Abstract
Evidence suggests that social and economic factors are important determinants of health. Yet, despite higher poverty rates, less education, and worse access to health care, health outcomes of many Hispanics living in the United States today are equal to, or better than, those of non-Hispanic whites. This paradox is described in the literature as the epidemiological paradox or Hispanic health paradox. In this paper, the authors selectively review data and research supporting the existence of the epidemiological paradox. They find substantial support for the existence of the epidemiological paradox, particularly among Mexican Americans. Census undercounts of Hispanics, misclassification of Hispanic deaths, and emigration of Hispanics do not fully account for the epidemiological paradox. Identifying protective factors underlying the epidemiological paradox, while improving access to care and the economic conditions among Hispanics, are important research and policy implications of this review.
Keywords: Hispanic Americans, Hispanic health paradox, socioeconomic status, health status, review
Ever-increasing evidence suggests that the health of a population is greatly determined by the social and economic circumstances of that population, as well as its access to health care services.1–6 Yet, for many Hispanics living in the United States today, health outcomes are equal to, or better than, those of non-Hispanic whites, despite higher poverty rates, less education, and worse access to health care. This paradox has been described in the literature as the epidemiological paradox or Hispanic health paradox.7–8 In this paper, we selectively review data and research supporting the existence of a Hispanic health paradox. The paper is broadly organized into three main sections: (1) a review of indicators of social, economic, and behavioral determinants of health for Hispanics in the United States, including a brief review of the demographics of Hispanics in the United States; (2) a review of indictors of health outcomes among Hispanics in the United States; and (3) a review of some potential alternative explanations to the existence of a Hispanic health paradox, focusing on potential biases in national data sets. The paper concludes with a discussion of policy implications derived from the information reviewed.
Demographics and socioeconomic status of Hispanics
Hispanics constitute one of the fastest-growing racial/ethnic groups in the United States. According to results from the 2000 census, the number of Hispanics in the United States has increased by nearly 60 percent in the last decade, from 23 million in 1990 to 35.3 million in 2000.9 By 2050, Hispanics are expected to number 97 million and account for nearly one-quarter of the U.S. population.10
High fertility rates, high levels of immigration from Latin America, and high ethnic attribution rates* are the principal factors accounting for the growth of the Hispanic population.11 Although immigration has been an important factor in the growth of the Hispanic population, because of the high fertility rate among Hispanics (almost double that of non-Hispanic whites [whites]), the number of Hispanics would continue to increase significantly even if all immigration from Latin America were to cease. The Hispanic population would double by 2050 even in the absence of immigration.11
High levels of immigration from Latin America have created a large foreign-born and Spanish-speaking Hispanic population in the United States. According to the 1997 Current Population Survey (CPS), more than one-third of all Hispanics are foreign-born. Among the principal Hispanic subgroups in the Untied States, more than one-third of Mexican Americans (Mexicans) and two-thirds of Cuban Americans (Cubans) and South and Central Americans are foreign-born.12 Among foreign-born Hispanics, as many as 98 percent report speaking primarily Spanish at home, while only 24 percent report speaking English very well. Among foreign-born Hispanics living in the United States three or fewer years, 82 percent report speaking English not well or not well at all.13
Estimates derived from the 1997 CPS indicate that Mexicans are the largest subgroup of Hispanics in the United States, accounting for 63 percent of the U.S. Hispanic population.12 Puerto Ricans* are the next largest subgroup, accounting for 11 percent of the U.S. Hispanic population, followed by Cubans, who account for just more than 4 percent of the U.S. Hispanic population.12 Central and South Americans, who comprise people of multiple national backgrounds, account for 14 percent of the U.S. Hispanic population, while the remaining 7 percent of U.S. Hispanics are of other national backgrounds, including Spanish, or are of unknown origin.
On average, the socioeconomic status of Hispanics is comparable with that of African Americans and significantly lower than that of non-Hispanic whites. This situation is reflected in most measures of socioeconomic status, including personal and family income, poverty rates, educational attainment, and occupation. In 1997, for example, 26 percent of Hispanic and African American families lived in poverty, compared with 7 percent of white families (Table 1).12 While the median family income for all Americans was $42,299, the median income for Hispanic families was $26,178 (1996 dollars).
TABLE 1.
SELECTED DEMOGRAPHIC AND SOCIOECONOMIC CHARACTERISTICS OF HISPANICS
|
HISPANIC SUBGROUPS |
||||||
|---|---|---|---|---|---|---|
| RISK FACTOR (PERCENTAGE) | NON-WHITE | HISPANIC | MEXICAN | PUERTO RICAN | CUBAN | SOUTH/CENTRAL AMERICAN |
| Age (years) | ||||||
| < 20 | 27 | 39 | 42 | 41 | 20 | 34 |
| 20–44 | 37 | 42 | 42 | 38 | 37 | 47 |
| 45–64 | 22 | 14 | 12 | 16 | 23 | 16 |
| > 64 | 14 | 5 | 4 | 5 | 21 | 4 |
| Sex | ||||||
| Male | 51 | 51 | 52 | 52 | 53 | 51 |
| Female | 49 | 49 | 48 | 48 | 47 | 49 |
| Marital statusa | ||||||
| Married | 59 | 54 | 56 | 46 | 57 | 52 |
| Never married | 24 | 36 | 35 | 39 | 24 | 39 |
| Widowed/divorced | 17 | 10 | 9 | 15 | 19 | 9 |
| Educationb | ||||||
| Less than high school | 14 | 45 | 51 | 39 | 35 | 37 |
| High school graduate or more | 86 | 55 | 49 | 61 | 65 | 63 |
| Bachelor’s degree or more | 26 | 10 | 7 | 9 | 19 | 15 |
| Family income ($)c | 47,022 | 26,178 | 25,347 | 23,646 | 35,616 | 29,960 |
| Poverty | ||||||
| Families in poverty | 7 | 26 | 28 | 33 | 13 | 19 |
| Occupationd | ||||||
| High risk/low social status | 48 | 74 | 77 | 68 | 53 | 68 |
| Low risk/high social status | 52 | 26 | 23 | 32 | 47 | 32 |
Source: U.S. Census Bureau. Hispanic Population in the U.S., Current Population Survey, March, 1997. Available at http://www.census.gov/population/www/socdemo/hispanic/ho97.html.
For persons age 15 years and older.
For persons age 25 years and older.
Median family income in 1996.
Employed male persons age 16 years and older.
The occupation categories reported in the CPS can be divided into high–health risk/low–social position occupations and low–health risk/high–social position occupations.14 Low-risk/high–social position occupations include both managerial and professional occupations and technical, sales, and administrative support occupations, while high-risk/low–social position occupations include service occupations; precision production, craft, and repair occupations; operators, fabricators, and laborers; and farming, forestry, and fishing occupations. According to this taxonomy, Hispanics were disproportionately represented in high-risk/low–social position occupations. For example, in 1997, 74 percent of Hispanics held high-risk/low–social position occupations, compared with 48 percent of whites.12
Socioeconomic status varies significantly among Hispanic subgroups. Generally, Mexicans and Puerto Ricans are the worst off, while Cubans and South and Central Americans are the best off. In 1997, the median family income was highest for Cubans, followed by Mexicans and Puerto Ricans; the poverty rate was greatest among Puerto Rican families (33 percent), followed by Mexican families (28 percent), South and Central American families (19 percent), and Cuban families (13 percent).12 Educational attainment, as the proportion of the population to go beyond high school, was greatest among Cubans (65 percent), followed by South and Central Americans (63 percent), Puerto Ricans (61 percent), and Mexican Americans (49 percent).12 Rates of occupation in high-risk/low-status occupations were highest among Mexicans (77 percent), Puerto Ricans (68 percent), and South and Central Americans (68 percent), and lowest among Cubans (53 percent).12
Although we have presented data aggregated for all South and Central Americans, this group is composed of multiple nationality groups, with some groups relatively more disadvantaged than others. Recent Central American refugees from El Salvador and Guatemala, for example, are at particularly high socioeconomic risk. According to Lopez, only 28 percent of Salvadorans and 30 percent of Guatemalans had completed high school, and less than 5 percent of either group reported graduating from college.15
Behavioral risk factors
Low socioeconomic status is associated with unhealthy behaviors or lifestyles among Hispanics. For example, among Hispanic women, health-related behaviors such as smoking cigarettes, being overweight, and being physically inactive are more common among persons with a lower socioeconomic status than among those with a higher socioeconomic status (Figure 1).
FIGURE 1.
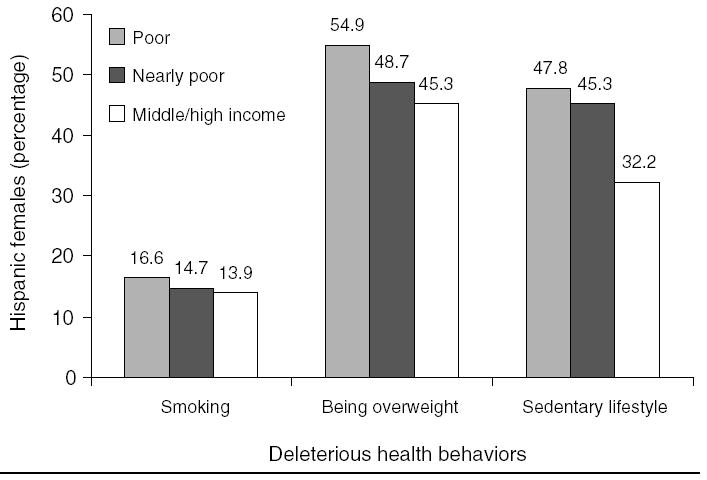
ASSOCIATIONS BETWEEN SOCIOECONOMIC STATUS AND DELETERIOUS HEALTH BEHAVIORS AMONG HISPANIC WOMEN
Among Hispanics, however, acculturation* is significantly associated with health-related behaviors. During the acculturation process, individuals are thought to relinquish the behavioral norms of their culture of origin while adopting those of another.16 Thus, for immigrants to the United States, the acculturation process can have either a positive or negative effect on the frequency of a particular behavior, depending on the frequency of that behavior in the acculturating person’s culture of origin and in U.S. culture. For example, if smoking were more frequent among men from a particular culture than among men in the United States, then the acculturation process would have a positive health effect (decreased smoking) on men from that culture. On the other hand, if smoking were less common among men from a particular culture than among men in the United States, then the acculturation process would have a negative health effect (increased smoking) on men from that culture. As we will see, the effects of acculturation frequently differ between men and women and among Hispanic subgroups.
Most studies of smoking rates among Hispanics and whites find that Hispanic women smoke less than Hispanic men, that Hispanic women smoke less than white women, and that Hispanic men smoke the same or more than white men.17 As predicted by acculturation theory, the rates of smoking among Hispanics and whites converge as acculturation increases. For example, research on Mexican and Central American women has found that smoking was more prevalent among more acculturated women than among less acculturated women, and that the smoking prevalence among more acculturated Hispanic women was similar to that of white women.18 The same study found that smoking was less common among more acculturated men than among less acculturated men, and that the prevalence of smoking among more acculturated Hispanic men was similar to that of white men. Less is known about the association between smoking and acculturation among Puerto Ricans and Cubans.
Smoking rates also vary among Hispanic subgroups (Figure 2). A recent comprehensive review of smoking among ethnic minorities by the surgeon general19 found that white (29 percent) and Mexican (29 percent) men had the highest smoking rates, followed by Puerto Rican men (23 percent) and Cuban men (26 percent). Among women, Puerto Ricans (23 percent) had the highest smoking rate, followed by whites (22 percent), Cubans (18 percent), and Mexicans (15 percent).
FIGURE 2.
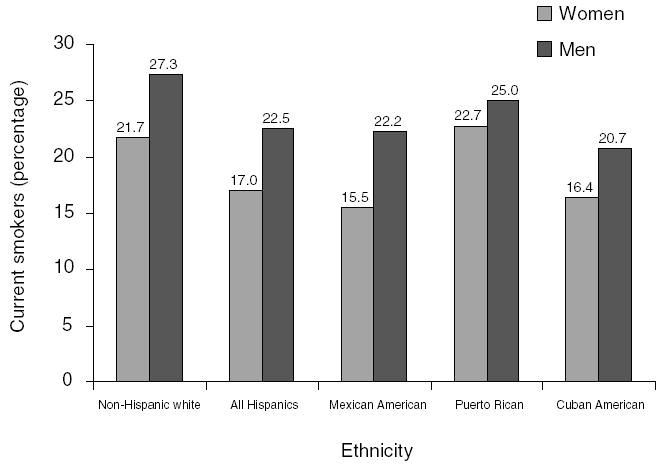
SMOKING RATES AMONG HISPANIC SUBGROUPS BY GENDER SOURCE
Relatively less research has been done on the dietary habits of Hispanics. However, existing research suggests that Hispanics consume similar or smaller amounts of total energy (calories) than whites20–22 and that the composition of Hispanic diets differs from that of whites. In several studies, Hispanics were found to consume a greater percentage of carbohydrates, protein, and fiber, and a lower percentage of total and saturated fat than non-Hispanics.20–23 Based on these and other findings, researchers have suggested that Hispanics are closer to meeting national cholesterol education program guidelines than are whites.20
Hispanic diets also differ by level of acculturation. Although the effects of acculturation on diet are mixed, overall, acculturation appears to have negative effects on the diet of Hispanics.24,25 In one study of younger Mexican American women (ages 19–44), use of traditional foods was found to decrease after immigration to the United States and as time progressed (i.e., second-generation women reported consuming fewer traditional foods than first-generation ones).26 This change in diet incorporated both positive (decreased use of lard, cream, and sausage; increased use of milk and salads) and negative (decreased use of homemade fruit juices and vegetable soup; increased use of butter, margarine, vegetable oil, mayonnaise, and cookies) trends. On balance, however, the authors concluded the changes were more negative than positive.
Other studies have found that less acculturated Hispanics consume more fiber, more fats, and more carbohydrates than more acculturated Hispanics27 and that first-generation Mexican American women have higher average intakes of protein, vitamins A and C, folate, and calcium than second-generation women.23 Yet another study found that less acculturated Hispanics were also more likely to eat fruits, rice, beans, meat, and fried foods and to drink whole milk than are more acculturated Hispanics.28
Diets also differ among the Hispanic subgroups. In one of the few studies to examine differences in dietary intake by Hispanic subgroup, Loria et al.20 found the following:
Carbohydrate intake was higher among Puerto Ricans and Cubans than Mexicans
Protein intake was similar among the three groups
Total fat and saturated fat intake was similar among Puerto Ricans and older Cubans (age 65+), but higher among Mexicans
Cholesterol intake was highest among Puerto Ricans and younger Cubans
The authors concluded that older Puerto Ricans and Cubans met the population guidelines for reducing chronic disease risk for more micronutrients than any other group. However, the authors of another study of Hispanic diets concluded that Puerto Ricans have less balanced diets than Cubans or Mexicans.24
Generally, alcohol consumption among Hispanics is lower than among whites. However, drinking patterns vary among Hispanic subgroups and between genders. Among all Hispanic subgroups, men are more likely to drink and to drink more heavily than women.29 Among Hispanic men, Mexicans have a higher rate of heavy drinking than Puerto Ricans, who, in turn, have a higher rate than Cubans do. Mexicans have the highest rates of abstention among Hispanic women, as well as the highest rate of heavy drinking, while Puerto Rican women have the lowest rate of abstention.
Acculturation is an important factor in the growing rates of alcohol problems among Hispanics.29 Among Hispanic women, acculturation is associated with a steady decrease in the rate of abstention and a steady increase in the rate of drinking, with the highest rates of drinking occurring among more acculturated and more educated Hispanic women.30 Higher rates of heavy drinking have also been found among older Hispanic women, supporting the hypothesis that traditional sanctions against drinking are negatively influenced by acculturation.31 Among Hispanic men, the influence of acculturation on drinking is less clear. Some researchers have found that acculturation is associated with higher drinking rates,28,30 while others have found that it has no association with drinking rates.25
One of the most important health problems facing Hispanics today is obesity. Being overweight is a risk factor for a number of medical conditions including hypertension; dyslipidemia; type 2 diabetes mellitus; coronary heart disease; stroke; gallbladder disease; osteoarthritis; sleep apnea; and endometrial, breast, prostrate, and colon cancers.32 According to the National Center for Health Statistics, 40 percent of Mexican men and 52 percent of Mexican women are overweight. In comparison, 34 percent of white men and 33 percent of white women are overweight.33 Earlier data from the Hispanic Health and Nutrition Examination Survey (1982–84) indicate that Mexican Americans have higher proportions of overweight men and women than Puerto Ricans and Cubans, a greater percentage of Puerto Rican women are overweight than Cuban women, and a greater percentage of Cuban men are overweight than Puerto Rican men.34
Other studies have found that Mexicans are less likely to report avoidance of sugar or practice dieting behavior than whites. Furthermore, Mexicans were more likely than whites to agree with the statement, “Americans are too concerned about weight loss,” which suggests to the authors of this study that Mexicans have not fully accepted the American ideal of leanness.35
Physical activity, like diet, is closely linked to being overweight. Generally, Hispanics lead more sedentary lifestyles than whites. Data from the National Health and Nutrition Examination Survey III and the National Health Interview Survey indicate that 37 percent of Hispanic women (age 18+) and 30 percent of Hispanic men (age 18+) engage in no leisure time physical activity, compared with 25 percent of white women and 20 percent of white men.36 In a smaller study of primarily Mexican and Central American Hispanics and whites in San Francisco, 40 percent of men and 46 percent of women reported a sedentary lifestyle, compared with 17 percent of white men and 23 percent of white women.18 These findings were further corroborated by results from the San Luis Valley Diabetes Study, which also found that Hispanics were less physically active than whites.37 Studies of school-age children have found that Hispanic children exercise less than white children, suggesting that there may be cultural factors accounting for the low physical activity levels observed among Hispanic adults.36
Access to, and use of, health care services
Access to care refers to the degree to which individuals and groups are able to obtain appropriate health care from the medical care system in a timely fashion. Numerous studies have documented that Hispanics lack sufficient access to health services for a number of reasons, such as financial barriers, structural barriers, and personal barriers to care. Financial barriers include inadequate or lack of health insurance and low personal income. Structural barriers include organizational barriers to care, poor geographic access to providers, and lack of transportation to and from providers. Personal barriers to care include cultural and linguistic factors. Given the demographic and economic characteristics of the Hispanic populations residing in the United States, it is not surprising that Hispanics face significant barriers to obtaining care.
Medical insurance is among the most important determinants of access to care. Using data from the Hispanic Health and Nutrition Examination Survey, Estrada et al.38 found that cost was one of the most frequently mentioned factors preventing Mexican Americans from using health care services. Similarly, Schur et al.39 reported on the importance of health insurance among Hispanic populations in predicting a number of indicators of access to care, including having a usual source of care, use of physician visits, and blood pressure screening.
Lack of health insurance is a significant access problem for Hispanics. Nationally, Hispanic adults younger than 65 are substantially more likely to be uninsured than white adults. In 1997, 37 percent of Hispanic nonelderly adults lacked any health care coverage, compared with 24 percent of blacks and 14 percent of whites.40 Among Hispanic subgroups, nonelderly Central and South Americans (42 percent) were most likely to be uninsured, followed by Mexicans (39 percent), Cubans (21 percent), and Puerto Ricans (21 percent).40
The lower uninsured rates among Puerto Ricans have been attributed to greater reliance on public assistance and Medicaid coverage.41 In 1996, 34 percent of Puerto Ricans obtained Medicaid or other public assistance coverage, compared with 19 percent of Mexicans and 14 percent of Cubans.33 Other explanations for the higher Medicaid coverage rates among Puerto Ricans include (1) the high proportion of poor Puerto Rican families that are headed by women and thus are more likely to be Medicaid eligible, given that many states exclude two-parent families regardless of income criteria, and (2) the fact that Puerto Ricans tend to live in states where Medicaid eligibility rules are less restrictive (New York and New Jersey), whereas Cubans and Mexicans tend to live in states where Medicaid eligibility rules are more restrictive (Florida and Texas).39
Uninsured rates among the foreign-born are high. On the basis of the 1989 and 1990 National Health Interview Survey, Thamer et al.42 reported that, overall, 41 percent of foreign-born Hispanics were uninsured, compared with 13 percent of the total U.S. population. Thamer et al. also found that uninsured rates varied by length of time in the United States. For 1989 and 1990, 70 percent of foreign-born Hispanics who had lived in the United States for less than 1 year were uninsured, compared with 62 percent of those who had lived in the United States from 1 to 4 years, 53 percent of those who had lived in the United States for 5 to 9 years, 44 percent of those who had lived in the United States for 10 to 14 years, and 26 percent of those who had lived in the United States for 15 or more years.42 During the same time period, 25 percent of U.S.-born Hispanics were uninsured.
Lack of insurance coverage among Hispanic children is also high. In 1997, 29 percent of Hispanic children younger than 18 were uninsured, compared with 19 percent of black children and 11 percent of white children.43 Furthermore, the risk of being uninsured increased with low socioeconomic status. Based on 1994–95 data, the uninsured rate increased from 7.2 percent among high-income Hispanic children to 33 percent among poor Hispanic children.32 Many Hispanic families who are eligible for Medicaid do not enroll. In a study of 817 poor inner-city Hispanic parents and their children, Halfon et al. found that while most of the children were eligible for Medicaid (84 percent), a substantial proportion (39.3 percent) had episodic or no coverage during their lifetime.44 The Children’s Health Insurance Program, enacted in 1997, may be reducing the numbers of uninsured Hispanic children, although early reports show low enrollment rates among those eligible.45
Geographic proximity and transportation stand out among the list of structural barriers faced by Hispanics. Data from the Hispanic Established Population for Epidemiological Studies of the Elderly showed that older Mexican Americans are much less likely to drive than whites.46 Foreign-born Mexican American women in particular tend to rely on family for their transportation needs.47 For many families, however, working-age adults who drive may not be able to take time from work to provide transportation for adults who do not drive. In many rural areas and low-income parts of central cities, public transportation services are inadequate or completely lacking, making access to medical care by alternative means difficult or impossible.
The geographic distribution of providers also makes using health care services difficult for Hispanic patients as few providers, especially physicians, locate their practices in Hispanic communities.48 In a survey of physicians across California, communities with high proportions of black and Hispanic residents were four times as likely as communities with high proportions of white residents to have a shortage of physicians, regardless of income.49 Moreover, the extreme shortage of Hispanic health care professionals creates additional barriers to care because Hispanic physicians are more likely than other physicians to care for Hispanic and uninsured patients.49
A significant number of Hispanic patients face language barriers when seeking medical care. Language becomes particularly critical when Spanish-speaking patients encounter medical providers who do not speak Spanish and who do not have professional interpreters available.50 In the 1990 U.S. census, more than 95 percent of Mexicans, Cubans, and Salvadorans reported speaking Spanish at home and, of these individuals, 74 percent of Mexicans, 63 percent of Cubans, and 75 percent of Salvadorans reported speaking English poorly.51
Because patient-provider communication is central to the health care delivery process, poor communication resulting from language barriers has implications for the quality and outcomes of care. For example, poor patient-provider communication may lead to inappropriate medical testing in an attempt to establish a diagnosis in the absence of an adequate medical history. Spanish-speaking patients who receive unclear explanations about taking prescribed medications may take them inappropriately, resulting in treatment that is suboptimal, regardless of whether the prescriptions were technically appropriate. Morales et al. found that Spanish-speaking patients were significantly less satisfied than English-speaking patients with explanations given them about prescribed medication.52 Other research has also found that language concordance between Spanish-speaking patients and their provider results in better health outcomes than the lack thereof.53
Cultural factors may also contribute to the barriers faced by Hispanics seeking medical care. For example, medical care providers unfamiliar with the Hispanic culture may not recognize the importance of family in making treatment decisions or in discharge planning.54 Cross-cultural miscommunication may occur when a Hispanic patient mistakenly perceives impersonal professional behavior for lack of interest or when a physician, unfamiliar with Hispanic patients, perceives Hispanics to be superstitious, present oriented, noncompliant, or uninterested in preventive exams.55
Several studies show that Hispanics tend to use medical care services at similar or lower rates than whites and that variability in use exists among Hispanic subgroups. On the basis of the 1987 Medical Expenditure Panel Survey, Kominski and Pourat56 found that Hispanics were less likely to report a physician visit in the prior year than whites, even after taking into account insurance status. Using data from the National Health Interview Survey, Trevino and Moss found that 33 percent of Mexican Americans reported no physician contact in the prior year, compared with 20 percent of Puerto Ricans, 23 percent of Cuban Americans, and 23 percent of whites.57 Based on a recent nationally representative study, Hispanics were found to use preventive care and hospital care at lower rates than whites.58 Other studies have reached similar conclusions regarding the low use of care among Hispanics and the variations among the Hispanic subgroups.59
Using data from the 1980–91 National Health Interview Survey, Flores et al.60 found differences in health care utilization among Hispanic children. Seventy-four percent of Mexican children had visited a physician in the previous year, compared with 78 percent of Cuban children and 87 percent of Puerto Rican children. The range for the other major ethnic groups studied (Native American, black, Asian/Pacific, and white) was 78 percent to 84 percent. Puerto Rican children had the largest mean number of physician visits per year (3.9), compared with 3.4 for whites, 2.4 for Mexican and black children, and 2.3 for Asian/Pacific Islander children. The mean number of physician visits for all Hispanic children was 2.8.60
In a recent literature review of access to health services among Hispanics, Giachello concluded that
Hispanics under-use health and mental health services. Overall, for example, they are less likely to see a physician, to be hospitalized within a year, or to use preventive health services. Among subgroups, however, Puerto Ricans and Cubans report the highest use of formal medical care while Mexicans report the lowest. And Hispanic women report higher use of preventive services than Hispanic men but lower use of mental health care.41
Health status
According to most government statistics, the health of Hispanics is quite favorable relative to other U.S. racial/ethnic groups, whether one looks at life expectancy, adult mortality, or infant mortality (Figure 3).
FIGURE 3.
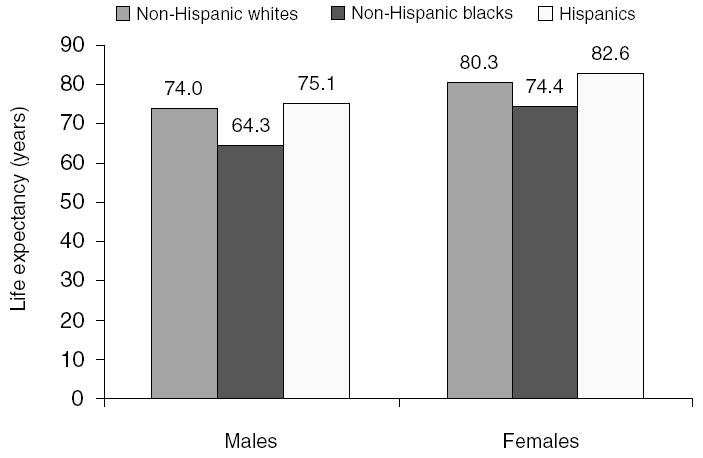
LIFE EXPECTANCY BY RACE AND HISPANIC ETHNICITY
The projected 1999 life expectancy at birth for Hispanic men and women was 75.1 years and 82.6 years, respectively. In comparison, the projected life expectancy for white men and women was 74.0 and 80.3 years, respectively.10 Similarly, the 1995 age-adjusted, all-cause mortality rate for the Hispanic population (386.8 per 100,000) was 18 percent below that of whites (475.2 per 100,000).61 Infant mortality for Hispanics (6.1 per 1,000 live births) also compared favorably with that of whites (6.3 per 1,000 live births).61
Although overall mortality rates for Hispanics and whites are comparable, differences emerge in disease-specific mortality rates (Table 2). For heart disease, which was the leading cause of death for both whites and Hispanics, Hispanics had an age-adjusted mortality rate of 88.6 (per 100,000) compared with a rate of 131.0 for whites. Similarly, age-adjusted mortality rates due to cerebrovascular disease, malignant neoplasms, chronic obstructive pulmonary disease, pneumonia and influenza, and suicide were higher among whites than among Hispanics. Conversely, age-adjusted mortality rates due to chronic liver disease, HIV/AIDS, unintentional injuries, and homicide and legal interventions were higher among Hispanics than among whites. Interestingly, HIV/AIDS and homicide and legal intervention were among the 10 leading causes of death for Hispanics, but not for whites, while suicide and Alzheimer’s disease were among the 10 leading causes of death for whites, but not for Hispanics.62
TABLE 2.
AGE-ADJUSTED MORTALITY RATES AMONG WHITES AND HISPANICS
| CAUSE-SPECIFIC MORTALITY RATE (PER 100,000) | HISPANICS | WHITES |
|---|---|---|
| Diseases of the heart | 88.6 | 131.0 |
| Cerebrovascular disease | 19.5 | 24.4 |
| Malignant neoplasms | 77.8 | 127.6 |
| Respiratory | 15.4 | 40.2 |
| Colorectal | 7.3 | 12.1 |
| Prostate | 9.9 | 13.6 |
| Breast | 12.8 | 20.1 |
| COPD | 8.9 | 22.1 |
| Pneumonia and influenza | 9.7 | 12.2 |
| Chronic liver disease | 12.6 | 6.7 |
| Diabetes mellitus | 18.8 | 11.5 |
| HIV/AIDS | 16.3 | 6.0 |
| Unintentional injuries | 49.0 | 29.3 |
| Suicide | 6.1 | 12.0 |
| Homicide and legal intervention | 12.4 | 3.5 |
Source: National Center for Health Statistics. Health, United States, 1998. With socioeconomic status and health chartbook. Hyattsville, MD: National Center for Health Statistics, 1998.
Note: COPD = Chronic obstructive pulmonary disease.
Significant variations in adult and infant mortality exist among the Hispanic subgroups. According to 1995 vital statistics, overall age-adjusted mortality was lowest among Mexicans (362.4 per 100,000), followed by Cubans (387.4 per 100,000) and Puerto Ricans (582.9 per 100,000).61 Infant mortality was lowest for Cubans (5.1 per 1,000 live births), followed by Mexicans (6.1 per 1,000 live births) and Puerto Ricans (8.6 per 1,000 live births). In comparison, white and African American overall age-adjusted mortality rates were 475.2 and 783.6, respectively, and the infant mortality rates were 6.3 per 1,000 live births and 15 per 1,000 live births, respectively.61
Results from the 1992–1995 National Health Interview Survey63 suggest that there is significant variation in self-reported health even after adjusting for differences in age distributions among Hispanics subgroups. For example, approximately 21 percent of Puerto Ricans reported limitations in daily activities* compared with 15 percent of Cubans and Mexicans. Cubans reported an average of three days per year lost from school or work compared with six days for Mexicans and Puerto Ricans. Mexicans fared better than Puerto Ricans on other measures such as restricted activity days, bed disability days, and hospitalizations.64
In a structured review of the published literature on the relationship between low birth weight (LBW) and Latino ethnicity, Fuentes-Afflick and Lurie found that LBW rates for Latinos and whites are comparable. This unexpected favorable outcome for Latinos masks the notably elevated LBW rates in Puerto Ricans.65
Fewer data are available on the health of foreign-born Hispanics. However, the existing data suggest that foreign-born Hispanics, U.S.-born Hispanics, and non-Hispanics may differ with respect to health. Using data from the National Health Interview survey, Liao et al. found that the relative risk of death was lowest among foreign-born Hispanics, followed by U.S.-born Hispanics and then whites.66 In addition, they found that the relative risk of dying among foreign-born Hispanics who had lived in the United States for less than 15 years was 23 percent to 45 percent lower than that of those who had lived in the United States for 15 years or more. Wei et al., using data from a cohort living near the Mexican border, found that sex- and age-adjusted mortality rates for native-born Mexican Americans (5.7 per 1,000 person years) exceeded those of non-Hispanic whites (3.8 per 1,000 person years) and foreign-born Mexican Americans (3.6 per 1,000 person years).67
Research based on self-reported health suggests that the health of recent immigrants may be better than that of earlier arrivals (Figure 4). Using data from the 1989 and 1990 National Health Interview Survey, Stephen et al.68 found that the percentage of foreign-born Hispanics reporting fair or poor health (on a scale ranging from excellent to poor), the percentage of foreign-born Hispanics reporting four or more bed days in the prior year, and the percentage of foreign-born Hispanics reporting activity limitations due to chronic conditions or impairments increased with duration of residence in the United States.68 Stephen et al. also found that, independent of duration of residence in the United States, the proportion of foreign-born Hispanics reporting poor or fair health as opposed to good health decreased as educational attainment increased.
FIGURE 4.
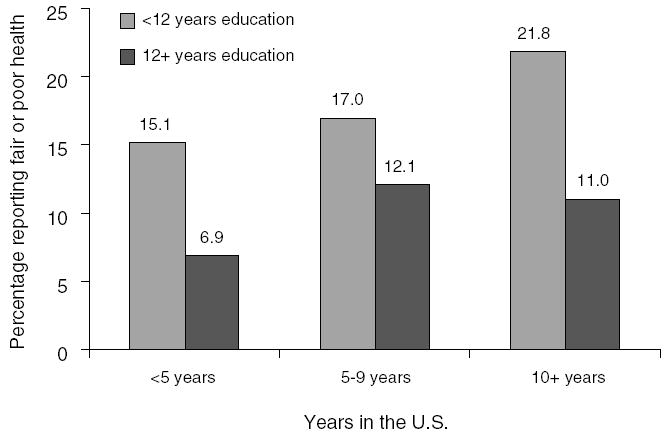
SELF-REPORTED HEALTH STATUS AMONG FOREIGN-BORN HISPANICS BY DURATION OF RESIDENCE IN THE UNITED STATES AND EDUCATIONAL ATTAINMENT
Using data from the 1992–96 National Health Interview Surveys, more recent research examined disparities between immigrant and native racial/ ethnic groups in self-reported health and activity limitations. This study found that foreign-born Mexicans, Cubans, other Hispanics, and Island-born Puerto Ricans were worse off compared with U.S.-born non-Hispanic whites with respect to one or both health outcomes studied after controlling for age and gender.69 Controlling for educational attainment, income, family size, and urban residence reduced, eliminated, or reversed all disparities between immigrant Hispanic subgroups and U.S.-born non-Hispanic whites (Tables 3 and 4).
TABLE 3.
ODDS RATIOS FROM UNWEIGHTED LOGISTIC REGRESSIONS OF HEALTH STATUS (IN FAIR OR POOR HEALTH) ON RACE/ETHNICITY AND IMMIGRANT STATUS, NATIONAL HEALTH INTERVIEW SURVEY, 1992–96
| INDEPENDENT VARIABLE | MODEL 1 | MODEL 2 | MODEL 3 | MODEL 4 |
|---|---|---|---|---|
| White U.S.-born (reference) (n = 68,370) | 1.00 | 1.00 | 1.00 | 1.0 |
| Island-born Puerto Rican (n = 619) | 2.58***a | 1.55*** | 1.26** | 1.36*** |
| Mainland-born Puerto Rican (n = 123) | 1.10a | 1.09 | 1.00 | 1.00 |
| Cuban immigrant (n = 746) | 1.53*** | 1.08 | 0.95 | 0.84*a |
| Cuban U.S.-born (n = 94) | 1.69 | 1.47 | 1.46 | 1.39a |
| Mexican immigrant (n = 1,175) | 2.05*** | 1.00a | 0.83**a | 0.78***a |
| Mexican U.S.-born (n = 1,832) | 2.03*** | 1.26***a | 1.10a | 1.00a |
| Other Hispanic immigrant (n = 906) | 1.40*** | 0.98 | 0.84*a | 0.84*a |
| Other Hispanic U.S.-born (n = 1,160) | 1.29*** | 1.11 | 1.07a | 1.03a |
| Controls | ||||
| Age, sex, year, self-report | ✓ | ✓ | ✓ | ✓ |
| Education | ✓ | ✓ | ✓ | |
| Income, family size | ✓ | ✓ | ||
| Region, MSA size, central city | ✓ | |||
Source: Heron MP, Schoeni RF, Morales LS. Health status of immigrants in the United States. Manuscript submitted for publication, 2001.
Note: The sample is limited to adults age 55 and older. Regression covariates include those listed in addition to indicators for immigrant whites and the following immigrant and U.S.-born groups: blacks, Chinese, Japanese, other Asian, and other. MSA = metropolitan statistical area.
Indicates statistically significant difference at p < 0.05 level between immigrants and U.S.-born persons within the same Hispanic subgroup.
p < 0.05.
p < 0.01.
p < 0.001.
TABLE 4.
ODDS RATIOS FROM UNWEIGHTED REGRESSIONS OF ACTIVITY LIMITATIONS ON RACE/ETHNICITY AND IMMIGRANT STATUS, NATIONAL HEALTH INTERVIEW SURVEY, 1992–96
| INDEPENDENT VARIABLE | MODEL 1 | MODEL 2 | MODEL 3 | MODEL 4 |
|---|---|---|---|---|
| White U.S.-born (reference) | 1.00 | 1.00 | 1.00 | 1.0 |
| Island-born Puerto Rican | 1.81***a | 1.27** | 1.05 | 1.15 |
| Mainland-born Puerto Rican | 1.03a | 1.03 | 0.94 | 0.95 |
| Cuban immigrant | 0.88 | 0.68*** | 0.62*** | 0.60*** |
| Cuban U.S.-born | 0.89 | 0.80 | 0.77 | 0.76 |
| Mexican immigrant | 1.22** | 0.71***a | 0.60***a | 0.53***a |
| Mexican U.S.-born | 1.38*** | 0.98a | 0.87**a | 0.77***a |
| Other Hispanic immigrant | 0.94 | 0.72***a | 0.62***a | 0.62***a |
| Other Hispanic U.S.-born | 0.96 | 0.88*a | 0.85*a | 0.81**a |
| Controls | ||||
| Age, sex, year, self-report | ✓ | ✓ | ✓ | ✓ |
| Education | ✓ | ✓ | ✓ | |
| Income, family size | ✓ | ✓ | ||
| Region, MSA size, central city | ✓ | |||
Source: Heron, Schoeni, and Morales, 2001.
Note: The sample is limited to adults age 55 and older. Regression covariates include those listed in addition to indicators for immigrant whites and the following immigrant and U.S.-born groups: blacks, Chinese, Japanese, other Asian, and other. MSA = metropolitan statistical area.
Indicates statistically significant difference at p < 0.05 level between immigrants and U.S.-born persons within the same Hispanic subgroup.
p < 0.05.
p < 0.01.
p < 0.001.
This study also found that there were few differences in self-reported health and activity limitations between immigrants and U.S.-born persons within the same Hispanic subgroup after controlling for age and gender, except between Island-born and mainland-born Puerto Ricans. However, controlling for educational attainment, income, family size, and urban residence eliminated the disparities between island-born and mainland-born Puerto Ricans. Among the other Hispanic subgroups, controlling for educational attainment, income, family size, and urban residence resulted in better self-reported health and lower rates of activity limitations for immigrants than natives.
The Hispanic health paradox
Research suggests that social, economic, and environmental factors, as well as access to health care, influence the health of populations.1–3,6,70 Associations between mortality and various socioeconomic characteristics including education,5,71–79 occupation and employment,2,5,73,76,79–83 health insurance,84,85 and poverty,86,87 as well as between mortality and socioeconomic position88–90 have been reported. Other factors also associated with socioeconomic status including the effect of the intrauterine environment,91 the cumulative effects of prolonged exposures to stressful life events,92 and reactions to macrosocietal factors such as rising levels of income inequality93 are also being investigated. On the basis of this body of evidence, one would expect Hispanics to have significantly poorer health outcomes than whites (Table 2). As we have seen, however, this is not generally the case.
The paradox of relatively good health outcomes for Hispanics in the face of high socioeconomic risks hinges primarily on mortality data, the quality of which has been questioned. The mortality statistics presented in this paper were in large part prepared by the vital statistics system of the United Sates. However, research has shown that the race and ethnicity data reported in vital statistics are questionable, particularly for Hispanics. In the National Mortality Follow-Back Survey, demographic data of death certificates were compared with demographic data provided by next of kin. While only 1.1 percent of cases were in disagreement, in 88.5 percent of these cases, the origin on the death certificate was non-Hispanic, whereas the origin provided by next of kin was Hispanic.94 In the National Longitudinal Mortality Study, selected administrations of the CPS from the Bureau of the Census were matched to death certificates through the National Death Index.95 Agreement between self-identified Hispanic ethnicity in the CPS and ethnicity identified by next of kin on the death certificates was 89.7 percent. Agreement between the two data sources was 84.9 percent for Mexicans, 85.9 percent for Puerto Ricans, and 80 percent for Cubans. In the same study, agreement on foreign-born status was 97.3 percent, while agreement on native-born status was 98.1 percent.
Although misclassification of Hispanics as non-Hispanics can cause the true mortality rate among Hispanics to be underestimated, census undercounts can inflate it. This occurs because the numerator in mortality rates provided by the National Center for Health Statistics is derived from death certificates, and the denominator is derived from the census data. It is estimated that the 1990 census undercounted blacks by 4.6 percent, whites and others by 0.7 percent, and Hispanics by 5.0 percent.96 A recent study that accounted for census undercounts and death certificate misclassification among racial/ethnic groups found that vital statistics underestimate Hispanic mortality rates, but that the rates for Hispanics are only increased by 1.6 percent by adjustment and that they remain about 20 percent below those of the white population.96 Similar studies of Hispanic subgroup mortality rates have not been conducted.
Various studies have investigated the comparability of Hispanic and white mortality rates. In a recent study using data from the National Health Interview Survey and the National Death Index, overall mortality among Hispanics was found to be lower than among whites, particularly among adults age 65 years and older.66 In the same study, mortality among younger Hispanics was higher than that of similarly aged whites, and risk of death among foreign-born Hispanics was lower than among whites. In a different study using data from the National Health Interview Survey, Mexican Americans and whites were found to have similar mortality rates.97 Areport from the San Antonio Heart Study used information from next of kin to ascertain vital status for 98.1 percent of the cohort.67 The eight-year mortality rates for U.S.-born Mexican Americans and whites were similar, although the total number of deaths in the study was small (N = 136). In an earlier study based on the National Longitudinal Mortality Study, relative to whites, Hispanics were found to have lower overall mortality, lower morality due to cancer, and lower mortality due to cardiovascular disease, but higher mortality due to diabetes mellitus and to homicide.98
Relatively few studies have examined mortality among Hispanic subgroups. Those that have, though, suggest that the positive side of the health paradox does not appear to hold for all subgroups. Specifically, mortality is higher among Puerto Ricans relative to Mexican and Cuban migrants living in the United States.99
The reasons for the health paradox among Hispanics are not entirely clear. The healthy migrant effect is one explanation mentioned in the literature. It posits that healthier persons are more likely to emigrate than their relatively less healthy compatriots, which results in a greater longevity in the emigrant population. This theory is of interest because more than one-third of Hispanics are foreign-born, making migrants an important segment of the Hispanic population. Although relatively few studies have examined the health of immigrants, those we reviewed suggest that foreign-born Hispanics have a mortality advantage over U.S.-born Hispanics, but that the health of the foreign-born may decline with the duration of residence in the United States.
A second hypothesis, the moribund migrant effect, posits that older and/or dying Hispanics return to their country of origin to die and therefore are unlikely to be counted among U.S. decedents (or, following their departure, in the census). This emigration effect would cause estimates of Hispanic mortality to be understated and would inflate life expectancy estimates. Little research has been conducted to examine the rate of return migration among Hispanics. In one study of emigration among the foreign-born population enumerated in the 1980 and 1990 censuses, only 7 percent of Hispanic immigrants were found to have left the United States.100 In comparison, non-Hispanic white and Asian/Pacific Islander emigration rates were 10 percent to 11 percent. The authors suggested that the emigration rate for Hispanics was probably low for the same reasons that the Hispanic immigration rate is so high (e.g., the relative difference in economic and social conditions between the origin and destination countries). Other studies corroborate the low rates of emigration before death among Hispanics.101
The acculturation hypothesis is related to the healthy-migrant effect theory because, on average, immigrants are presumably less acculturated than U.S.-born Hispanics. The acculturation hypothesis posits that Hispanic cultural orientation (i.e., traditional Mexican culture) results in health-related behaviors that protect Hispanics from the adverse health outcomes associated with low socioeconomic status in the United States. Furthermore, the acculturation hypothesis suggests that as one’s cultural orientation changes to that of U.S. culture, some of these protective behaviors are lost.
The evidence reviewed in this paper generally supports the acculturation hypothesis, with some salient points to be noted. Smoking and alcohol consumption increase with acculturation, particularly among women. Acculturation effects on diet include both health-enhancing and deleterious changes, but the net effect has been judged to be deleterious. The relationship between weight and acculturation, however, does not support the acculturation hypothesis, as obesity is higher among less acculturated Hispanics, particularly women.
Overall, the studies and vital statistics reviewed in this paper support the existence of a Hispanic health paradox (Table 5). Although Hispanics have significantly higher socioeconomic risks and less access to health care than whites, they have comparable health outcomes. Lifestyle and behavioral differences alone between whites and Hispanics do not appear to be strong enough to explain this finding.
TABLE 5.
SUMMARY OF FINDINGS
| DETERMINANT OF HEALTH | RISK PATTERN |
|---|---|
| Socioeconomic status | |
| Education | Hispanic > White |
| Income | Hispanic > White |
| Occupation | Hispanic > White |
| Behavioral risk factor | |
| Tobacco use | White > Hispanic |
| Diet | White ≥ Hispanic |
| Alcohol consumption | White > Hispanic |
| Sedentary lifestyle | White < Hispanic |
| Access to care | |
| Insurance | Hispanic > White |
| Use of care | Hispanic > White |
| Health status | |
| Life expectancy | White > Hispanic |
| Mortality | White > Hispanic |
| Infant mortality | White > Hispanic |
An equally important finding is that the health paradox does not appear to hold for all Hispanic subgroups equally. Specifically, the paradox appears to hold most strongly for Mexicans but does not appear to hold for Puerto Ricans. Therefore, regarding Hispanics as a monolithic group in future research and analysis may risk masking important heterogeneity among Hispanic subgroups.
Implications for health policy
This review suggests several strategies for improving the health of Hispanics. First, better data collection strategies are needed to improve the quality of morbidity and mortality data available for Hispanics. As we have seen in this review, there are significant problems with the current system for collecting vital statistics on Hispanics. Strategies for improving this system include adding Hispanic subgroup identifiers to all major surveys, including a sufficient sample size of Hispanics for data analysis at the Hispanic subgroup level, conducting additional research to improve the identification of Hispanics by cultural group and by level of acculturation, increasing the consistency of reporting of data on Hispanics, and increasing the participation of marginalized Hispanics (such as the Spanish-speaking, immigrants, and people with very low incomes) in research. Other data collection and research issues include developing standard methods for collecting acculturation information on surveys and developing standard methods for translating Spanish-language instruments.
The health paradox is most striking among Mexicans, who average the lowest socioeconomic status among the Hispanic subgroups but also have the lowest age-adjusted, all-cause mortality rate. The Cuban mortality rate is greater than that of Mexicans and is similar to that of whites. However, Cubans also have the highest socioeconomic levels among Hispanics, although they are still disadvantaged relative to whites. Puerto Ricans, on the other hand, are less advantaged than whites and have a higher all-cause morality rate. Of these Hispanic subgroups, Puerto Ricans appear to least exhibit the health paradox.
From a prevention standpoint, identifying the components of Hispanic culture that provide protection from the adverse effects of low socioeconomic status is important. As reported in this review, Guendelman and Abrams, for example, found that the loss of protective dietary habits is linked to generational status among pregnant Mexican women.23 Their work suggests that traditional dietary preferences, more common among first-generation Mexican women than among second-generation women, may, in part, account for generational differences in rates of LBW.102 Furthermore, Guendelman and Abrams reported that more acculturated women had diets similar to those of white women. Therefore, their work suggests that traditional dietary choices (with some modifications) should be encouraged among less acculturated and first-generation Mexican women, while more acculturated Mexican women may require health education strategies similar to those used among white women.
Other research presented in this review suggests that smoking and alcohol consumption are also linked to acculturation, particularly among women. Learning how Hispanic women lose the attributes that proscribe adverse health behaviors, such as drinking and smoking, and how they develop attributes that do not effectively proscribe them may aid in the design of health promotion efforts.
Strategies to prevent smoking and reduce drinking among Hispanic women may differ by level of acculturation. On one hand, more acculturated women may respond to approaches developed for white women, while less acculturated women may respond to different approaches. Distinctions between the two approaches might include a greater emphasis on family and friends than on the individual when targeting less acculturated individuals. For example, in a community intervention to reduce smoking among Hispanics in San Francisco, antismoking messages were developed that emphasized the adverse consequences of smoking on children and family, rather than the adverse consequences of smoking on the individual.17
This review also shows that Hispanics continue to lag behind whites in access to care. While this is not a new finding, it is a persistent one that deserves continued attention. Hispanics have higher diabetes and HIV/AIDS mortality rates than whites. Effective treatments exist for controlling both these conditions, and therefore reductions in mortality might be achieved by improved access to medical care. One of the most important determinants of access is insurance coverage and, as our review notes, Hispanics lag behind whites in coverage. Therefore, policies and programs to increase insurance coverage for Hispanics should remain a priority.
Gaining access to medical care through insurance coverage is necessary but insufficient to effect positive changes on the overall health status of Hispanics. Medical care needs to be delivered in a culturally and linguistically appropriate fashion. Because the provider-patient interaction is central to the delivery of health care, Spanish-language interpreters and Spanish-language written materials are necessary. Increased attention needs to be given to the literacy level of these materials, in addition to making the content relevant for the Hispanic population. For example, dietary information using traditional cooking ingredients (which varies by subgroup) should be made available to Hispanic patients.
Finally, although Hispanics, particularly Mexicans, appear to have protective attributes that counter the effects of low socioeconomic status, Hispanics with higher socioeconomic status have better health than those with lower socioeconomic status. Therefore, it is still important to advocate for policies to improve the social and economic circumstances of Hispanics in order to improve the health of this population. Policies to increase educational attainment, to improve employment opportunities, and to reduce violence and environmental pollution in Hispanic neighborhoods will all greatly benefit the health of Hispanics.
Acknowledgments
Support for this research was received from the Opening Doors Foundation to RAND (Leo S. Morales, principal investigator) and the Agency for Health Care Policy Research to RAND (U18HS09204) (Leo S. Morales, co–principal investigator). This paper was prepared while Leo Morales was a Robert Wood Johnson Minority Medical Faculty Development Program Fellow (UCLA 042679).
Footnotes
DR. MORALES and DR. LARA are assistant professors in residence at the University of California, Los Angeles and natural scientists at RAND Health, Santa Monica. DR. KINGTON is associate director for Behavioral and Social Sciences Research at the National Insitutes of Health in Bethesda, Maryland. DR. VALDEZ is dean of the School of Public Health at MCP Hahnemann University in Philadelphia. DR. ESCARCE is senior natural scientist at RAND Health, Santa Monica.
Attribution refers to the likelihood that children of mixed ethnic background will report themselves as Hispanic.
The population of the Island of Puerto Rico is not included in this estimate.
Acculturation refers to the process by which individuals whose primary lifestyle has been that of one culture (e.g., Latin American) acquire characteristic ways of living of another culture (e.g., Anglo American). As implied by the definition, acculturation scales typically assume that an individual moves from one cultural orientation to another, losing the first as the second is acquired. More complex theories of acculturation posit that individuals may simultaneously retain one ethnic identity while also learning the new culture’s traditions and values. While the latter conceptualization of acculturation is appealing, it is rarely used in studies.
The National Health Interview Survey asks about limitations with major activity. Major activity is defined differently according to the age of the survey respondent. Survey respondents between 18 and 69 are asked about limitations with working, keeping house, or going to school. Survey respondents 70 and older are asked about limitations with activities of daily living such as household chores, shopping, and getting around.
References
- 1.Marmot MG, Smith GD, Stansfeld S, et al. Health inequalities among British civil servants: The Whitehall II study. Lancet. 1991 Jun 8;337(8754):1387–93. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- 2.Marmot MG, Shipley MJ, Rose G. Inequalities in death—specific explanations of a general pattern? Lancet. 1984 May 5;1(8384):1003–6. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 3.Feinstein JS. The relationship between socioeconomic status and health: Areview of the literature. Milbank Q. 1993;71(2):279–322. [PubMed] [Google Scholar]
- 4.House JS, Kessler RC, Herzog AR. Age, socioeconomic status, and health. Milbank Q. 1990;68(3):383–411. [PubMed] [Google Scholar]
- 5.Kitagawa EM, Hauser PM. Differential mortality in the United States: A study of socioeconomic epidemiology. Cambridge, MA: Harvard University Press; 1973. [Google Scholar]
- 6.Antonovsky A. Social class, life expectancy and overall mortality. Milbank Mem Fund Q. 1967 Apr;45(2):31–73. [PubMed] [Google Scholar]
- 7.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: An epidemiologic paradox. Public Health Rep. 1986 May–Jun;101(3):253–65. [PMC free article] [PubMed] [Google Scholar]
- 8.Scribner R. Paradox as paradigm—The health outcomes of Mexican Americans. Am J Public Health. 1996 Mar;86(3):303–5. doi: 10.2105/ajph.86.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guzmán B. The Hispanic population: Census 2000 brief. Washington, DC: U.S. Census Bureau; 2001. [Google Scholar]
- 10.Day JC. U.S. Census Bureau, Current Population Reports. Report No. P25–1130. Washington, DC: Government Printing Office; 1996. Population projections of the United States by age, sex, races and Hispanic origin: 1995 to 2050. [Google Scholar]
- 11.Smith JP, Edmonston B. The face of the U.S. population in 2050. In: Smith JP, Edmonston B, editors. The new Americans. Washington, DC: National Academy Press; 1997. [Google Scholar]
- 12.U.S. Census Bureau, Current Population Reports. The Hispanic population of the United States. Washington, DC: U.S. Census Bureau; 1997. [Google Scholar]
- 13.Stevens G. Immigration, emigration, language acquisition, and the English language proficiency of immigrants to the United States. In: Edmonston B, Passel JS, editors. Immigration and ethnicity. Washington, DC: The Urban Institute Press; 1994. [Google Scholar]
- 14.Friedman-Jimenez G, Ortiz JS. Latino Health and the work environment. In: Molina CW, Aguirre-Molina M, editors. Latino health in the U.S.: A growing challenge. Washington, DC: American Public Health Association; 1994. [Google Scholar]
- 15.Language: Diversity and assimilation. In: Lopez DE, editor; Waldinger R, Bozorgmehr M, editors. Ethnic Los Angeles. New York: Russel Sage Foundation; 1996. [Google Scholar]
- 16.Landrine H, Klonoff EA. Cultural change, tobacco and alcohol use among U.S. ethnic minorities: An operant model of acculturation. In: Marin G, editor. Conference on acculturation: Advances in theory, measurement and applied research. San Francisco: University of San Francisco; 1998. [Google Scholar]
- 17.Perez-Stable EJ, Marin BV, Marin G. A comprehensive smoking program for the San Francisco Bay area Latino community: Programa Latino Para Dejar de Fumar. Am J Health Promot. 1993 Jul–Aug;7(6):430–42. doi: 10.4278/0890-1171-7.6.430. 475. [DOI] [PubMed] [Google Scholar]
- 18.Perez-Stable EJ, Marin G, Marin BV. Behavioral risk factors: A comparison of Latinos and non-Latino whites in San Francisco. Am J Public Health. 1994 Jun;84(6):971–76. doi: 10.2105/ajph.84.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.U.S. Department of Health and Human Services. Tobacco use among U.S. racial/ethnic minority groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A report of the U.S. surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]
- 20.Loria CM, Bush TL, Carroll MD, et al. Macronutrient intakes among adult Hispanics: A comparison of Mexican Americans, Cuban Americans, and mainland Puerto Ricans. Am J Public Health. 1995 May;85(5):684–89. doi: 10.2105/ajph.85.5.684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDowell MA, Briefel RR, Alaimo K, et al. Energy and macronutrient intakes of persons ages 2 months and over in the United States: Third National Health and Nutrition Examination Survey, Phase 1, 1988–91. Adv Data. 1994 Oct 24;(255):1–24. [PubMed] [Google Scholar]
- 22.Marshall JA, Lopez TK, Shetterly SM, et al. Association of education level with atherogenic diets in a rural biethnic population. Am J Prev Med. 1995 Sep–Oct;11(5):294–300. [PubMed] [Google Scholar]
- 23.Guendelman S, Abrams B. Dietary intake among Mexican-American women: Generational differences and a comparison with white non-Hispanic women. Am J Public Health. 1995 Jan;85(1):20–25. doi: 10.2105/ajph.85.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marks G, Garcia M, Solis JM. Health risk behaviors of Hispanics in the United States: Findings from HHANES, 1982–84. Am J Public Health. 1990 Dec;80(Suppl):20–26. doi: 10.2105/ajph.80.suppl.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tucker KL, Falcon LM. Nutrition among Hispanic elders in the United States. In: Markides KS, Miranda MR, editors. Minorities, health and aging. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- 26.Romero-Gwynn E, Gwynn D, Grivette L, et al. Dietary acculturation among Latinos of Mexican descent. Nutr Today. 1993 July–Aug;28(4):5–12. [Google Scholar]
- 27.Elder JP, Castro FG, de Moor C, et al. Differences in cancer-risk-related behaviors in Latino and Anglo adults. Prev Med. 1991 Nov;20(6):751–63. doi: 10.1016/0091-7435(91)90069-g. [DOI] [PubMed] [Google Scholar]
- 28.Otero-Sabogal R, Sabogal F, Perez-Stable EJ, et al. Dietary practices, alcohol consumption, and smoking behavior: Ethnic, sex, and acculturation differences. J Natl Cancer Inst Monogr. 1995;(18):73–82. [PubMed] [Google Scholar]
- 29.Aguirre-Molina M, Caetano R. Alcohol use and alcohol-related issues. In: Molina CW, Aguirre-Molina M, editors. Latino health in the U.S.: A growing challenge. Washington, DC: American Public Health Association; 1994. [Google Scholar]
- 30.Caetano R. Drinking, ethnic identity, and educational status among Mexican Americans. Berkeley, CA: Pacific Medical Research Institute, Alcohol Research Group; 1988. [Google Scholar]
- 31.Caetano R. Responding to alcohol-related problems among Hispanics. Contemp Drug Problems. 1988 fall;15(3):335–63. [Google Scholar]
- 32.National Heart, Lung and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. The evidence report. Bethesda, MD: National Heart, Lung and Blood Institute; 1998. (NIH Pub. No. (NIH) 98–4083.) [Google Scholar]
- 33.Pamuk E, Makuc D, Heck K, et al. Socioeconomic status and health chartbook. Health, United States, 1998. Washington, DC: National Center for Health Statistics; 1998. [Google Scholar]
- 34.Najjir MF, Kuczmarski RJ. Anthropometric data and the prevalence of overweight for Hispanics: 1982–1984. Washington, DC: U.S. Department of Health and Human Services; 1989. (DHHS Pub. No. (PHS) 89–1689.) [PubMed] [Google Scholar]
- 35.Stern MP, Pugh JA, Gaskill SP, et al. Knowledge, attitudes, and behavior related to obesity and dieting in Mexican Americans and Anglos: The San Antonio Heart Study. Am J Epidemiol. 1982 Jun;115(6):917–28. doi: 10.1093/oxfordjournals.aje.a113379. [DOI] [PubMed] [Google Scholar]
- 36.U.S. Department of Health and Human Services. Physical activity and health: Areport of the surgeon general. Washington, DC: U.S. Department of Health and Human Services; 1996. [Google Scholar]
- 37.Burchfiel CM, Hamman RF, Marshall JA, et al. Cardiovascular risk factors and impaired glucose tolerance: The San Luis Valley Diabetes Study. Am J Epidemiol. 1990 Jan;131(1):57–70. doi: 10.1093/oxfordjournals.aje.a115485. [DOI] [PubMed] [Google Scholar]
- 38.Estrada AL, Trevino FM, Ray LA. Health care utilization barriers among Mexican Americans: Evidence from HHANES 1982–84. Am J Public Health. 1990 Dec;80(Suppl):27–31. doi: 10.2105/ajph.80.suppl.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schur CL, White LA, Berk ML. Health care use by Hispanic adults: The role of financial vs. nonfinancial determinants [abstract] AHSR FHSR. Annu Meet Abstr Book. 1995;12:103. [Google Scholar]
- 40.Hoffman C, Pohl M. Health insurance coverage in America: 1999 data update. The Kaiser Commission on Medicaid and the Uninsured; 2000. [Google Scholar]
- 41.Giachello AL. Issues of access and use. In: Molina CW, Aguirre-Molina M, editors. Latino health in the U.S.: A growing challenge. Washington, DC: American Public Health Association; 1994. [Google Scholar]
- 42.Thamer M, Richard C, Casebeer AW, et al. Health insurance coverage among foreign-born U.S. residents: The impact of race, ethnicity, and length of residence. Am J Public Health. 1997 Jan;87(1):96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bennefield R. Census Brief: Children without Health Insurance. Report No. CENBR/98–1. Washington, DC: U.S. Department of Commerce; 1998. [Google Scholar]
- 44.Halfon N, Wood DL, Valdez RB, et al. Medicaid enrollment and health services access by Latino children in inner-city Los Angeles. JAMA. 1997 Feb 26;277(8):636–41. [PubMed] [Google Scholar]
- 45.U.S. Department of Health and Human Services. Interagency task force on children’s health insurance outreach: A report to the president, 1998. Retrieved on August 1, 2001, from http://cms.hhs.gov/schip/chiprpt.pdf.
- 46.Angel RJ, Angel JL. Health services use and long term care among Hispanics. In: Markides KS, Miranda MR, editors. Minorities, aging, and health. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- 47.Angel JL, Angel RJ, McClellan JL, et al. Nativity, declining health, and preferences in living arrangements among elderly Mexican Americans: Implications for long-term care. Gerontologist. 1996 Aug;36(4):464–73. doi: 10.1093/geront/36.4.464. [DOI] [PubMed] [Google Scholar]
- 48.Valdez RB, Giachello Á, Rodriguez-Trias H, et al. Improving access to health care in Latino communities. Public Health Rep. 1993 Sep–Oct;108(5):534–39. [PMC free article] [PubMed] [Google Scholar]
- 49.Komaromy M, Grumbach K, Drake M, et al. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996 May 16;334(20):1305–10. doi: 10.1056/NEJM199605163342006. [DOI] [PubMed] [Google Scholar]
- 50.Baker DW, Parker RM, Williams MV, et al. Use and effectiveness of interpreters in an emergency department. JAMA. 1996 Mar 13;275(10):783–88. [PubMed] [Google Scholar]
- 51.Lapham SJ, Montgomery P, Niner D. We the American foreign born. Report No. WE-7. Washington, DC: U.S. Department of Commerce; 1993. [Google Scholar]
- 52.Morales LS, Cunningham WE, Brown JA, et al. Are Latinos less satisfied with communication by health care providers? A study of 48 medical groups. J Gen Intern Med. 1999 Jul;14(7):409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Perez-Stable EJ, Naapoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997 Dec;35(12):1212–19. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Molina CW, Zambrana E, Aguirre-Molina M. The influence of culture, class and environment on health care. In: Molina CW, Aguirre-Molina M, editors. Latino health: A growing challenge. Washington, DC: American Public Health Association; 1994. [Google Scholar]
- 55.Gregory D. Transcultural medicine: Treating Hispanic patients. Behav Med. 1978 Feb;3(1):22–29. [Google Scholar]
- 56.Kominski GF, Pourat N. Differences in utilization of ambulatory care among Asian Americans. Abstr Book Assoc Health Serv Res. 1997;14:71–72. [Google Scholar]
- 57.Trevino FM, Moss AJ. Health Indicators for Hispanic, black and white Americans. Washington, DC: National Center for Health Statistics; 1984. (NCHS Rep. No. [PHS] 84–1576.) [DOI] [PubMed] [Google Scholar]
- 58.Guendelman S, Wagner TH. Health services utilization among Latinos and white non-Latinos: Results from a national survey. J Health Care Poor Underserved. 2000 May;11(2):179–94. doi: 10.1353/hpu.2010.0719. [DOI] [PubMed] [Google Scholar]
- 59.Schur CL, Bernstein AB, Berk ML. The importance of distinguishing Hispanic sub-populations in the use of medical care. Med Care. 1987 Jul;25(7):627–41. doi: 10.1097/00005650-198707000-00006. [DOI] [PubMed] [Google Scholar]
- 60.Flores G, Bauchner H, Feinstein A, et al. The impact of ethnicity, family income, and paternal education on children’s health and use of health services. Am J Public Health. 1999 Jul;89(7):1066–71. doi: 10.2105/ajph.89.7.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anderson RN, Kochanek KD, Murphy SL. Report of final mortality statistics, 1995. Mon Vital Stat Rep. 1997;45(11 suppl 2) [Google Scholar]
- 62.U.S. Bureau of the Census. Selected social characteristics of all persons and Hispanic persons, by type of origin: March, 1996. Washington, DC: U.S. Bureau of the Census; 1998. [Google Scholar]
- 63.U.S. Department of Health and Human Services (DHHS), National Center for Health Statistics (NCHS) National Health Interview Survey, 1994 [computer file]. ICPSR ver. Hyattsville, MD: DHHS, NCHS [producer], 1995. Ann Arbor, MI: Inter-University Consortium for Political and Social Science Research [distributor]; 1996. [Google Scholar]
- 64.Hajat A, Lucas JB, Kington R. National Center for Health Statistics. Vital and Health Statistics/Advance Data. February 2000. Health outcomes among Hispanic subgroups: Data from the National Health Interview Survey, 1992–95. Report No. 310. [PubMed] [Google Scholar]
- 65.Fuentes-Afflick E, Lurie P. Low birth weight and Latino ethnicity. Examining the epidemiologic paradox. Arch Pediatr Adolesc Med. 1997 Jul;151(7):665–74. doi: 10.1001/archpedi.1997.02170440027005. [DOI] [PubMed] [Google Scholar]
- 66.Liao Y, Cooper RS, Cao G, et al. Mortality patterns among adult Hispanics: Findings from the NHIS, 1986 to 1990. Am J Public Health. 1998 Feb;88(2):227–32. doi: 10.2105/ajph.88.2.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wei M, Valdez RA, Mitchell BD, et al. Migration status, socioeconomic status, and mortality rates in Mexican Americans and non-Hispanic whites: The San Antonio Heart Study. Ann Epidemiol. 1996 Jul;6(4):307–13. doi: 10.1016/s1047-2797(96)00026-9. [DOI] [PubMed] [Google Scholar]
- 68.Stephen EH, Foote K, Hendershot GE, et al. Health of the foreign-born population: United States, 1989–90. Adv Data. 1994 Feb 14;(241):1–12. [PubMed] [Google Scholar]
- 69.Schoeni R, Heron M, Morales L. Disparities in health status among immigrant and native ethnic groups. RAND labor and population working paper. Santa Monica, CA: RAND; 2001. [Google Scholar]
- 70.Antonovsky A, Bernstein J. Social class and infant mortality. Soc Sci Med. 1977 May;11(8–9):453–70. doi: 10.1016/0037-7856(77)90022-1. [DOI] [PubMed] [Google Scholar]
- 71.Feldman JJ, Makuc DM, Kleinman JC, et al. National trends in educational differentials in mortality. Am J Epidemiol. 1989 May;129(5):919–33. doi: 10.1093/oxfordjournals.aje.a115225. [DOI] [PubMed] [Google Scholar]
- 72.Ries P. Educational differences in health status and health care. Vital Health Stat [10] 1991 Sep;(179):1–66. [PubMed] [Google Scholar]
- 73.Guralnik JM, Land KC, Blazer D, et al. Educational status and active life expectancy among older blacks and whites. N Engl J Med. 1993 Jul 8;329(2):110–16. doi: 10.1056/NEJM199307083290208. [DOI] [PubMed] [Google Scholar]
- 74.Doornbos G, Kromhout D. Educational level and mortality in a 32-year follow-up study of 18-year-old men in the Netherlands. Int J Epidemiol. 1990 Jun;19(2):374–79. doi: 10.1093/ije/19.2.374. [DOI] [PubMed] [Google Scholar]
- 75.Kunst AE, Mackenbach JP. The size of mortality differences associated with educational level in nine industrialized countries. Am J Public Health. 1994 Jun;84(6):932–37. doi: 10.2105/ajph.84.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Slater CH, Lorimor RJ, Lairson DR. The independent contributions of socioeconomic status and health practices to health status. Prev Med. 1985 May;14(3):372–78. doi: 10.1016/0091-7435(85)90063-5. [DOI] [PubMed] [Google Scholar]
- 77.Liu K, Cedres LB, Stamler J, et al. Relationship of education to major risk factors and death from coronary heart disease, cardiovascular diseases and all causes: Findings of three Chicago epidemiologic studies. Circulation. 1982 Dec;66(6):1308–14. doi: 10.1161/01.cir.66.6.1308. [DOI] [PubMed] [Google Scholar]
- 78.Keil JE, Sutherland SE, Knapp RG, et al. Mortality rates and risk factors for coronary disease in black as compared with white men and women. N Engl J Med. 1993 Jul 8;329(2):73–78. doi: 10.1056/NEJM199307083290201. [DOI] [PubMed] [Google Scholar]
- 79.Seltzer CC, Jablon S. Army rank and subsequent mortality by cause: 23-year follow-up. Am J Epidemiol. 1977 Jun;105(6):559–66. doi: 10.1093/oxfordjournals.aje.a112420. [DOI] [PubMed] [Google Scholar]
- 80.Rogot E, Sorlie PD, Johnson NJ. Life expectancy by employment status, income and education in the National Longitudinal Study. Public Health Rep. 1992 Jul–Aug;107(4):457–61. [PMC free article] [PubMed] [Google Scholar]
- 81.Cooper SP, Buffler PA, Cooper CJ. Health characteristics by occupation and industry of longest employment. Vital Health Stat [10] 1989 Jun;(168):1–105. [PubMed] [Google Scholar]
- 82.Pearce NE, Davis PB, Smith AH, et al. Mortality and social class in New Zealand II: Male mortality by major disease groupings. N Z Med J. 1983 Sep 28;96(740):711–16. [PubMed] [Google Scholar]
- 83.Moser KA, Fox AJ, Jones DR. Unemployment and mortality in the OPCS Longitudinal Study. Lancet. 1984 Dec 8;2(8415):1324–29. doi: 10.1016/s0140-6736(84)90832-8. [DOI] [PubMed] [Google Scholar]
- 84.U.S. Office of Technology Assessment. Does health insurance make a difference? Washington, DC: U.S. Office of Technology Assessment; 1992. (OTA Pub. No. BP-H-99.) [Google Scholar]
- 85.Franks P, Clancy CM, Gold MR. Health insurance and mortality: Evidence from a national cohort. JAMA. 1993 Aug 11;270(6):737–41. [PubMed] [Google Scholar]
- 86.Williams DR, Collins C. U.S. socioeconomic and racial differences in health: Patterns and explanations. Ann Rev Sociol. 1995;21:349–86. [Google Scholar]
- 87.Haan M, Kaplan GA, Camacho T. Poverty and health: Prospective evidence from the Alameda County Study. Am J Epidemiol. 1987 Jun;125(6):989–98. doi: 10.1093/oxfordjournals.aje.a114637. [DOI] [PubMed] [Google Scholar]
- 88.Newacheck PW, Butler LH, Harper AK, et al. Income and illness. Med Care. 1980 Dec;18(12):1165–76. doi: 10.1097/00005650-198012000-00002. [DOI] [PubMed] [Google Scholar]
- 89.Lundberg O. Class and health: Comparing Britain and Sweden. Soc Sci Med. 1986;23(5):511–17. doi: 10.1016/0277-9536(86)90011-0. [DOI] [PubMed] [Google Scholar]
- 90.Amick BC, Levine S, Tarlov AR, et al. Society and health. New York: Oxford University Press; 1995. [Google Scholar]
- 91.Barker DJ, Osmond C, Golding J, et al. Growth in utero, blood pressure in childhood and adult life, and mortality from cardiovascular disease. BMJ. 1989 Mar 4;298(6673):564–67. doi: 10.1136/bmj.298.6673.564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Seeman TE, Singer BH, Rowe JW, et al. Price of adaptation—Allostatic load and its health consequences. MacArthur studies of successful aging. Arch Intern Med. 1997 Oct 27;157(19):2259–68. [PubMed] [Google Scholar]
- 93.Wilkenson RG. Unhealthy societies: The afflictions of inequality. London: Routledge; 1996. [Google Scholar]
- 94.Poe GS, Powell-Griner E, McLaughlin JK, et al. Comparability of the death certificate and the 1986 National Mortality Followback Survey. Vital Health Stat 2. 1993 Nov;(118):1–53. [PubMed] [Google Scholar]
- 95.Sorlie PD, Rogot E, Johnson NJ. Validity of demographic characteristics on the death certificate. Epidemiology. 1992 Mar;3(2):181–84. doi: 10.1097/00001648-199203000-00018. [DOI] [PubMed] [Google Scholar]
- 96.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: A summary of current research, 1999. National Center for Health Statistics. Vital Health Stat 2. 1999 Sep;(128):1–13. [PubMed] [Google Scholar]
- 97.Rogers RG, Hummer RA, Nam CB, et al. Demographic, socioeconomic and behavioral factors affecting ethnic mortality by cause. Social Forces. 1996;74(4):1419–38. [Google Scholar]
- 98.Sorlie PD, Backlund E, Johnson NJ, et al. Mortality by Hispanic status in the United States. JAMA. 1993 Nov 24;270(20):2464–68. [PubMed] [Google Scholar]
- 99.Rosenwaike I. Mortality differentials among persons born in Cuba, Mexico, and Puerto Rico residing in the United States, 1979–81. Am J Public Health. 1987 May;77(5):603–6. doi: 10.2105/ajph.77.5.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ahmed B, Robinson JG. Estimates of emigration of the foreign-born population: 1980–1990. Washington, DC: U.S. Bureau of the Census; 1994. (Pub. No. 9.) [Google Scholar]
- 101.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, et al. The Latino mortality paradox: A test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999 Oct;89(10):1543–48. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Guendelman S, Gould JB, Hudes M, et al. Generational differences in perinatal health among the Mexican American population: findings from HHANES 1982–84. Am J Public Health. 1990 Dec;80(Suppl):61–65. doi: 10.2105/ajph.80.suppl.61. [DOI] [PMC free article] [PubMed] [Google Scholar]


