Abstract
Objectives. Evidence regarding the long-term impact of health and other community development programs on under-5 mortality (the risk of death from birth until the fifth birthday) is limited. We compared mortality in a population served by health and other community development programs at the Hôpital Albert Schweitzer (HAS) with national mortality rates among children younger than 5 years for Haiti between 1958 and 1999.
Methods. We collected information on births and deaths in the HAS service area between 1995 and 1999 and assembled previously published under-5 mortality rates at HAS. Published national rates for Haiti served as a comparison.
Results. In the early 1970s, the under-5 mortality rate at HAS declined to a level three fourths lower than that in Haiti nationwide. More recently, HAS rates have remained at one half those for Haiti nationwide. Child survival interventions in the HAS service area were substantially higher than in Haiti nationwide although socioeconomic characteristics and levels of childhood malnutrition were similar in both areas.
Conclusions. HAS’s programs have been responsible for long-term sustained reduction in mortality among children aged less than 5 years. Integrated systems for health and other community development programs could be an effective strategy for achieving the United Nations Millennium Goal to reduce under-5 mortality two thirds by 2015.
During the past half-century, numerous advances in medicine and public health have been introduced into local health programs throughout the world. The under-5 mortality rate (the risk of death from birth until the fifth birthday) in developing countries fell by 47% (from 167 deaths per 1000 live births to 89 deaths per 1000 live births) between 1970 and 2001.1,2 The degree to which this decline can be attributed to local health programs is not well understood.3,4
It appears that a strong direct causal relation exists between program funding, staffing resources, and facilities (inputs); services and advances in knowledge and practice within programs (processes); expansion of programs (outputs); and declines in mortality rates among children younger than 5 years (impacts). Although there is substantial evidence to support the short-term efficacy of specific interventions in controlled settings,5 the evidence for a direct causal relation between the services of ongoing, long-term local programs and long-term declines in under-5 mortality in developing countries is strikingly limited. Numerous studies over the past half-century have documented that multiple underlying socioeconomic and demographic factors, generally independent of local programs, exert a strong influence on under-5 mortality.6–9
We recently reported evidence that links inputs, processes, and outputs to under-5 mortality at the Hôpital Albert Schweitzer (HAS) between 1995 and 1999.10 Here, we report the long-term trends of under-5 mortality in the HAS service area between 1958 and 1999. We summarized the findings of previously published studies on under-5 mortality at HAS, added findings from the most recent mortality assessment, and compared these findings with those for Haiti at large. We also summarized the evidence in support of the conclusion that lower mortality rates in the HAS service area can be attributed to HAS programs.
HAS is a local system of health and other community development programs in the Artibonite Valley of Haiti, which has been serving a rural population of mostly subsistence farmers since 1956.11 This system has gradually evolved over the past half-century from what was initially only a hospital. Between 1956 and 1967, HAS provided immunizations at its outpatient clinic and ran a program that taught local midwives to sterilize instruments that were used to cut umbilical cords during childbirth. Sick children were admitted to the hospital, and mothers of children with signs of kwashiorkor were encouraged to bring their children to the hospital. In the late 1960s, HAS established a program of community-based primary health care, which was closely integrated with the hospital’s inpatient services, as well as a program of community development activities. Since then, HAS health and other community development programs have gradually expanded. A recent description of HAS programs and services has been published elsewhere.10
Today, HAS provides community-based primary health care services to a population of 148 000 persons in 7 functional units of the health district (Unite Communale de Sante [UCS]) of Petite Riviere, Verettes, and LaChapelle. The UCS has a total of 258 000 residents in 14 functional units. Primary health care services in the other 7 functional units are now provided by other nongovernmental organizations and the Haitian Ministry of Health. However, up until 1996, HAS provided primary health care services in all 14 functional units to a population estimated at 180 000 persons.
METHODS
In late 1999 and early 2000, specially trained interviewers carried out a household survey of 3427 women of reproductive age in the 7 HAS functional units (hereafter referred to as the HAS service area). The women interviewed represented a 10% sample of the total women of reproductive age. They were selected at random from a computerized list of households maintained by the health information system of the HAS Community Health Division. This master list is based on lists of households maintained by health agents, who visit each home every 1–3 months. The master list is updated in the computerized central system every 6 months. The questionnaire used to collect birth history information is identical to that used for the birth history component of the 1999 demographic and health survey in Haiti.12 This questionnaire asks the respondents for information about the date for each of the respondent’s offspring, whether the birth produced a boy or girl, whether the child is still living, the current age of the child, whether the child is living at home or elsewhere, and if the child died, the child’s age at death.
Two of the authors (H. P. and F. P.) trained the interviewers using a 4-day program and 1 of the authors (F. P.) provided close field supervision and daily review of the collected data. The survey was carried out in accordance with ethical guidelines present at HAS at that time, and participants were given the opportunity not to respond after receiving an explanation of why they were being interviewed and how the information would be used. The collected data were transferred into Epi Info version 6.04d (Centers for Disease Control and Prevention, Atlanta, Ga) for analysis. From these data, mortality rates were calculated for the periods 1985–1989, 1990–1994, and 1995–1999.
The risk of death from birth until the first birthday (1q0) was approximated using the infant mortality rate: the number of infant deaths during the time period was divided by the number of live births during the same period. The 1–4 year mortality rate is the risk of death from the first birthday until the fifth birthday (4q1). This was approximated by dividing the number of deaths from the first to the fifth birthdays during the time period by the difference between the number of births and the number of deaths during the first year. The under-5 mortality rate is the risk of death from birth until the fifth birthday (5q0). This was approximated by determining the number of under-5 deaths during the time period and dividing by the number of live births. The relation between these rates is
 |
(1) |
All rates are expressed per 1000.
For some of the references cited, 1–4 year mortality rates were reported as the number of deaths per 1000 population of that age group per year (4m1). This was converted to 4q1 by using the formula
 |
(2) |
The findings from the analysis of the most recent HAS survey data were then compared with those from previously published studies on under-5 mortality rates between 1958 and 1992 in the HAS service area13–15 and for Haiti nationwide from 1970 to 1999.12,16–18 For the periods 1980–1984, 1985–1989, and 1990–1994, there are estimates from the 2 previous national demographic and health surveys (1994–1995 and 2000).12,18 We report the estimate that was obtained closest to the time of data collection. In Table 1 ▶, we show 2 estimates for under-5 mortality at HAS for the period 1990–1994.
TABLE 1—
Infant and Child Mortality Rates in the Hôpital Albert Schweitzer (HAS) Primary Health Care Service Area and Among the HAS Service Population: Haiti, 1958–1999
| Infant Mortality Ratea | 1–4 Year Mortality Rateb | Under-5 Mortality Ratec | ||||||||
| Haiti | Haiti | Haiti | ||||||||
| Year | HAS Service Population (Children Under 5) | HAS | National | Rural | HAS | National | Rural | HAS | National | Rural |
| 1958–1962 | 8820 (1305)d | 174.0d | 91.5d,e | 249.6d | ||||||
| 1963–1967 | 8820 (1305)d | 110.0d | 54.5d,e | 158.5d | ||||||
| 1968–1972 | 48.0d | 29.9d,e | 76.5d | |||||||
| 1970 | 47.0d | 147.0f | 35.4d,e | 123.7f | 80.7d | 252.5f | ||||
| 1972 | 60 000 (8880)g | 34.0d | 23.7d,e | 56.9d | ||||||
| 1971–1973 | 150.0h | 87.9h | 224.7h | |||||||
| 1975–1979 | 137.3i | 77.0i | 203.7i | |||||||
| 1980–1984 | 138 000 (20 424)j | 120.0i | 76.1i | 175.6i | ||||||
| 1985–1989 | 150 000 (22 200)j | 39.2k | 101.4i | 24.0k | 55.5i | 62.3k | 151.2i | |||
| 1985–1995 | 88.9i | 60.8i | 144.3i | |||||||
| 1992 | 33.0l | 15.9l | 48.4l | |||||||
| 1990–1994 | 165 000 (24 420)j | 42.4k | 73.9i | 25.1k | 61.2i | 66.4k | 130.6i | |||
| 1990–1999 | 91.0m | 64.8m | 149.4m | |||||||
| 1996 | 180 000 (26 640)j | |||||||||
| 1995–1999 | 47.3k | 80.3m | 15.8k | 41.7m | 62.3m | 118.6m | ||||
aEstimate of the probability of death between birth and the first birthday (1q0) multiplied by 1000. See the “Methods” section for further details.
bEstimate of the probability of death between 1 and the fifth birthday (4q1) multiplied by 1000. The 1–4 year mortality rate used is the average risk of death over a 4-year period, which was present for the period of time indicated in column 1. See the “Methods” section for further details.
cEstimate of the probability of death between birth and 5 years of age [5q0 = 1 − (1 − 1q0)(1 − 4q1)]. See the “Methods” section for further details.
eThe number of deaths per year per 1000 children aged 1.0–4.9 years, 4m1, was converted to 4q1. See the “Methods” section for further details.
fInstitut Haitien de Statistiques.16
gBerggren et al.13
hAllman.17
iCayemittes.18
j W. Berggren and G. Berggren, personal communication, 2004.
kHAS birth history survey, 2000.
lBerggren.14
m Cayemittes.12
Whenever possible, we have computed 95% confidence intervals for the mortality rate estimates. In all cases except 2, these were computed using Computer Programs for Epidemiologists, PEPI version 4.0.19 The national estimates for the periods 1990–1994 and 1995–1999 had been previously calculated and reported.12,18 The number of births and deaths for rural Haiti from 1990 to 1999 were estimated from additional data provided by ORC Macro, a research company based in Calverton, Maryland (B. Barrère, BS, Macro International, personal communication, 2006).
RESULTS
Table 1 ▶ and Figures 1 ▶ and 2 ▶ show that, for more than 3 decades, the infant and 1–4 year mortality rates in the HAS service area have been substantially lower than rates for similar age groups in Haiti as a whole. In the HAS service area, infant and 1–4 year mortality rates declined rapidly between 1958 and 1970 and remained at a relatively low level through 1999. Under-5 mortality in the HAS service area fell from 249.6 deaths per 1000 live births in the period 1958–1962 to 56.9 deaths per 1000 live births in 1972 and continued in that range until 1995–1999. Infant mortality at HAS fell from 174.0 deaths per 1000 live births during 1958–1962, to 34.0 deaths per 1000 live births in 1972 and continued in that range until 1995–1999. The 1–4 years mortality rates show a similar pattern, with a marked drop from 91.5 deaths per 1000 children reaching their first birthday in the period 1958–1962, to 23.7 deaths per 1000 live births in 1972, and further decline to 15.8 deaths in the period 1995–1999.
FIGURE 1—
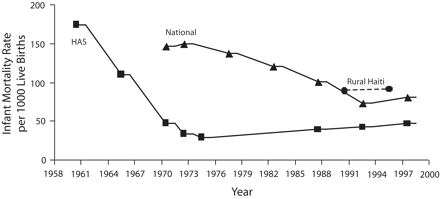
Long-term trends in infant 0–11 month mortality in Haiti and in the primary health care service area of Hôpital Albert Schweitzer, 1958–1999.
Source. HAS birth history survey, 2000, and Cayemittes et al.12,18
Note. Mortality rates for rural Haiti were not available before 1985.
FIGURE 2—
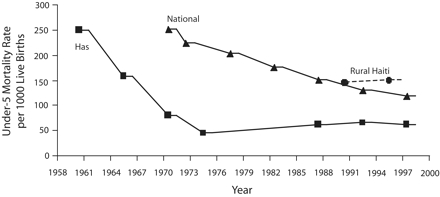
Long-term trends in under-5 mortality rates in Haiti and in the primary health care service area of the Hôpital Albert Schweitzer, 1958–1999.
Source. HAS birth history survey, 2000, and Cayemittes et al.12,18 Note. Rates refer to the total risk of death over a 5-year period, from birth to 59 months of age. Mortality rates for rural Haiti were not available before 1985.
The under-5 mortality rate for Haiti as a whole has declined much more gradually over this same period, beginning at what presumably was a level similar to that in the HAS service area in 1956. Although actual data for Haiti as a whole are not available before 1970, extrapolation of the mortality rates in Figure 2 ▶ to earlier time periods suggests that the under-5 mortality for Haiti would have been similar to that at HAS. Remarkably, infant and child mortality rates for Haiti at large continued to decline even in the face of economic deterioration and political instability during the 1990s. For the 1995–1999 period, the national infant mortality rate for Haiti was 1.7-times greater than that in the HAS service area, and the 1–4 year mortality rate was 2.6-times greater than in the HAS service area.
The median of the 95% confidence intervals for the mortality rates in the HAS service area (Table 2 ▶) is 19.4% of the rates themselves and for the national rates 9.7%. In all cases in which it was possible to measure confidence intervals, the differences between the rates for the HAS service area and the national rates for Haiti for the same or similar period are statistically significant.
TABLE 2—
Numbers of Births and Deaths by Age Group and Mortality Rates for the HAS Primary Health Care Service Area and for Haiti: 1971–1999.
| Period | Geographic Area | Births | Infant Deaths During Period | Deaths Among Children 1–4 Years | Deaths Among Children Younger Than 5 Years | Infant Mortality Rate (95% CI)a | 1–4 year Mortality Rate (95% CI)b | Under-5 Mortality Rate (95% CI)c | Data Source |
| 1971–1973 | Haiti | 134 900d | 20 242d | 12 805d | 33 047d | 150.0 (148.1, 151.9) | 87.9 (86.3, 89.5) | 224.7 (220.2, 229.2) | Allman17 |
| 1985–1989 | HAS | 1507 | 59 | 35 | 94 | 39.2 (29.9, 50.2) | 24.0 (16.9, 33.5) | 62.3 (50.1, 75.1) | HAS birth history survey, 2000 |
| 1990–1994 | HAS | 2120 | 92 | 40 | 132 | 42.4 (34.3,51.9) | 25.1 (18.8,32.9) | 66.4 (56.3,78.0) | HAS birth history survey, 2000 |
| 1990–1994 | Haiti | NA | NA | NA | NA | 73.9 (63.2,84.7) | 61.2 (50.0,72.5) | 130.6 (115.6,145.7) | Cayemittes18 |
| 1990–1999 | Haiti (rural) | 8813d | 802d | 495d | 1297d | 91.0 (85.1,97.2) | 64.8 (59.5,70.4) | 149.4 (142.1,157.1) | Cayemittes12 |
| 1995–1999 | Haiti | 8132d | 653d | 312 | 964d | 80.3 (68.7,92.0) | 41.7 (32.1,51.2) | 118.6 (101.7,135.6) | Cayemittes12 |
| 1995–1999 | HAS | 2393 | 113 | 36 | 149 | 47.3 (39.1,56.5) | 15.7 (11.1,21.8) | 62.3 (52.9,72.7) | HAS birth history survey, 2000 |
Note: CI = confidence interval; HAS = Hôpital Albert Schweitzer; NA = not available.
aEstimate of the probability of death between birth and the first birthday (1q0) multiplied by 1000. See the “Methods” section for further details.
bEstimate of the probability of death between 1 and the fifth birthday (4q1) multiplied by 1000. The 1–4 year mortality rate used is the average risk of death over a 4-year period, which was present for the period of time indicated in column 1. See the “Methods” section for further details.
cEstimate of the probability of death between birth and 5 years of age [5q0 = 1 − (1 − 1q0)(1 − 4q1)]. See the “Methods” section for further details.
dEstimated from available data.
The population of the HAS service area has gradually increased during the period of observation as a result of population growth and expansion of the geographic area of service. We have conservatively estimated the population of the HAS service area where measurements of mortality took place (Table 1 ▶). However, HAS also provided services in adjacent geographic areas not included in our mortality assessment.
DISCUSSION
Our findings indicate that infant mortality rates, 1–4 year mortality rates, and 0–4 year mortality rates in the population served by HAS have remained substantially less than those for Haiti as a whole over a period of 3 decades. In fact, in the early 1970s when comparisons were first available, the rate at HAS was only one quarter of that for Haiti as a whole. Even though HAS rates have remained relatively unchanged since 1970, the rates for the HAS service area in 1995–1999 were still approximately half as great as those nationally during that same time period. Furthermore, these mortality rates remained low during the period from 1968 until 1996, when the HAS service area gradually expanded from 8820 to 180 000 people.
These findings raise the question of whether the observed differences in mortality can be attributed to the programs provided by HAS. Elsewhere10 we have assessed the level of inputs (health staff resources and health facilities), service use (number of home visits, nutritional evaluations of children, ambulatory visits, and hospital admissions as well as number of community development activities), and outputs (coverage of key child survival services) in the year 2000 and in the 5 to 10 years before that.
An extensive staff and facility infrastructure is in place and has been stable during the previous 4 decades. HAS provides a high volume of community outreach, ambulatory, and inpatient services, as well as a substantial variety of community development activities. The coverage of key child survival services (immunizations, vitamin A distribution, treatment of diarrhea, treatment for serious respiratory symptoms, prenatal care, birth assistance by a trained health provider, exclusive breastfeeding during the first 6 months of life, and family planning) is at least 1.5-times greater in the HAS service area than in Haiti at large and ranges as high as 2.8-times greater.10 Thus, the inputs, processes, and outputs of the health services at HAS during the late 1990s, when compared with those for Haiti nationally, support the conclusion that the differences in under-5 mortality can be attributed to the integrated system of primary health care, hospital referral care, and community development programs operated by HAS. Although data regarding inputs, processes, and outputs for earlier periods are not available, it is common knowledge in Haiti that the services present at HAS in the late 1990s were generally reflective of the volume and quality present there for several decades.
Is the entire population of Haiti an appropriate comparison group for the HAS service area? We compared data regarding the socioeconomic characteristics of the HAS population and those of rural Haiti for the year 2000 and found that the levels of education, access to electricity, and household sanitation were essentially the same for the 2 populations, although the access to protected water was substantially less in the HAS service area.10 Furthermore, we found that the levels of childhood malnutrition in the HAS service area as measured by height-for-age, weight-for-age, and height-for-weight were no better than in the rest of rural Haiti.10
Haiti is a relatively small country of 8.1 million people in an area about the size of Mary-land. Haiti is still largely rural, as is the population served by HAS. Furthermore, it has no major ethnic, religious, cultural, or language divisions and is relatively homogeneous in economic terms except for a very small middle class and an even smaller class of elite. In 1970, 78% of the national population was rural and in 2001, 64% was rural.2 As Table 1 ▶ and Figure 2 ▶ demonstrate, under-5 mortality rates were not available for rural Haiti before 1985, and the rural rates that are available recently are similar to the national rates. For the above reasons, we conclude that the national population of Haiti is a suitable comparison group to the HAS service area except in terms of the availability of health and other community-development programs.
The rapid decline in under-5 mortality during the first decade of program operations at HAS can be explained largely by the decline in mortality from neonatal tetanus (almost all pregnant women were immunized against tetanus) as well as by the increased coverage of other key child survival interventions. In the late 1960s, a retrospective study found that neonatal tetanus had been responsible for 270 deaths per 1000 live births.20 When HAS began providing services in 1956, program emphasis was on immunizing pregnant women against tetanus, hospital care of newborns with tetanus (a recovery rate of 50%), and proper umbilical cord care at the time of delivery. Only when the community health program began in 1967, which made it possible to immunize all women of reproductive age, did infant mortality attributable to tetanus fall to virtually zero.20
Even after the dramatic initial declines at HAS in under-5 mortality from 1960 to1970, the 1–4 year mortality rate declined by 56% between 1970 and 1999 (35.4 to 15.7) and the overall under-5 mortality rate declined by 23% (from 80.7 to 62.3) during the same period. However, the infant mortality rate has shown no consistent trend and remained between 33.0 and 47.3.
Why has there been a lack of progress at HAS in further reducing under-5 mortality since the early 1970s? The program service area gradually expanded from 8820 to 180 000 people and the areas of expansion were mostly in isolated mountainous areas. There, the mortality rates are twice that of the central valley area around the hospital, where the community health program began (H. P., MD, unpublished data, 2006).
In 2000, rates of childhood malnutrition at HAS remained very high: 18.4% of children were at less than 2 standard deviations below the international mean of weight-for-age and 22.6% of the children were at less than 2 standard deviations below the international mean of height-for-age.10 Improving household food security was difficult in the midst of Haiti’s economic and political turmoil during the 1980s and 1990s. Thus, the persistence of childhood malnutrition limited progress in further reducing under-5 mortality.
The arrival of HIV/AIDS in the population in the early 1980s is another possible explanation. We have estimated elsewhere10 that if HIV/AIDS had not been present, the under-5 mortality rate in the HAS service area would have fallen by an additional 20% and the under-5 mortality rate for Haiti as a whole would have fallen by an additional 8%. HIV/AIDS affected 3.7% of the HAS service population of reproductive age in 1996 and 3.9% in 2001 (H.P., MD, unpublished data, 2006) compared with 5.6% nationally in 2003.21
Haiti has one of the most mobile populations in the world. Furthermore, children are frequently moved from one household to another and away from 1 or both of their biological parents because of the death of a parent, instability of conjugal unions, changing locations for agricultural work, or opportunities for income generation in other areas.22 Field experience in Haiti suggests that children born into unstable unions have higher mortality than children born into stable households.22,23 As a result, the challenges for continuity of care in child health programs and reducing child mortality further are enormous.
Between 1986 and 1999, the country remained in almost continuous political turmoil and steady economic decline. There were frequent changes of government and the per capita income declined by 3.0% during this period.2
Given the higher levels of mortality in the expansion areas, the impoverishment of the population, the low level of education, the high rates of childhood malnutrition, HIV/AIDS, the mobility of the population, and the overall political instability that were all present throughout this period, it is remarkable that the under-5 mortality rates at HAS did not increase as the service area gradually expanded.
Limitations
The main weaknesses of this study are that the mortality data are largely retrospective and that a gap existed in data collection between 1972 and 1992 at HAS. However, national data were based on a similar retrospective methodology with a gap in data collection between 1970 and 1995. The net effect of the possible biases should be negligible when comparing the differences in under-5 mortality between the HAS service area and Haiti at large. The inclusion of prospectively collected vital events data in the late 1960s at HAS along with subsequent retrospectively collected vital events data is not likely to significantly affect the quality of the data, because recent research has demonstrated a high degree of correlation when the 2 methods are applied to the same population.24
Similar Assessments Elsewhere
We are aware of only 1 other program that has documented long-term program effects on under-5 mortality: the Matlab Maternal and Child Health-Family Planning Program in Bangladesh. In Matlab, under-5 mortality in an intervention area of 100000 people has been monitored and compared with under-5 mortality in an adjacent control area since 1965.25,26 There, under-5 mortality rates have generally been one-third lower in the intervention area than in the comparison area, and this difference has persisted since 1978.27 Although the Matlab program has a far more rigorous and intensive surveillance system and lacks a community development component, it is similar to HAS’s program in that it provides services in the home and refers patients needing hospitalization.
Other programs that have been able to document impact on under-5 mortality have reported findings for much shorter periods of time (usually 5 years or less), and these programs have usually introduced 1 or several selected interventions.28–36 One notable exception is the Society for Education, Action and Research in Community Health field trial in Gadchiroli, India. In this trial, interventions by community health workers were focused on case management of childhood pneumonia and home-based neonatal care, which has resulted in a decline in neonatal mortality over a 10-year period.37 In other locations in developing countries, systems of monitoring vital events over a longer period of time have been established, but do not lend themselves to comparisons with populations that are similar in other respects except for program interventions.38,39 One health program, the Jamkhed Comprehensive Rural Health Project in India, has established a long-term infant mortality surveillance capability and reports an infant mortality rate of 20 deaths per 1000 live births, but without an appropriate comparison group.40 Thus, we believe that HAS provides one of the few available demonstrations of the long-term impact of a local health program on under-5 mortality.
Conclusions
Our findings support the conclusion that a local system of comprehensive health and development activities can make a major long-term impact on under-5 mortality. Narrower, disease-specific approaches have been successful and can take justifiable credit for their role in reducing the number of child deaths globally.41 However, overreliance on such approaches may be one of the factors that has stalled progress in further reducing under-5 mortality. Although successful in the short term, these narrower, disease-specific approaches are not the long-term answer. The need, therefore, is to begin to strengthen integrated long-term local health and community development programs in order to achieve sustainable gains in public health.42–45
Our findings provide supportive evidence that HAS, as an integrated system of health and development activities, has reduced under-5 mortality and sustained that reduction over 3 decades. Similar results in other severely impoverished settings should be achievable if adequate financial and technical support and professional leadership are available. Additional evidence regarding long-term effectiveness is needed from other program sites around the world. The United Nations Millennium Goal is to reduce under-5 mortality by two thirds by the year 2015. If that goal is to be reached, financial and technical support as well as professional leadership will be required to build on successful experiences such as that at Hôpital Albert Schweitzer by replicating and scaling up these programs.
Acknowledgments
The evaluation activities which made this report possible were funded by the Bill and Melinda Gates Foundation, the United States Agency for International Development, and the general operating funds of HAS.
The authors acknowledge the late John B. Wyon for his guidance and critical influence on the design of the HAS outreach services almost 4 decades ago; the late Larimer Mellon and Gwendolyn Mellon for their vision, personal involvement, and financial support from 1956 to 2000; the residents of the HAS service area for their cooperation; the board of directors of the Grant Foundation in Pittsburgh, Pa, for commissioning this evaluation; the previous and current staff and professional leadership of HAS who made these results possible; and Jack Bryant, Doug Ewbank, Leslie King, Robert Northrup, Jon Rhode, Dory Storms, and John Wyon, as well as anonymous reviewers, for their helpful comments on the article. We are grateful to Doug Ewbank of the University of Pennsylvania, who provided technical support for the mortality analysis, and to Bernard Barrère of ORC Macro, who provided information on the numbers of births and deaths in rural areas from the Haiti national health and demographic survey in 2000. We are also grateful for the assistance that Bryan Proffitt and Angela Barton provided in computerizing the birth history data.
Finally, the authors acknowledge the strong long-term support of the many individual and organizational donors who have made the work at HAS possible.
Human Participant Protection At the time data were collected, HAS did not have an institutional review board. The methods of data collection from households in the HAS service area in 2000 were all within the guidelines of HAS’s policies and procedures.
Peer Reviewed
Contributors H. Perry developed the idea for this article, directed the collection and analysis of the data, wrote the initial drafts, and coordinated the contributions of the coauthors. W. Berggren and G. Berggren designed and led the initial implementation of HAS’s community health program from 1967 to 1974 and are currently technical advisors to HAS. D. Dowell worked as a pediatrician for HAS off and on from 1970 to 2003, and served as Medical Director of the HAS community health program from 1999 to 2003. H. Menager, E. Bottex, and J. R. Dortonne led community health activities at HAS during the time covered by the study. F. Philippe provided field supervision of the collection of mortality data at HAS from 1985 to 1999. M. Cayemittes directed the activities of the Institut Haitien de l’Enfance in collecting national mortality data for Haiti from 1980 to 1999, as well as for collecting the data regarding socioeconomic conditions, childhood nutritional data, and coverage of child survival services in the HAS service area for the year 2000.
References
- 1.Ahmad OB, Lopez AD, Inoue M. The decline of child mortality: a reappraisal. Bull World Health Organ. 2000;78:1175–1191. [PMC free article] [PubMed] [Google Scholar]
- 2.United Nations Development Program. Human Development Report 2003. Available at: http://www.undp.org/hdr2003. Accessed September 19, 2003.
- 3.Ewbank DC, Gribble JN, eds. Effects of Health Programs on Child Mortality in Sub-Saharan Africa. Washington, DC: National Academy Press; 1993. [PubMed]
- 4.Ewbank DC. Evaluating large scale health interventions: methodological issues. In: Rashad H, Gray R, Boerma T, eds. Evaluation of the Impact of Health Interventions. Liège, Belgium: International Union for the Scientific Study of Population; 1995:277–295.
- 5.Hill Z, Kirkwood B, Edmond K. Family and Community Practices that Promote Child Survival, Growth and Development: A Review of the Evidence. Geneva, Switzerland: World Health Organization; 2004.
- 6.McKeown T. The Role of Medicine: Dream, Mirage or Nemesis? London, England: Nuffield Provincial Hospitals Trust; 1976.
- 7.Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries. Pop and Dev Review. 1984;10(suppl):25–45. [PMC free article] [PubMed] [Google Scholar]
- 8.Leon DA, Walt G. Poverty, inequality and health in international perspective: a divided world? In: Leon D, Walt G, eds. Poverty, Inequality and Health: An International Perspective. Oxford, England: Oxford University Press; 2001:1–16.
- 9.Evans T, Whitehead M, Diderichsen F, Bhuiya A, Wirth M, eds. Challenging Inequities in Health: From Ethics to Action. Oxford, England: Oxford University Press; 2001.
- 10.Perry H, Cayemittes M, Philippe F, et al. Reducing under-5 mortality through Hôpital Albert Schweitzer’s integrated system in Haiti. Health Policy Plan. 2006;21: 217–230. [DOI] [PubMed] [Google Scholar]
- 11.Hôpital Albert Schweitzer Haiti. Available at: http://www.hashaiti.org. Accessed September 27, 2005.
- 12.Cayemittes M, Placide MF, Barrère B, Mariko S, Sévère B. Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-III) Haiti, 2000. Calverton, MD: ORC Macro; Port-au-Prince, Haiti: Ministère de la Santé Publique et de la Population and Institut Haïtien de l’Enfance; 2001.
- 13.Berggren WL, Ewbank DC, Berggren GG. Reduction of mortality in rural Haiti through a primary-health-care program. New Engl J Med. 1981;304:1324–1330. [DOI] [PubMed] [Google Scholar]
- 14.Berggren G, Menager H, Genece E, Clerisme C. A prospective study of community health and nutrition in rural Haiti from 1968 to 1993. In: Scrimshaw NS, ed. Community-Based Longitudinal Nutrition and Health Services: Classical Examples from Guatemala, Haiti and Mexico. Boston, MA: International Foundation for Developing Countries; 1995:143–178.
- 15.Berggren G, Berggren W, Menager H, Genece E. Longitudinal community health research for equity and accountability in primary health care in Haiti. In: Das Gupta M, Aaby P, Garenne M, Pison G, eds. Prospective Community Studies in Developing Countries. Oxford, England, and New York, NY: Clarendon Press/Oxford University Press; 1997:157–185.
- 16.Institut Haitien de Statistiques. Statistical Report on Haiti. Port-au-Prince, Haiti: Institut Haitien de Statistiques; 1970.
- 17.Allman J, May J. Fertility, mortality, migration and family planning in Haiti. Pop Stud. 1979;33:505–521. [Google Scholar]
- 18.Cayemittes M, Rival A, Barrère B, Lerebours G, Gédéon MA. Enquête Mortalité, Morbidité et Utilisation des Services (EMMUS-II) Haiti, 1994–95. Calverton, MD: Macro International, Inc.; Petionville, Haiti: Institut Haïtien de l’Enfance; 1995.
- 19.Abrahamson JH, Gahlinger PM. Computer Programs for Epidemiologists (PEPI) v. 4.0. Salt Lake City, UT: Sagebrush Press; 2001.
- 20.Berggren WL. Administration and evaluation of rural health services. I. A tetanus control program in Haiti. Am J Trop Med Hygiene. 1974;23:936–949. [DOI] [PubMed] [Google Scholar]
- 21.UNAIDS: The Joint United Nations Programme on HIV/AIDS. Available at: http://www.unaids.org/en. Accessed on September 26, 2005.
- 22.Berggren G, Berggren W. Household structure, mobility, family building, and dissolution in rural Haiti: insights from longitudinal studies in rural Haitian communities [Seminar]. Portudal, Senegal: The International Union for the Scientific Study of Population (IUSSP); 1991.
- 23.Rawson I, Berggren G. Family structure, child location and nutritional disease in rural Haiti. Environ Child Health. 1973;19:288–298. [DOI] [PubMed] [Google Scholar]
- 24.Espeut D. A Validation of Birth and Pregnancy Histories in Matlab, Bangladesh [PhD thesis]. Baltimore, MD: Johns Hopkins University; 2002.
- 25.Aziz KMA, Mosley WH. The history, methodology, and main findings of the Matlab Project in Bangladesh. In: Das Gupta M, Aaby P, Garenne M, Pison G, eds. Prospective Community Studies in Developing Countries. Oxford, England, and New York, NY: Clarendon Press/Oxford University Press; 1997: 28–53.
- 26.Koenig M, Strong M. Assessing the mortality impact of an integrated health programme: lessons from Matlab, Bangladesh. In: Rashad H, Gray R, Boerma T, eds. Evaluation of the Impact of Health Interventions. Liège, Belgium: International Union for the Scientific Study of Population; 1995:361–395.
- 27.Health and Demographic Surveillance System, Matlab: Registration of Health and Demographic Events, 2000. Scientific Report No. 89. Dhaka, Bangladesh: International Centre for Diarrhoeal Disease Research, Centre for Health and Population Research; 2002.
- 28.Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmuck MD. Effect of home-based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet. 1999;354:1955–1981. [DOI] [PubMed] [Google Scholar]
- 29.Becker SR, Diop F, Thornton JN. Infant and child mortality in two counties of Liberia: results of a survey in 1988 and trends since 1984. Int J Epidemiol. 1993; 22(Suppl 1):S56–S63. [DOI] [PubMed] [Google Scholar]
- 30.Ewbank DC. Impact of health programs on child mortality in Africa: evidence from Zaire and Liberia. Int J Epidemiol. 1993;22(Suppl 5):S64–S72. [DOI] [PubMed] [Google Scholar]
- 31.Greenwood BM, Bradley AK, Byass P, et al. Evaluation of a primary health care programme in Gambia. II. Its impact on mortality and morbidity in young children. J Trop Med Hygiene. 1990;93:87–97. [PubMed] [Google Scholar]
- 32.Gwatkin D, Wray JD, Wilcox JR. Can Health and Nutrition Interventions Make a Difference? Monograph No. 13. Washington, DC: Overseas Development Council; 1980.
- 33.Lamb WH, Foord FA, Lamb CMB, Whitehead RG. Changes in maternal and child mortality rates in three isolated Gambian villages over ten years. Lancet. 1984; 2:912–914. [DOI] [PubMed] [Google Scholar]
- 34.Perry HB, Shanklin DS, Schroeder DG. Impact of a community-based comprehensive primary healthcare programme on infant and child mortality in Bolivia. J Health Pop Nutr. 2003;21:383–395. [PubMed] [Google Scholar]
- 35.Pison G, Trape JF, Lefebvre M, Enel C. Rapid decline in child mortality in a rural area of Senegal. Int J Epidemiol. 1993;22:72–80. [DOI] [PubMed] [Google Scholar]
- 36.Bryant J, Marsh D, Khan KS, et al. A developing country university oriented toward strengthening health systems: challenges and results. Am J Public Health. 1993;83:1537–1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bang AT, Bang RA, Reddy HM. Home-based neonatal care: summary and applications of the field trial in rural Gadchiroli, India (1993 to 2003). J Perinatology. 2005;25:S108–S122. [DOI] [PubMed] [Google Scholar]
- 38.Garenne M, Cantrell P. Three decades of research on population and health: the ORSTOM experience in rural Senegal. In: Das Gupta M, Aaby P, Garenne M, Pison G, eds. Prospective Community Studies in Developing Countries. Oxford, England, and New York, NY: Clarendon Press/Oxford University Press; 1997: 233–252.
- 39.Van Ginneken JK, Muller AS, Omondi O. Design, results, and comments on the Machakos Project in Kenya. In: Das Gupta M, Aaby P, Garenne M, Pison G, eds. Prospective Community Studies in Developing Countries. Oxford, England, and New York, NY: Clarendon Press/Oxford University Press; 1997:189–212.
- 40.Arole M, Arole R. Jamkhed: A Comprehensive Rural Health Project. London, England: MacMillan Press; 1994.
- 41.Walsh J, Warren KS. Selective primary health care: an interim strategy for disease control in developing countries. New Engl J Med. 1979;301:967–974. [DOI] [PubMed] [Google Scholar]
- 42.Perry HB, Robison N, Chavez D, et al. Attaining health for all through community partnerships: principles of the census-based, impact-oriented approach developed in Bolivia, South America. Soc Sci Med. 1999; 48:1053–1067. [DOI] [PubMed] [Google Scholar]
- 43.Bellagio Study Group on Child Survival. Knowledge into action for child survival. Lancet. 2003;362: 323–327. [DOI] [PubMed] [Google Scholar]
- 44.Sachs JD. Macroeconomics and Health: Investing in Health for Human Development. Geneva, Switzerland: World Health Organization; 2001.
- 45.World Health Organization. The World Health Report 2000. Health Systems: Improving Performance. Geneva, Switzerland: World Health Organization; 2000.


