relationships with mental health professionals. Private psychiatrists were most frequently mentioned. There were insufficient numbers to analyze these doctors more fully, but we conducted a sensitivity analysis of our results to see whether there were differences when we excluded them from comparisons between physicians involved in formal collaborative care and controls. For the rest of this paper, collaborative care will mean formal, as opposed to informal, arrangements, unless otherwise stated.
Table 1.
Characteristics of family physicians with and without access to collaborative mental health care
We also investigated the relationship between demographic factors and self-reported experience in managing psychiatric disorders. We divided years of practice into a dichotomous variable about the median (19 years). We also divided scores for knowledge, skills, and comfort about the value of 2, as this was the median for 21 of the 33 survey items. Physicians with fewer years in practice (33/57) were more than twice as likely to be comfortable dealing with eating disorders as those with more years in practice (16/44) were (95% confidence interval 1.1 to 5.0). No other demographic factors were associated with knowledge, skills, or comfort.
Access to collaborative care
Family physicians with access to collaborative care were more likely to be female, were significantly younger than the mean age, and had significantly fewer years in practice (Table 1). Ninety (90%) participants had at least a moderate interest in psychiatry, and there was no statistically significant difference between collaborative-care and control groups in this area.
Participants in both groups reported more knowledge, skills, and comfort in dealing with adults with depression or anxiety and adjustment disorders than in dealing with teenagers with the same disorders (Tables 2, 3, and 4).
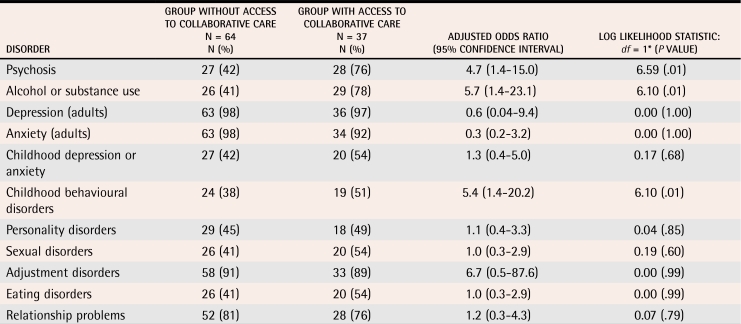
Table 2.
Self-reported knowledge about managing psychiatric disorders of family physicians with and without access to collaborative mental health care
*Adjusted for sex, years in practice, and level of interest in mental health care.
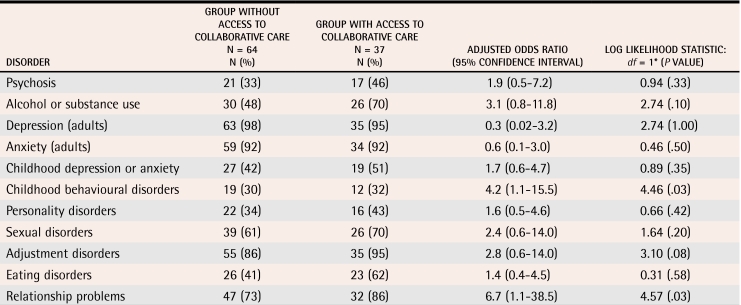
Table 3.
Self-reported skills for managing psychiatric disorders of family physicians with and without access to collaborative mental health care
*Adjusted for sex, years in practice, and level of interest in mental health care.
Table 4.
Self-reported comfort in managing psychiatric disorders of family physicians with and without access to collaborative mental health care
*Adjusted for sex, years in practice, and level of interest in mental health care.
We then compared differences in self-reported knowledge, skills, and comfort among physicians who had access to collaborative care with those among physicians who did not. We adjusted the odds ratios to control for physicians’ sex, years in practice, and level of interest in psychiatry because our previous study suggested that these could act as confounders in our analysis.6
Physicians who had access to collaborative care reported significantly greater knowledge in the areas of psychosis, alcohol or substance use, and childhood behavioural problems, such as attention deficit hyperactivity disorder and conduct disorders (Table 2). They also reported better skills for managing psychosis, alcohol or substance use, childhood depression or anxiety, childhood behavioural disorders, and relationship problems (Table 3). They were also significantly more comfortable in managing relationship problems and childhood behavioural disorders (Table 4). Our results remained the same when we conducted a sensitivity analysis to see whether excluding family practitioners with informal collaborative care arrangements from the comparison between those with formal collaborative care and controls would make any difference.
Satisfaction with services
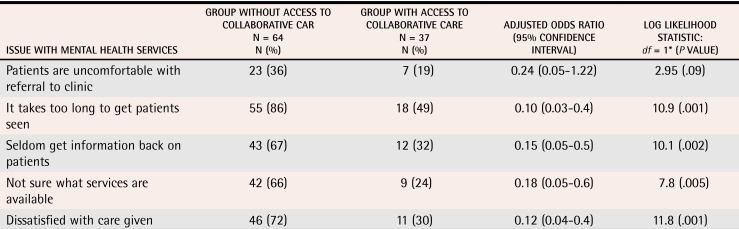
We again divided the scores about the value of 2, as this was the median score for most items in this area. Only four (4%) of 101 participants were uncomfortable referring patients to mental health services, although 30 (29.7%) thought that patients were uncomfortable with being referred. More than half the physicians (51%) were not sure what services were available, and 17 (16.8%) were unsure about how to make a referral to the services of which they were aware. Three quarters thought that waiting lists were too long, and 57 (56.4%) were generally dissatisfied with mental health services. There were no significant differences in participants’ views on services for adults and for children and adolescents, other than more physicians being unsure how to make referrals for children and adolescents (chi-square 4.3, df 1, P = .04).
Table 5 shows that physicians with access to collaborative care were less likely to think waiting lists were too long or communication insufficient, to express uncertainty about the availability of services, or otherwise to be dissatisfied. In this analysis, we again controlled for sex, years in practice, and level of interest in mental health.
Table 5.
Levels of satisfaction with mental health services of physicians with and without access to collaborative mental health care
*Adjusted for sex, years in practice, and level of interest in mental health care.
DISCUSSION
To our knowledge, this is the first study in Canada to assess the association between collaborative care and self-reported knowledge, skills, and comfort in managing psychiatric disorders, and satisfaction with mental health services. The participation rate of physicians who were involved in collaborative care was acceptable (80%); it was considerably lower for those who did not have such involvement. Sex and years in practice of control physicians did not differ significantly from those of possible respondents identified from the register. We also adjusted for sex, years in practice, and level of interest in psychotherapy.
As in the Australian study,7 sex was not associated with greater self-reported knowledge, skills, or comfort. Other work suggests that female physicians are more likely to provide mental health services.13
Physicians involved in collaborative care in Nova Scotia had greater knowledge and skills in management of psychosis and alcohol or substance use, rather than in adult depression or anxiety, as in the Australian study.7 This finding also contrasts with the general focus on anxiety or depression in the shared-care literature.9,15,16 Explanations for this could include our program’s focus on marginalized communities or the fact that physicians had sufficient prior experience to be comfortable in dealing with anxiety and depression, and so only required assistance with psychosis and drug or alcohol use. Support for this idea comes from the high levels of knowledge, skills, and comfort in managing adult depression or anxiety reported by physicians, regardless of their access to collaborative care. We could clarify this further only by assessing knowledge, skills, and comfort before the introduction of collaborative care.
It was encouraging to see that physicians involved in collaborative care reported they had greater knowledge, skills, and comfort in dealing with childhood disorders, especially behavioural conditions. This could be because they have more contact with mental health professionals from child and adolescent services. The Australian shared-care service covered only adults.7
Our other main finding was that physicians with access to collaborative care were significantly more satisfied with mental health services generally, over and above collaborative care. This echoes reports from Ontario and suggests that collaborative care informs and helps physicians in their referrals to specialist services.3
Shared-care arrangements, therefore, can complement educational initiatives, which might be important, given that the effectiveness of large continuing education workshops is unclear.2 Collaboration might also address possible selection bias by involving physicians who choose continuing education on topics other than mental health, but still look after patients with psychiatric disorders.
Limitations
We have no information on physicians’ knowledge of or interest in mental health care before the introduction of collaborative care, so we had to rely on retrospective information. Our sample might have been subject to selection bias, since physicians with an interest in mental health care might have been more likely to respond to our survey. Use of self-reported measures could have introduced information bias. Our study might have been underpowered to detect important differences between groups in areas where our findings failed to reach statistical significance. To preserve physicians’ anonymity, we did not collect information on practice size or other characteristics. The study shows only an association between access to collaborative care and self-reported knowledge, skills, and comfort in managing mental health issues, not cause and effect. These findings, however, can complement evaluation of referral patterns where modest changes in physicians’ behaviour are also found.17-20
Conclusion
Participants with access to collaborative care reported greater knowledge, skills, and comfort in managing psychiatric disorders, even after controlling for possible confounders (such as demographics and interest in psychiatry). Being involved in collaborative care also appeared to enhance physicians’ satisfaction with mental health services overall.
Acknowledgments
We thank the Capital District Health Authority’s Shared and Primary Care Program for their support in developing and promoting collaborative care and for logistical support in evaluation of the program. We also thank the physicians who participated in the evaluation.
Biographies
Dr Kisely is Head of the Department of Community Health and Epidemiology at Dalhousie University in Halifax, NS, and is Medical Director of the Shared Care Program at the Capital District Health Authority.
Dr Duerden is Team Leader of Primary Medical Services at the Capital District Mental Health Program.
Ms Shaddick is Health Services Manager at Shared Care and Cole Harbour/Eastern Community Mental Health.
Dr Jayabarathan is Medical Director of Cowie Hill and Camp Hill Family Medicine Centres.
Footnotes
Competing interests: None declared
References
- 1.Kates N, Craven C, Bishop J, Clinton T, Kraftcheck D, LeClair K, et al. Shared mental health care in Canada. Position paper no. 1997-38. Ottawa, Ont: Canadian Psychiatric Association and College of Family Physicians of Canada; 1997. [Google Scholar]
- 2.Kates N. Shared mental health care. The way ahead [editorial]. Can Fam Physician. 2002;48:853. 853-5 [Eng],859-61 [Fr] [PMC free article] [PubMed] [Google Scholar]
- 3.Kates N, Fugere C, Farrar S. Family physician satisfaction with mental health services: findings from a community survey. CPA Bull. 2004;36:10–14. [Google Scholar]
- 4.Lesage AD, Goering P, Lin E. Family physicians and the mental health system. Report from the Mental Health Supplement to the Ontario Health Survey. Can Fam Physician. 1997;43:251–256. [PMC free article] [PubMed] [Google Scholar]
- 5.Fitzpatrick NK, Shah S, Walker N, Nourmand S, Tyrer PJ, Barnes TR, et al. The determinants and effect of shared care on patient outcomes and psychiatric admissions—an inner city primary care cohort study. Soc Psychiatry Psychiatr Epidemiol. 2004;39:154–163. doi: 10.1007/s00127-004-0721-0. [DOI] [PubMed] [Google Scholar]
- 6.Carr VJ, Faehrmann C, Lewin TJ, Walton JM, Reid AA. Determining the effect that consultation-liaison psychiatry in primary care has on family physicians’ psychiatric knowledge and practice. Psychosomatics. 1997;38:217–229. doi: 10.1016/S0033-3182(97)71458-0. [DOI] [PubMed] [Google Scholar]
- 7.Kisely S, Horton-Hausknecht J, Tait A, Bostwick R, Wong P, Miller K, et al. Does increased collaboration between primary care and psychiatric services change GPs’ practice? A controlled trial. Aust Fam Physician. 2002;31:587–589. [PubMed] [Google Scholar]
- 8.Lucena RJ, Lesage A. Family physicians and psychiatrists. Qualitative study of physicians’ views on collaboration. Can Fam Physician. 2002;48:923–929. [PMC free article] [PubMed] [Google Scholar]
- 9.Brown JB, Lent B, Stirling A, Takhar J, Bishop J. Caring for seriously mentally ill patients. Qualitative study of family physicians’ experiences. Can Fam Physician. 2002;48:915–920. [PMC free article] [PubMed] [Google Scholar]
- 10.Kisely S, Jayabarathan A. Can shared care change self-reported skills in managing psychiatric disorders? In: 5th National Conference on Shared Mental Health Care. 2004 Program. Hamilton, Ont: Hamilton HSO Mental Health and Nutrition Program; 2004. [cited 2006 June 13]. p. 20. Available from: http://www.shared-care.ca/bc_conference.shtml. [Google Scholar]
- 11.World Health Organization. Diagnostic and management guidelines for mental disorders in primary care. ICD-10, chapter V, primary care version. Gottingen, Ger: Hogrefe and Hubler; 1996. [Google Scholar]
- 12.Hickie IB, Davenport TA, Naismith SL, Scott EM, Hadzi-Pavlovic D, Koschera A. Treatment of common mental disorders in Australian general practice. Med J Aust. 2001;175(Suppl):25–30. doi: 10.5694/j.1326-5377.2001.tb143786.x. [DOI] [PubMed] [Google Scholar]
- 13.Hickie IB, Davenport TA, Naismith SL, Scott EM. Conclusions about the assessment and management of common mental disorders in Australian general practice. Med J Aust. 2001;175(Suppl):52–55. doi: 10.5694/j.1326-5377.2001.tb143791.x. [DOI] [PubMed] [Google Scholar]
- 14.Nova Scotia College of Physicians and Surgeons. Search physician listing. Halifax, NS: Nova Scotia College of Physicians and Surgeons; 2005. [cited 8 June 2005]. Available at: http://www.cpsns.ns.ca/ [Google Scholar]
- 15.Wilkinson G. The role of primary care physicians in the treatment of patients with long-term mental disorders. Int Rev Psychiatry. 1991;3:35–42. [Google Scholar]
- 16.Katon W, Gonzales J. A review of randomized trials of psychiatric consultation-liaison studies in primary care. Psychosomatics. 1994. 268–78. [DOI] [PubMed]
- 17.Warner RW, Gater R, Jackson MG, Goldberg DP. Effects of a community mental health service on the practice and attitudes of general practitioners. Br J Gen Pract. 1993;43:507–511. [PMC free article] [PubMed] [Google Scholar]
- 18.Bower P, Sibbald B. Do consultation-liaison services change the behaviour of primary care providers? A review. Gen Hosp Psychiatry. 2000;22:84–96. doi: 10.1016/s0163-8343(00)00058-x. [DOI] [PubMed] [Google Scholar]
- 19.Bower P, Sibbald B. On-site mental health workers in primary care: effects on professional practice. Cochrane Database Syst Rev. 2000. CD000532. [DOI] [PubMed]
- 20.Bower P, Sibbald B. Systematic review of the effect of on-site mental health professionals on the clinical behaviour of general practitioners. BMJ. 2000;320:614–617. doi: 10.1136/bmj.320.7235.614. [DOI] [PMC free article] [PubMed] [Google Scholar]