Abstract
Objectives. We investigated whether the Kidskin sun protection intervention increased children’s body mass index by reducing the time spent outdoors at midday.
Methods. The Kidskin sun protection intervention involved 1614 Australian school children assigned to 1 of 3 groups: a control group, a moderate-intervention group, or a high-intervention group. Schools in the control group received the standard health curriculum and schools in the intervention groups received a multicomponent intervention. Outcomes included time spent outdoors and nevus development (a marker of melanoma risk). Height and weight were measured at 3 time points. Body mass index was transformed into age- and gender-specific z scores; z scores at each age were modeled simultaneously. Time spent outdoors at ages 10 and 12 years was analyzed using a linear mixed effects modeling.
Results. The proportion of children who were overweight or obese increased with age. The moderate-intervention and control groups had a minimal increase in z score over time, and the z score for the high-intervention group decreased over time. There were no differences among groups with respect to total time outdoors at any age.
Conclusions. It is possible to reduce the time children spend outdoors when ultraviolet radiation is high without producing an unfavorable effect on the children’s body mass index.
Childhood obesity is an independent risk factor for adult obesity and the associated health problems of type 2 diabetes, hypertension, and cardiovascular disease.1 In many developed countries, there has been a large increase in the prevalence of childhood overweight and obesity in recent years. The prevalence of obesity has increased two- to threefold over 25 years in the United States, and by the same amount over 10 years in the United Kingdom.2 In Australia, the prevalence of childhood overweight doubled, and that of obesity trebled between 1985 and 1995; 20% to 25% of children are currently being classified as overweight or obese.3 Furthermore, data from the last 35 years indicate that the increase in obesity among children is accelerating.1 It is not yet clear whether the increase is primarily because of higher energy intake, reduced physical activity, or both.1 However, encouraging both a healthy diet and more physical activity is recognized as a key strategy to curb these disturbing trends.4
Most interventions aimed at preventing or treating childhood overweight and obesity have been designed to improve children’s eating habits and increase their physical activity levels.5 Children have been particularly encouraged to walk or ride bicycles to school and to spend less of their leisure time engaged in sedentary activities.5 However, there is limited evidence that these interventions have been effective.6
Over the past 25 years, there have also been a growing number of sun protection interventions designed to reduce children’s exposure to sun in an effort to reduce the incidence of skin cancer in adult life.7 Many of these interventions have focused on reducing the time children spend outdoors in the middle of the day when solar ultraviolet radiation is most intense, typically between 10 am and 3 pm. Children have been encouraged to stay indoors and engage in a range of alternative indoor activities during these hours.7 Messages promoted in interventions (“Stay indoors and keep out of the sun”) are aimed at reducing exposure to the sun and may be perceived as being at odds with messages aimed at increasing physical activity (“Go outside and be active”). For example, studies consistently report that the time children spend outdoors is highly correlated with their level of physical activity.8 It is, therefore, plausible that adhering to the sun safety message could inadvertently have a detrimental affect on children’s body mass index (BMI).
Results from our study—the Kidskin sun protection intervention trial, conducted in Perth, Western Australia, between 1995 and 2001—have been published.9–13 In those articles, we reported that children who received the intervention spent less time outdoors in the middle of the day after both 2 years9 and 4 years of the intervention.13 We also reported that 2 years into the study, the total time spent outdoors was similar in the 3 study groups.9 For this analysis, we examined whether, after 6 years, the Kidskin intervention had an effect on the total time children spent outdoors—and thus, on their opportunity to engage in physical activity—or on their weight relative to height.
METHODS
Analysis
The design and baseline results of the Kidskin intervention study have been previously described.14 Briefly, the study involved a cohort of children who commenced school in 1995 at the age of 5 or 6 years (hereafter age 6). The design was a nonrandomized trial in which schools were the units of intervention.14 There were 3 groups: a control group of 14 schools, a moderate-intervention group of 11 schools, and a high-intervention group of 8 schools. Children in the control schools received the standard Western Australian health education curriculum.15 Children in the moderate- and high-intervention schools received a specially designed sun protection curriculum that was administered over 4 consecutive years, beginning with children aged 6 years (1995–1998). Children were encouraged to reduce sun exposure by staying indoors during the middle of the day, when solar ultraviolet radiation is highest, and to protect themselves when outdoors by using shade, clothing, hats, and sunscreen. The program was designed to be taught across the curriculum and integrated into a range of subjects, including physical education. Children in the high-intervention group were sent program materials over the summer vacation, when sun exposure is likely to be highest, and were also offered low-cost sun protective swimwear.
Outcomes used to evaluate the program included number of nevi (as a biological marker of melanoma risk), measured suntan, and reported time spent outdoors. Information on time spent outdoors was collected from questionnaires completed by parents when children were at baseline (age 6) and at ages 8, 10, and 12 years (age 8, age 10, and age 12, respectively). Parents were asked for the average time each day that the children were outdoors between 8 and 11 am, 11 am to 2 pm, and 2 to 5 pm. Data were recorded separately for the beach, public outdoor swimming pools, and at home and around the neighborhood (including backyard swimming pools). The total time spent outdoors was calculated by adding the responses for these 3 time periods.
In order to adjust for children’s body surface area in the analysis of nevi at ages 6, 10, and 12, each child’s height was measured to the nearest millimeter with a stadiometer, and weight was measured with a set of digital bathroom scales accurate to 200 g, according to standardized protocols. Trained observers were blinded to the aim of the current analysis. BMI (weight in kilograms divided by height in meters squared) at ages 6, 10, and 12 was subsequently calculated.
Body Size
BMI was transformed into age- and gender-specific z scores by the least mean squares method16 and by using 2000 growth chart data from the Centers for Disease Control and Prevention.17 The children were also classified as normal weight, overweight, or obese on the basis of their age, gender, and BMI. The age- and gender-specific BMI cutoff points for the 3 body size categories (normal weight, overweight, obese) were developed for the International Obesity Taskforce from large, nationally representative cross-sectional datasets from Brazil, Great Britain, Hong Kong, the Netherlands, Singapore, and the United States.18 The z score (BMI-for-age) and body size category were derived for each child using add-ons to Stata 8.2 (Stata Corp, College Station, Tex).19
In the primary analysis, the z score data collected at baseline (at age 6), at age 10, and at age 12 were modeled simultaneously by constructing linear models (growth curves) for z scores by time since baseline. We assessed the intervention by comparing a model in which each study group had its own slope for z score over time, with a model of a common slope, by fitting an interaction between study group and time. Because they were considered a priori to be potential confounders of the associations under study, gender, ethnicity (southern European vs Great Britain and northern European), and parental educational level (tertiary vs other) were included in all models. Random intercepts and slopes and covariances between these terms were fitted at the school and child level. Random effects were only retained if the likelihood ratio test had a P value<.05. The final model had a random intercept, slope, and covariance at the child level, and a random slope at the school level.
Two secondary analyses were performed, in which the outcome measure was z score at either age 10 or 12. The data were analyzed using linear mixed effects modeling that incorporated a random effect for school and adjustment for the fixed effects: study group, z score at baseline, gender, ethnicity, and parental educational level (as defined previously).
Total Time Spent Outdoors
Total time spent outdoors during the day, recorded at baseline (age 6), and at ages 8, 10, and 12, could not be analyzed simultaneously because of changes to the relevant questions in the questionnaire. Therefore, 2 separate analyses were performed in which the outcome measure was total time spent outdoors at either age 10 or 12. Comparison of total time spent outdoors at age 8 across study groups has been previously reported10 and is not presented here. These data were analyzed using linear mixed effects modeling that incorporated a random effect for school and adjustment for the fixed effects: study group, total time outdoors at baseline, gender, ethnicity, parental educational level (as defined previously), and tendency to sunburn (tendency to painfully and severely sunburn vs tendency to mildly or not sunburn). In all analyses, total time spent outdoors was log transformed after the addition of 1 to account for zero values.
MLwiN 2.1 (Centre for Multilevel Modeling, University of London, UK) was used to construct the linear growth curves. All other statistical analyses were performed using Stata 8.2.
RESULTS
Response and Retention
At the beginning of the Kidskin intervention study, consent was obtained from 1776 (70%) of those invited to participate. All analyses were restricted to the 1623 children of European ethnicity, which was determined from information provided by parents in the 1995 (baseline) questionnaire. A total of 1615 children of European ethnicity had height and weight recorded at age 6. At age 10, a total of 1448 (retention rate of 90%) children were measured, and at age 12, 1116 (69%) children were measured.
Valid z scores (BMI-for-age) were available for analysis for 1598 children who were age 6, 1446 children at age 10, and 1115 children at age 12. Total time spent outdoors was available for analysis for 1488 children who were age 6, 1275 children at age 10, and 1000 children at age 12.
The respective distributions of BMI, gender, ethnicity, and total time spent outdoors at baseline were similar when we compared children with and without follow-up data at age 12 (mean BMI [SD]: 15.9 [1.6] vs 16.1 [1.7] kg/m2; percentage boys: 50.2 vs 57.4; median total time spent outdoors [interquartile range]: 161.3 [112.5, 219.4] vs 157.5 [106.1, 225.0] minutes/day). The percentage of children who had a tertiary-educated parent was slightly higher among those with follow-up data than among those without: 32.5% versus 27.8%. However, parental education was not closely associated with the prevalence of childhood overweight or obesity (data not shown).
Body Size
At age 6, 10.3% and 2.8% of the children were overweight and obese, respectively (Table 1 ▶). These proportions increased markedly by age 10 to 16.3% and 5.7%, respectively; the changes between age 10 and age 12 were smaller. At baseline, children in the high-intervention group had higher z scores and were more likely to be obese than were children in the moderate-intervention and control groups (Table 1 ▶). These differences were also apparent in the primary analysis, in which the adjusted mean z score at baseline was 0.21 (95% confidence interval [CI]=0.10, 0.32) greater in the high-intervention group than in the control group. No differences in the adjusted mean z score at baseline between the moderate-intervention group and control group were observed (Figure 1 ▶). Both the moderate-intervention and control groups had a minimal (nonsignificant) increase in z score over time (change in z score per 1-year increase in age was 0.016 [95% CI = −0.002, 0.034] and 0.009 [95% CI=−0.007, 0.025], respectively); whereas there was a decrease in z score over time for the high-intervention group (change in z score per 1-year increase in age was −0.017 [95% CI=−0.039, 0.005]; Figure 1 ▶; overall P= .067).
TABLE 1—
Distribution of Body Size and Total Time Spent Outdoors, by Age at 6 Years, 10 Years, and 12 Years: The Kidskin Study, Australia, 1995–2001
| 6 Years (Baseline) | 10 Years | 12 Years | |
| Body Size | |||
| Sample size | N = 1598 | n = 1446 | n = 1115 |
| Mean BMI, kg/m2 (SD) | 16.0 (1.6) | 18.2 (3.1) | 19.4 (3.6) |
| Mean z score, BMI-for-age (SD) | |||
| All children | 0.25 (0.92) | 0.29 (0.96) | 0.22 (1.01) |
| High-intervention group | 0.42 (0.93) | 0.35 (0.93) | 0.21 (0.98) |
| Moderate-intervention group | 0.20 (0.87) | 0.27 (0.97) | 0.25 (1.00) |
| Control group | 0.19 (0.94) | 0.28 (0.98) | 0.20 (1.04) |
| Percentage overweight | |||
| All children | 10.3 | 16.3 | 17.2 |
| High-intervention group | 12.6 | 18.3 | 15.8 |
| Moderate-intervention group | 8.8 | 17.5 | 19.8 |
| Control group | 10.1 | 14.5 | 16.2 |
| Percentage obese | |||
| All children | 2.8 | 5.7 | 5.3 |
| High-intervention group | 5.3 | 6.1 | 5.0 |
| Moderate-intervention group | 1.5 | 4.2 | 4.0 |
| Control group | 2.3 | 6.5 | 6.4 |
| Total time spent outdoors | |||
| Sample size | n = 1488 | n = 1275 | n = 1000 |
| Median minutes per day (interquartile range) | |||
| All children | 160.7 (112.5, 221.3) | 117.9 (65.1, 189.6) | 105.5 (53.7, 192.4) |
| High-intervention group | 160.2 (111.4, 215.1) | 104.9 (62.1, 173.6) | 100.0 (52.9, 180.2) |
| Moderate-intervention group | 154.8 (102.6, 213.8) | 121.2 (61.0, 180.3) | 97.1 (51.4, 173.6) |
| Control group | 167.1 (112.5, 228.2) | 129.3 (72.9, 207.5) | 117.6 (55.5, 208.8) |
Note. BMI = body mass index.
FIGURE 1—
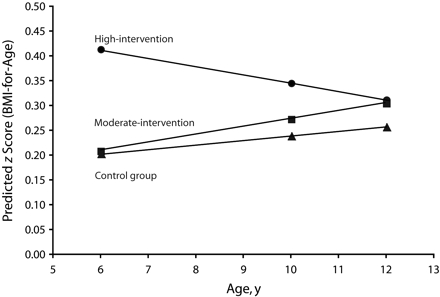
Predicted z scores over time, by level of intervention.
Note. Scores were derived from the linear growth curves, with gender, ethnicity, and parental education set to their baseline distribution.
Table 2 ▶ shows the adjusted mean difference in z scores at age 10 and 12 among the study groups. There were no significant differences between the control and intervention groups.
TABLE 2—
Adjusted Differences in z Scores (BMI-for-Age) and Relative Differences in Total Time Spent Outdoors at Age 10 and 12 Years: The Kidskin Study, Australia, 1995–2001
| 10 Years (95% CI) | 12 Years (95% CI) | |
| Adjusted absolute difference, z score (BMI-for-age)a | n = 1423 | n = 1100 |
| Control group | Reference | Reference |
| Moderate-intervention group | 0.01 (−0.12, 0.14) | 0.05 (−0.09, 0.20) |
| High-intervention group | −0.08 (−0.22, 0.06) | −0.11 (−0.27, 0.05) |
| Adjusted relative difference, total time spent outdoorsb | n = 1177 | n = 921 |
| Control group | Reference | Reference |
| Moderate-intervention group | 1.0 (0.87, 1.15) | 0.94 (0.81, 1.09) |
| High-intervention group | 0.90 (0.78, 1.05) | 0.98 (0.83, 1.15) |
Note. BMI = body mass index; CI = confidence interval. The number of children available for analysis in Tables 1 ▶ and 2 differs because of missing data in the confounders.
aAdjusted for gender, ethnicity, parental educational level, and z score at baseline.
bAdjusted for gender, ethnicity, parental educational level, tendency to sunburn, and total time spent outdoors at baseline. was addressed by the objectives and design of the intervention.
Total Time Spent Outdoors
Overall, children spent between 2 and 3 hours outside every day between 8 am and 5 pm. The distribution of total time spent outdoors by age and study group is presented in Table 1 ▶. As indicated in the “Methods” section, the results for this outcome cannot be compared between years; the appropriate comparison is among the groups in each year. At age 8, the median total time spent outdoors in each of the groups was similar (P= .710; data not shown). There was no association between study group and total time outdoors at either age 10 or age 12 (Table 2 ▶). When group was ignored in the analysis, no association was observed between total time spent outdoors and BMI (data not shown).
The results in Table 2 ▶ for children at age 10 were unchanged when restricted to children for whom we also had data on BMI and time spent outdoors at age (data not shown).
DISCUSSION
The Kidskin sun protection intervention program reduced the amount of time children spent outdoors in the middle of the day during the summer9,13 and was not associated with an increase in BMI. This is reassuring, because it suggests that the program did not lead to a reduction in physical activity—at least relative to dietary energy intake. This interpretation is supported by our previous9 and current findings that the Kidskin intervention was not associated with a reduction in the total time spent outdoors, which indicates that children who received the Kidskin intervention rescheduled their time outdoors to earlier in the day, later in the day, or both. This is clearly a desirable outcome and reflects some of the objectives of the Kidskin intervention program.
Each year, specific program objectives focused on students developing the problem solving, decisionmaking, planning, and goal-setting skills to reduce summer sun exposure, while continuing to engage in their usual leisure activities. The inclusion of home- and classroom-based activities may have increased family support of rescheduling activities to reduce sun exposure. The maintenance of physical activity levels was also supported by the cross-curricular nature of the program. Each year, the curriculum included activities that integrated sun protection and shade games into physical education lessons. Therefore, although maintaining time outdoors was not a specific objective of the Kid-skin program, maintaining physical activity
The proportion of children in the Kidskin intervention cohort who were overweight or obese increased during the course of the study, particularly between ages 6 and 10 years. Another longitudinal study of Australian children20 found an increase in the prevalence of childhood overweight from 15% among children between age 5 and 10 years at baseline in 1997, to 19.7% 3 years later; the prevalence of obesity increased from 4.3% to 4.8% during the same period. That study involved children in a relatively broad age range, and BMI was assessed at only 2 time points; therefore, it is not possible to examine the increase at specific ages. Furthermore, the actual proportions of children in the 2 studies who were overweight or obese are not directly comparable, because children in the Kidskin intervention study were aged 5 or 6 years at baseline, compared with 5 to 10 years in the study by Hesketh et al.20
The Kidskin study has some strengths and limitations. It was a large intervention trial, which had a 4-year intervention period and 2 additional years of follow-up to gauge long-term effects. We collected objective data on sun exposure, nevi, and BMI in a cohort of more than 1000 children who were followed from ages 6 to 12 years. BMI was measured at 3 time points by trained observers and was treated as a continuous variable in the analyses. The study’s large size means that we can be confident about the null findings, and as is apparent from the confidence intervals in Table 2 ▶, the results are consistent with (at most) very small adverse effects on BMI.
The retention rates in this study were high: more than 90% after 4 years and 69% after 6 years. Our results are unlikely to be biased because of loss to follow-up, because the results for BMI at age 10 remained the same, whether or not children followed up to age 12 were included in the analysis. Furthermore, loss to follow-up was not related to BMI at baseline or with any associated variable.
Limitations include lack of randomization14 and baseline differences among the groups. We did not directly assess physical activity among children in the Kidskin study, because that was outside the scope of the study. Nonetheless, time spent outdoors has consistently been correlated with physical activity.8 Time spent outdoors could be considered an indirect measure of physical activity, because it is clearly related to the opportunity to undertake physical activities such as walking, running, cycling, and swimming, which are not as easily or frequently done indoors. Studies of the relation between physical activity and childhood overweight and obesity have used a variety of indirect measures of physical activity, including time spent playing sports or watching television, or time spent in activities that elicit sweating and breathlessness.21 Although findings have been inconsistent, more studies have reported an association than not.21 The reason for the lack of association between total time spent outdoors and BMI in the Kidskin study is not clear, although it may be attributed to our imprecise measurement of time spent outdoors. In addition, we did not have data on children’s nutrient intake and so were unable to adjust for this in our analysis.
To our knowledge, no other published skin cancer prevention intervention has reported the effect of the program on children’s adiposity. However, it is useful to know that it is possible to reduce the time children spend outdoors when ultraviolet radiation is at its highest without producing an unfavorable affect on children’s weight relative to height. Children in the Kidskin intervention study increased their time outdoors at other times of the day, which may, at least partly, explain the absence of any effect on BMI.
A growing number of health issues are becoming the focus of health promotion efforts. Health promoters need to be aware of—and account for—the aims of other programs operating contemporaneously within a given target population.
Acknowledgments
The Kidskin intervention program was funded by the National Health and Medical Research Council (grants 954601, 110221, 209 057) and by the Cancer Foundation of Western Australia. Billie Giles-Corti is supported by a National Health and Medical Research Council/National Heart Foundation Career Development Award (grant 254688).
The authors acknowledge Donna Cross, who contributed to the design and conduct of the study.
Human Participant Protection This study was approved by the human research ethics committees at the University of Western Australia and Curtin University of Technology. Written consent was obtained from the children in the study and their parents.
Peer Reviewed
Contributors E. Milne, D. English, and B. Giles-Corti originated the study and supervised all aspects of its implementation. R. Johnston designed the Kidskin intervention program. J. Simpson undertook the statistical analysis. E. Milne led the writing. All authors helped to conceptualize ideas, interpret findings, and review drafts.
References
- 1.Salmon J, Ball K, Crawford D, et al. Reducing sedentary behavior and increasing physical activity among 10-year-old children: overview and process evaluation of the ‘Switch-Play’ intervention. Health Prom Int. 2005; 20(1):7–17. [DOI] [PubMed] [Google Scholar]
- 2.Ebbeling CB, Pawlak DB, Ludwig DS. Childhood obesity: public-health crisis, common sense cure. Lancet. 2002;360(9331):473–482. [DOI] [PubMed] [Google Scholar]
- 3.Batch JA, Baur LA. Management and prevention of obesity and its complications in children and adolescents. Med J Aust. 2005;182(3):130–135. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Obesity. Preventing and managing the global epidemic. Geneva, Switzerland: World Health Organization; 2000. [PubMed]
- 5.Magnusson J. Childhood obesity: prevention, treatment and recommendations for health. Community Practitioner. 2005;78(4):147–149. [PubMed] [Google Scholar]
- 6.Strock GA, Cottrell ER, Abang AE, Buschbacher RM, Hannon TS. Childhood obesity: a simple equation with complex variables. J Long Term Eff Med Implants. 2005; 15(1):15–32. [DOI] [PubMed] [Google Scholar]
- 7.Buller DB, Borland R. Skin cancer prevention for children: a critical review. Health Education Behavior. 1999;26(3):317–343. [DOI] [PubMed] [Google Scholar]
- 8.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963–975. [DOI] [PubMed] [Google Scholar]
- 9.Milne E, English DR, Johnston R, et al. Improved sun protection behavior in children after two years of the Kidskin intervention. Aust N Z J Public Health. 2000; 24(5):481–487. [DOI] [PubMed] [Google Scholar]
- 10.Milne E, English DR, Johnston R, et al. Reduced sun exposure and tanning in children after two years of school-based intervention. Cancer Causes Control. 2001;12(5):387–393. [DOI] [PubMed] [Google Scholar]
- 11.Milne E, Johnston R, Cross D, Giles-Corti B, English D. Effect of a school-based sun protection intervention on the development of melanocytic nevi in children. Am J Epidemiol. 2002;155(8):739–745. [DOI] [PubMed] [Google Scholar]
- 12.English DR, Milne E, Jacoby P, Giles-Corti B, Cross D, Johnston R. The effect of a school-based sun protection intervention on the development of melanocytic nevi in children: 6-year follow-up. Cancer Epidemiol Biomarkers Prev. 2005;14(4):977–980. [DOI] [PubMed] [Google Scholar]
- 13.Milne E, Jacoby P, Giles-Corti B, Cross D, Johnston R, English DR. The impact of the kidskin sun protection intervention on summer suntan and reported sun exposure: was it sustained? Prev Med. 2006;42(1):14–20. [DOI] [PubMed] [Google Scholar]
- 14.Milne E, English DR, Cross D, Corti B, Costa C, Johnston R. Evaluation of an intervention to reduce sun exposure in children: design and baseline results. Am J Epidemiol. 1999;150:164–173. [DOI] [PubMed] [Google Scholar]
- 15.Education Department of Western Australia. Health Education K-10 Syllabus. Perth, Australia: William C. Brown Printers; 1985.
- 16.Cole TJ. The LMS method for constructing normalized growth standards. Eur J Clin Nutr. 1990; 44(1):45–60. [PubMed] [Google Scholar]
- 17.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data 2000(314):1–27. [PubMed]
- 18.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000; 320(7244):1240–1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vidmar S, Carlin J, Hesketh K, Cole T. Standardizing anthropometric measures in children and adolescents with new functions for EGEN. Stata J. 2004; 4(1):50–55. [Google Scholar]
- 20.Hesketh K, Wake M, Waters E, Carlin J, Crawford D. Stability of body mass index in Australian children: a prospective cohort study across the middle childhood years. Public Health Nutr. 2004;7(2):303–309. [DOI] [PubMed] [Google Scholar]
- 21.Molnar D, Livingstone B. Physical activity in relation to overweight and obesity in children and adolescents. Eur J Pediatr. 2000;159(suppl 1):S45–55. [DOI] [PubMed] [Google Scholar]


