Abstract
We determined the proportion of research on childhood mortality directed toward better medical technology (i.e., by improving old technology or creating new technology) compared with research on technology delivery and utilization. We also estimated mortality reductions from a research-funding strategy focusing primarily on developing technology compared with one that also focused on delivery and utilization.
Ninety-seven percent of grants were for developing new technologies, which could reduce child mortality by 22%. This reduction is one third of what could be achieved if existing technologies were fully utilized.
There is a serious discrepancy between current research and the research needed to save children’s lives. In addition to increased research on the efficacy of treatment, there is an even greater need for increased research on delivery and use of technology.
AN INVESTIGATION undertaken in 2003 for the Bellagio Conference on Child Survival showed that the vast majority of deaths of children younger than 5 years, about 10 million per year, occurred in 42 low-income countries.1 The Bellagio Conference concluded that about two thirds of these could be prevented by interventions currently available and feasible for implementation in these countries.1 Other articles from the conference indicated that the systems for delivering these technologies are seriously deficient2 and that their utilization is inadequate, especially among the poor.3
Before the Bellagio Conference, the international Commission on Health Research for Development drew attention to the imbalance in research addressing ill health in developing countries compared with research on health issues of populations in wealthy, industrialized countries.4 The critical finding from the commission report was that 90% of all research funding for health was devoted to the health problems of industrialized countries, whereas only 10% was for research on the health issues of low-income countries. This issue has received considerable public attention, and the imbalance is now widely referred to as the “10/90 gap.”5
The findings from the Bellagio Conference and global disparities in the allocation of research resources for health issues of populations in developing countries raise other questions about current research priorities: how much research is being directed toward breaking the bottlenecks in delivery and utilization that prevent existing technology from reducing child mortality? If, as we suspect, little such research is performed, how great a reduction in mortality can be expected from new health technologies in the future, given present conditions of utilization and delivery?
We first examined the evidence for another “gap,” namely that between research investments in biological and clinical technology and research investments in delivery and utilization. Second, we estimated mortality reductions from a research funding strategy focusing primarily on the development of better health technologies compared with a strategy also focusing on delivery and utilization. These investigations were based on the premise that research leading to the development of better health technologies will not automatically have an impact on child mortality, because technologies must also be delivered to and used by the children who need them. Achieving improvements throughout this process, from basic scientific discoveries to their utilization, requires scientific research. Applied operations research in the context of health and welfare programs is generally considered to be a national responsibility, but research to obtain general knowledge through theory development and its testing in practice is a global responsibility.
METHODS
To determine the extent to which funded research grants on the causes of childhood mortality in developing countries focused on the development of better health technology versus improvements in health care delivery and utilization, we examined the allocation of research by the National Institutes of Health (NIH) and the Bill and Melinda Gates Foundation, which are the largest public and not-for-profit sources of funds for health research, respectively. We reviewed the research grants funded by both institutions between 2000 and 2004 relating to the major killers of preschool children in developing countries.6
Using the Computer Retrieval of Information on Scientific Projects system (CRISP), we searched the NIH Web site7 for funded studies, employing key words and phrases to identify grants in the system (Table 1 ▶). The CRISP database is maintained by the Office of Extramural Research. We reviewed P (Research Program Projects and Centers), R (Research Projects), and S (Research-Related Program) grants, excluding grants that could not be classified as earmarked for research. Grants with the following numbers were excluded: P30 (center core grants), P41 (biotechnology resource grants), P51 (primate research center grants), P60 (comprehensive center), R13 (conferences), S10 and S11 (biomedical research support), S21 (capacity building), and S22 (educational program). We also excluded all grants whose online abstracts did not provide enough information to enable their classification, as well as grants identified by our key words but clearly not related to the health of children in developing countries (e.g., “smoking and ethanol-induced defects in pneumonia defense”). We reviewed the Bill and Melinda Gates Foundation Web site for Global Health Grants.8 Because the site does not support a keyword search, all grant descriptions were evaluated.
TABLE 1—
Key Words and Phrases Used to Identify Grants in CRISP system
| Disease or Condition | Key Words and Phrases |
| Diarrhea | Diarrhea* |
| Pneumonia | Pneumonia* |
| Malaria | Malaria* |
| HIV/AIDS | (HIV* & maternal*), (HIV* & mother*), (AIDS* & maternal*), (AIDS* & mother*), (breastfeeding* & HIV*), (breast* & feeding* & HIV*), (breastfeeding* & AIDS*), (breast* & feeding* & AIDS*) |
| Measles | Measles* |
| Birth asphyxia | Birth* & asphyxia* |
| Sepsis | (Perinatal* and sepsis*), (neonatal* & sepsis*) |
| Preterm | Preterm* |
| Tetanus | Tetanus* |
| Undernutrition | “Complementary feeding*”, “complementary food*” Micronutrient*, “micro nutrient*” Malnutrition*, undernutrition*, “under nutrition*” |
Note. CRISP = Computer Retrieval of Information on Scientific Projects; * = truncation.
To code the information, we set up a simple classification system for the objectives of each study: (1) category A, predelivery research; (2) category B, efficacy trials; (3) category C, diagnosis; or (4) category D, delivery and utilization research. Predelivery studies (category A) were classified as those studies aimed at the identification and characterization of diseases and conditions, the description of their clinical and functional impact, or the development of preventive or curative technologies. We counted efficacy trials (category B) separately because they often could not be clearly classified as either category A or D. The rationale for creating a separate category for diagnosis research (category C) was that the delivery of health care often requires diagnosis. Most of the diagnosis research funded by the NIH appeared to be of little relevance to child health in developing countries but might have future relevance, and these studies were therefore separated from other categories. When a grant investigated more than 1 category, we listed it under each relevant category; therefore, the sum of the number of grants listed under all categories is higher than the actual total number of grants. However, as very few grants addressed more than 1 category, we refer to the category sums as if they were the sums of the grants.
To determine the probable impact on child mortality of continuing to focus future research primarily on developing better technologies compared with expanding the scope of research on improving the delivery and use of current technology, we began with a list of the major causes of child mortality (Table 2 ▶, first column) and the proportion each contributed to total mortality (second column) according to Black et al.6 In principle, mortality could be reduced by expanding the use of existing technology, developing new, more effective technologies, or by a combination of the 2 approaches.
TABLE 2—
Potential for Decreasing Mortality Among Children Aged Younger Than 5 Years in the 42 Countries That Account for 90% of Such Deaths Worldwide
| Cause-Specific Deaths That Could Be Averted, % | Potential Deaths Averted as Proportion of All Deaths, % | ||||
| Cause of Mortality | Percentage of All Deathsa | Improving Utilization With Efficacy of Technology Constanta | Improving Efficacy of Technology With Utilization Constantb | With Technology Constantc | With Utilization Constantd |
| Diarrhea | 22 | 88 | 40 | 19.5 | 8.9 |
| Pneumonia | 21 | 65 | 29 | 13.7 | 6.2 |
| Malaria | 9 | 91 | 23 | 8.6 | 2.1 |
| HIV/AIDS | 3 | 48 | 3 | 1.6 | 0.1 |
| Measles | 1 | 100 | 10 | 1.1 | 0.1 |
| Birth asphyxia | 10 | 39 | 2 | 3.7 | 0.2 |
| Sepsis | 8 | 94 | 18 | 7.8 | 1.4 |
| Preterm | 8 | 59 | 19 | 4.7 | 1.5 |
| Tetanus | 2 | 81 | 46 | 1.9 | 1.1 |
| Other neonatal | 5 | 0 | 0 | 0.0 | 0.0 |
| Other postneonatal | 10 | 0 | 0 | 0.0 | 0.0 |
| Total | 100 | 62.5 | 21.5 | ||
aCalculations based on data are from Jones et al.1
bMethod of calculation is explained in “Methods” section (equation 2).
cPercentages from second column multiplied by percentages from third column. dPercentages from second column multiplied by percentages from fourth column.
For each disease and condition in Table 2 ▶, Jones et al.1 identified available technologies that were potentially feasible for widespread delivery in low-income countries and ascertained their efficacy in reducing mortality. Missing from Table 2 ▶ is malnutrition, which accounted for more than half of postneonatal child deaths because it increases mortality from infectious diseases.9–11 It would therefore be more appropriate to show the proportion of all deaths caused by malnutrition in the second column of Table 2 ▶. The high proportion of children whose lives could be saved by preventing malnutrition highlights the importance of nutrition interventions in the armamentarium of strategies to reduce mortality. For the sake of consistency with previous publications, however, we have retained the original list (without malnutrition).
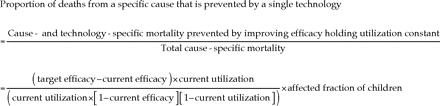
Building on the work of Jones et at.1, we then estimated how many child deaths in the 42 low-income countries identified in the Bellagio Conference could have been averted by developing better technologies if they were used at the rates then used for existing technologies. These averted deaths were calculated using equation 1:
(1) See equation box.
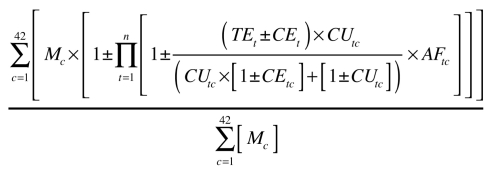
The “affected fraction” in equation 1 indicates the proportion of deaths for each cause that could be averted with a specific technology. For example, vitamin A was assumed to have an effect only on children aged 6 to 59 months who were deficient in this vitamin.1 We used equation 1 sequentially for all technologies that addressed the same cause, applying the equation to the remaining cause-specific mortality as shown in the product term of equation 2. This equation was used to calculate the proportion of total cause-specific child deaths that could be averted by improving efficacy and holding utilization constant. The Φ(1 – deaths prevented) part of the equation ensures that children’s lives are counted as saved only once.
(2) See equation box.
With Mc =cause-specific mortality in country
CUtc =current utilization of technology t in country c
TEt =target efficacy of technology t
CEt =current efficacy of technology t
AFtc =affected fraction specific to technology t and country c
n =total number of cause-specific treatments
To calculate the proportion of deaths relative to total deaths that could have been averted with technology that was 100% effective if it were delivered and used at existing rates, we multiplied the proportion calculated with equation 2 by the cause-specific proportion of all deaths.
RESULTS
In 2001, an estimated US $106 billion was spent globally on health research and development, roughly half of which came from the public sector. The US government alone spent US $28.6 billion, or almost three fifths of global public sector expenditures. Over 70% of the US government’s expenditure (US $20.5 billion) was provided by the NIH. Among the not-for-profit sources of funding for global health initiatives (including health research), the Bill and Melinda Gates Foundation was by far the top funder.12 The 2 institutions thus represent an influential proportion of research funding for health in developing countries.
Of the 994 NIH grants identified by the search, 649 were deemed relevant. Of these grants, 625 were classified in category A (predelivery research), 24 in category B (efficacy trials), 19 in category C (diagnostics research), and 17 in category D (delivery and utilization). The proportion of grants funded by the NIH on delivery and utilization issues (3%) was very low compared with the rest of research relevant to the diseases and conditions that kill children in developing countries.
Among the 435 global health grants funded by the Bill and Melinda Gates Foundation, 53 grants (12%) were directed toward research on malnutrition or the diseases and conditions listed in Table 2 ▶. Of these 53 grants, 34 were classified in category A, 12 in category B, 4 in category C, and 12 in category D. Thus, among the research grants funded by the Bill and Melinda Gates Foundation that were directed at the primary diseases and conditions that kill children, only one fourth focused on delivery and utilization.
In summary, from 2000 to 2004 most of the research grants awarded by the NIH and Bill and Melinda Gates Foundation went to predelivery research, whereas no more than 3% of NIH grants and 23% of Bill and Melinda Gates Foundation grants were pertinent to research on delivery and utilization. Given that the total budget appropriated by the NIH in 2001 was more than 40 times larger than the total research resources provided by the Bill and Melinda Gates Foundation, the proportion of research on health care delivery and utilization is much closer to the 3% estimate. The relative funding of health research from other agencies (such as bilateral and multilateral donors) was small compared with the combined budgets of the Bill and Melinda Gates Foundation and the NIH,13 although the proportion allocated to research on delivery and utilization by these agencies was likely to be higher because of their mission. This is more than counterbalanced by the fact that half of all health research is funded by the private sector, which has little incentive to invest in research on health care delivery and utilization because the results cannot be patented.
The fourth column in Table 2 ▶ shows our estimates of the proportion of deaths, by cause, that could have been be averted by improving the efficacy of technology to 100%. The sixth column, which is the product of the second and third columns, presents the proportion of deaths relative to total deaths that could have been averted with technology that was 100% effective if that technology were delivered and used at existing rates. The sixth column sums to 21.5%, which is the percentage of all child deaths per year (i.e., 2 million) that would be prevented by optimizing the efficacy of technology alone.
Comparing the third and fourth columns shows that for each cause of death, improving the efficacy of health technology would save considerably fewer lives than improving the delivery and use of existing technology. For some causes of death, the sum of these 2 columns is more than 100%. This is because a child’s life could be saved by either increased efficacy or increased use of technology if either were improved and could not be saved twice if both were improved simultaneously. The very limited effect of improving the efficacy of technology on lowering mortality rates from HIV/AIDS or birth asphyxia is a consequence of the low availability of the technologies addressing these causes.
DISCUSSION
We made some approximations and assumptions to calculate our estimates. For example, because of the limited information available on the Bill and Melinda Gates Foundation Web site for Global Health Grants, a small number of grants may have been misclassified. In the calculations of relative impact on mortality rates, we assumed conditions of ideal utilization and maximally efficacious technology. Would changing this approximation or assumption significantly alter the results? The magnitude of the differences is so large that even major changes in the estimates would have little effect on the conclusion that there is a major imbalance between the proportion of lives that could be saved by improving delivery and use of health technology compared with creating new technology (62.5% and 21.5%, respectively) and the relative proportion of grants funded in the 2 areas (3% and 97%). We call this latter imbalance the “3/97 gap.”
The analyses presented in Table 2 ▶ raise serious questions about the wisdom of continuing the current funding policy. On the one hand, the benefits that have accrued from past investments in health technology research are clear. Future investments will continue to bear fruit, and it is critical that such investments continue. On the other hand, the effects of the failure to invest in research on delivery and implementation are also clear. Extrapolating to the future, it appears that only one fifth of child deaths per year (i.e., 2 million) are likely to be prevented by continuing to improve health technology alone. This figure is in sharp contrast to the 6 million deaths per year that could be prevented by optimizing the delivery and use of currently available technology.
The rationale for our proposition—that increasing research on the delivery and use of health technologies will make it possible to realize the potential of current technologies—is based on several arguments. First, the current problems in delivery and utilization are not inherent in the technologies themselves. Second, although a lack of adequate economic investment is an important factor, the current problems in utilization and delivery are not wholly because of a lack of economic investments to ensure their availability. Finally, research on delivery and use of technology can yield insights that lead to new strategies for identifying and breaking the bottlenecks that prevent current technologies from achieving their potential.
Regarding the first argument, there is ample evidence to support the proposition that the vast majority of currently available safe and effective technologies can be delivered and utilized. Across the world, health care workers with limited education and minimal training have been taught to safely inject antibiotics and vaccines. Teaching health care workers how to administer oral measles vaccine and vitamin A capsules safely has not been a significant barrier to the delivery of these life-saving technologies. What has proved much more difficult has been the logistics of the delivery of supplies and deployment of personnel, and the systematic application of these technologies through health services and other channels.14,15
There is strong evidence that families can use currently efficacious life-saving technologies when they receive appropriate teaching and support.16,17 Moreover, when families use these technologies—for example, packaged or home-prepared oral rehydration therapy or other home-prepared fluids to help control diarrhea—the results are reduced mortality rates; this has been shown for diarrheal disease on all continents.18 Programs to encourage and support breast-feeding provide another example of critical life-saving “technology.” Such programs have not encountered insurmountable technical barriers and have been successful in promoting exclusive breast-feeding in populations not normally practicing it.19 Even mal-nourished women can exclusively breastfeed, at least for 4 months, when they are given minimal counseling.20
The second argument, that problems of delivery and utilization are not wholly caused by lack of economic resources, rests on interpretation of the word wholly. On the one hand, increasing health sector funding would have major, positive effects on reducing mortality. On the other hand, there is evidence that countries with similar levels of economic development and health expenditures have substantially different levels of health.21 It can therefore be inferred that factors other than economic resources are making the difference. These factors range from culture, governance, and the political will to use the resources well to bureaucratic and market structures delivering the interventions to household and individual behavior in both accessing interventions and complying with good health practices.
The third argument is the proposition that problems in these aspects of health care are inherently researchable, that there are research methods presently available to address them (e.g., see Gove et al.22), and that such research provides insights and guidance on breaking the bottlenecks that prevent current technologies from achieving their potential.23 There is substantial evidence from research by medical anthropologists, sociologists, and nutritionists documenting the potentially modifiable social, cultural, and behavioral barriers impeding the full and effective delivery and utilization of these and other existing technologies.24–27 Moreover, there is also clear evidence that delivery and utilization can be signficantly improved through appropriate interventions.28–30
There is substantial technical capacity to address these issues in the fields of social science and public health research, although development of a critical mass of investigators is urgently needed. The research agenda would focus not only on obtaining a better understanding of why the policy decisions and bureaucratic and household behaviors do not conform to expectations but also on developing theoretical frameworks that inform—and are informed by—intervention.
An additional argument for increasing research on the delivery and use of technology is the probability that new technologies will encounter the same barriers that have prevented current ones from achieving their potential. Research that leads to better delivery and use of current technologies will facilitate the planning and implementation of activities to introduce and institutionalize new technologies.
CONCLUSIONS
Our quantification of research grant allocation shows that within the general research disparity articulated in the 10/90 gap is another serious, compounding gap. Only a small proportion of funded research designed to help reduce child mortality is directed towards doing so in low-income countries, and very little of that research concerns health care delivery and utilization. It is time to also recognize the “3/97 gap” and begin to take steps to correct it by investing adequate resources for research on the delivery and use of technology to help reduce the remaining burden of childhood mortality.
Acknowledgments
This work was partially funded by the Howard Hughes Medical Institute through a fellowship to J. L. Leroy.
Juan Rivera and Jennifer Bryce provided useful comments on earlier drafts of this article. We acknowledge an anonymous reviewer for her/his contribution in clarifying our thinking about the implications of our findings.
Human Participant Protection No human subjects were involved in the study.
Peer Reviewed
Contributors All authors participated in the conception of the study, the interpretation of the data, and the writing of the manuscript. J. L. Leroy was responsible for the data analyses.
References
- 1.Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year? Lancet. 2003;362:65–71. [DOI] [PubMed] [Google Scholar]
- 2.Bryce J, el Arifeen S, Pariyo G, Lanata C, Gwatkin D, Habicht JP. Reducing child mortality: can public health deliver? Lancet. 2003;362:159–164. [DOI] [PubMed] [Google Scholar]
- 3.Victora CG, Wagstaff A, Schellen-berg JA, Gwatkin D, Claeson M, Habicht JP. Applying an equity lens to child health and mortality: more of the same is not enough. Lancet. 2003;362:233–241. [DOI] [PubMed] [Google Scholar]
- 4.Commission on Health Research for Development. Health Research: Essential Link to Equity in Development. New York, NY: Oxford University Press; 1990.
- 5.Global Forum for Health Research. The 10/90 Report on Health Research. 2003–2004. Geneva, Switzerland: Global Forum for Health Research, 2004.
- 6.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361: 2226–2234. [DOI] [PubMed] [Google Scholar]
- 7.National Institutes of Health. Computer Retrieval of Information on Scientific Projects. Available at: http://crisp.cit.nih.gov. Accessed on February 1, 2005.
- 8.Bill and Melinda Gates Foundation. Available at: http://www.gatesfoundation.com. Accessed on February 1, 2005.
- 9.Pelletier DL, Frongillo EA, Jr., Habicht JP. Epidemiologic evidence for a potentiating effect of malnutrition on child mortality. Am J Public Health. 1993;83:1130–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pelletier DL, Frongillo EA Jr, Schroeder DG, Habicht JP. The effects of malnutrition on child mortality in developing countries. Bull World Health Organ. 1995;73:443–448. [PMC free article] [PubMed] [Google Scholar]
- 11.Fishman SM, Caulfield LE, de Onis M, et al. Childhood and maternal underweight. In: Ezzati M, Lopez AD, Rodgers A, Murray CJL, eds. Comparative Quantification of Health Risks: The Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Geneva, Switzerland: World Health Organization; 2004:39–161.
- 12.Global Forum for Health Research. The 10/90 Report on Health Research. 2001–2002. Geneva, Switzerland: Global Forum for Health Research, 2002.
- 13.Global Forum for Health Research. Monitoring Financial Flows for Health Research. Geneva, Switzerland: Global Health Forum; 2004.
- 14.Bryce J, Victora CG, Habicht JP, Black RE, Scherpbier RW, and MCE-IMCI Technical Advisors. Programmatic pathways to child survival: results of a multi-country evaluation of Integrated Management of Childhood Illness. Health Policy Plan. 2005;20(suppl 1):i5–i17. [DOI] [PubMed] [Google Scholar]
- 15.Gouws E, Bryce J, Pariyo G, Armstrong Schellenberg J, Amaral J, Habicht JP. Measuring the quality of child health care at first-level facilities. Soc Sci Med. 2005;61:613–625. [DOI] [PubMed] [Google Scholar]
- 16.Chowdhury AM, Karim F, Ahmed J. Teaching ORT to women: individually or in groups? J Trop Med Hyg. 1988;91: 283–287. [PubMed] [Google Scholar]
- 17.Suarez De Balcazar Y, Balcazar FE. Child survival in the Third World: a functional analysis of oral rehydration therapy dissemination campaigns. Behav Change. 1991;8:26–34. [DOI] [PubMed] [Google Scholar]
- 18.Victora CG, Bryce J, Fontaine O, Monasch R. Reducing deaths from diarrhoea through oral rehydration therapy. Bull World Health Organ. 2000;78: 1246–1255. [PMC free article] [PubMed] [Google Scholar]
- 19.Quinn VJ, Guyon AB, Schubert JW, Stone-Jimenez M, Hainsworth MD, Martin LH. Improving breastfeeding practices on a broad scale at the community level: success stories from Africa and Latin America. J Hum Lact. 2005; 21:345–354. [DOI] [PubMed] [Google Scholar]
- 20.Gonzalez-Cossio T, Habicht JP, Rasmussen KM, Delgado HL. Impact of food supplementation during lactation on infant breast-milk intake and on the proportion of infants exclusively breastfed. J Nutr. 1998;128:1692–1702. [DOI] [PubMed] [Google Scholar]
- 21.Filmer D, Pritchett LH. Child mortality and public spending on health: how much does money matter? Washington, DC: World Bank. Development Research Group; 1997.
- 22.Gove S, Pelto GH. Focused ethnographic studies in the WHO Programme for the Control of Acute Respiratory Infections. Med Anthropol. 1994;15: 409–424. [DOI] [PubMed] [Google Scholar]
- 23.de Zoysa I, Habicht JP, Pelto G, Martines J. Research steps in the development and evaluation of public health interventions. Bull World Health Organ. 1998;76:127–133. [PMC free article] [PubMed] [Google Scholar]
- 24.Hahn RA, ed. Anthropology in Public Health: Bridging Differences in Culture and Society. New York, NY: Oxford University Press, 1999.
- 25.Kasper JD. Health-care utilization and barriers to health care. In: Albrecht GL, Fitzpatrick R, Scrimshaw SC, eds. The Handbook of Social Studies in Health & Medicine. London, England, and Thousand Oaks, Calif: Sage Publications Inc; 2000.
- 26.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 27.Fiscella K, Franks P, Clancy CM. Skepticism toward medical care and health care utilization. Med Care. 1998; 36:180–189. [DOI] [PubMed] [Google Scholar]
- 28.Santos I, Victora CG, Martines J, et al. Nutrition counseling increases weight gain among Brazilian children. J Nutr. 2001;131:2866–2873. [DOI] [PubMed] [Google Scholar]
- 29.Rivera JA, Sotres-Alvarez D, Habicht JP, Shamah T, Villalpando S. Impact of the Mexican program for education, health, and nutrition (Progresa) on rates of growth and anemia in infants and young children: a randomized effectiveness study. JAMA. 2004;291:2563–2570. [DOI] [PubMed] [Google Scholar]
- 30.Bryce J, Gouws E, Adam T, et al. Improving quality and efficiency of facility-based child health care through Integrated Management of Childhood Illness in Tanzania. Health Policy Plan. 2005;20(suppl 1):i69–i76. [DOI] [PubMed] [Google Scholar]


