Abstract
OBJECTIVE
To determine the prevalence and clinical characteristics of metabolic syndrome in a family practice population.
DESIGN
Chart abstraction and patient interviews.
SETTING
Family Medicine Centre in Kingston, Ont.
PARTICIPANTS
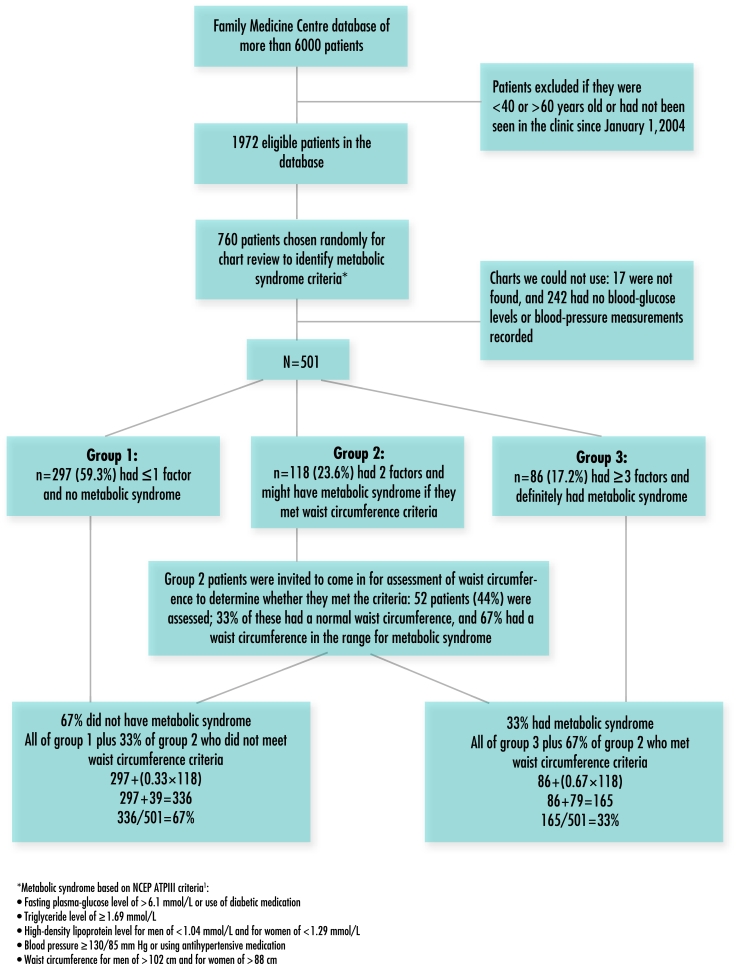
Five hundred one men and women between 40 and 60 years old registered at the Family Medicine Centre. Based on the number of risk factors for metabolic syndrome recorded on their charts (except for waist circumference), participants were stratified into 3 groups. Group 1 were patients without the syndrome (0 or 1 risk factor). Group 2 were patients who might have the syndrome, depending on subsequent measurement of waist circumference (2 risk factors). Group 3 were patients with metabolic syndrome (3 or more risk factors). Patients in group 2 were invited to attend the clinic for an assessment of waist circumference.
MAIN OUTCOME MEASURES
Presence of metabolic syndrome, as defined by the Third Adult Treatment Panel of the National Institutes of Health, based on waist circumference; blood pressure; and serum triglyceride, high-density lipoprotein, and glucose levels.
RESULTS
Prevalence of metabolic syndrome in this population was 33% (35% among men and 32% among women). Hypertension was the most prevalent component of the syndrome (81.6%). The most common combination of 3 components of the syndrome was central obesity, hypertriglyceridemia, and hypertension (43.7%).
CONCLUSION
Metabolic syndrome was prevalent among patients in the family practice studied. One in every 3 patients between 40 and 60 years old met the criteria for the syndrome.
Abstract
OBJECTIF
Déterminer la prévalence et les caractéristiques cliniques du syndrome métabolique dans la clientèle d’un centre de médecine familiale.
TYPE D’ÉTUDE
Étude sur dossier et interview de patients.
CONTEXTE
Le Centre de médecine familiale de Kingston, Ontario.
PARTICIPANTS
Cinq cent un hommes et femmes de 40 à 60 ans inscrits au Centre de médecine familiale. Les participants ont été répartis en 3 groupes selon le nombre de facteurs de risque retrouvés dans leur dossier (à l’exception du tour de taille). Les patients du groupe 1 n’avaient pas le syndrome (0 ou 1 facteur de risque). Ceux du groupe 2 (2 facteurs de risque) pouvaient l’avoir: cela dépendait de la mesure subséquente du tour de taille. Les patients du groupe 3 avaient le syndrome (3 facteurs de risque ou plus). Les patients du groupe 2 ont été invités à venir faire mesurer leur tour de taille à la clinique.
PRINCIPAUX PARAMÈTRES ÉTUDIÉS
Présence du syndrome métabolique, d’après les critères du Third Adult Treatment Panel du National Institute of Health: circonférence de taille, tension artérielle et niveaux sériques de triglycérides, de lipoprotéines de haute densité et de glucose.
RÉSULTATS
Dans cette population, la prévalence du syndrome métabolique était de 33% (35% chez les hommes et 32% chez les femmes). La composante la plus fréquente du syndrome était l’hypertension (81,6%). Obésité, hypertriglycéridémie et hypertension étaient la triade la plus fréquente (43,7%).
CONCLUSION
Le syndrome métabolique était prévalent chez les patients de la clinique de médecine familiale étudiée. Dans le groupe des 40 à 60 ans, 1 patient sur 3 rencontrait les critères du syndrome.
EDITOR’S KEY POINTS.
Metabolic syndrome is a constellation of clinical findings (central obesity, dyslipidemia, hypertension, and elevated blood sugar) that substantially increases risk of coronary artery disease.
This study, the first in Canada, measured the prevalence of metabolic syndrome in the population of a family practice unit in a small Canadian city.
The syndrome was found in 33% of the population measured; 1 in 3 patients was substantially at risk of coronary artery disease.
The study was limited because it focused on a single, moderately affluent population from an academic practice. It does, however, provide results of considerable concern. Similar studies should be carried out elsewhere in Canada.
POINTS DE REPÈRE DU RÉDACTEUR.
Le syndrome métabolique est un ensemble de données cliniques (obésité abdominale, dyslipidémie, hypertension et élévation de la glycémie) qui augmente de façon appréciable le risque de maladie coronarienne.
Cette étude, la première au Canada, évaluait la prévalence du syndrome métabolique parmi la clientèle d’une clinique de médecine familiale d’une petite ville canadienne.
Le syndrome était présent chez 33% de la population étudiée; 1 patient sur 3 présentait un risque important de maladie coronarienne.
Cette étude présentait certaines limitations, puisqu’elle portait sur la clientèle plutôt aisée d’une clinique universitaire. Ses résultats sont toutefois préoccupants. Il serait opportun de faire des études semblables ailleurs au Canada.
Metabolic syndrome is identified by a constellation of central obesity, dyslipidemia (hypertriglyceridemia and low levels of high-density lipoprotein [HDL] cholesterol), elevated blood pressure, and insulin resistance that leads to increased risk of cardiovascular disease and type 2 diabetes.1 There are several definitions of metabolic syndrome, as described by Miranda et al.2 For the purpose of this study, the criteria formulated by the National Institutes of Health’s National Cholesterol Education Program’s Third Adult Treatment Panel (NCEP ATPIII) will be used.1
Metabolic syndrome is based on the hypothesis that a condition characterized by multiple risk factors will carry a greater risk of adverse clinical outcomes than a condition with a single risk factor will. Recently published results from the Atherosclerosis Risk in Communities Study reported an increasing risk of coronary artery disease (CAD) with an increasing number of metabolic syndrome components in men and women.3 Men and women with metabolic syndrome (defined by their having 3 or more components of the syndrome) were almost twice as likely to develop CAD as those without the syndrome. These findings are in agreement with another published study.4
Information about the prevalence of metabolic syndrome in Canada is limited. Data from the Canada Heart Health Survey, a nationally representative cross-sectional survey conducted between 1986 and 1992, indicate a prevalence of 17.0% in men and 13.2% in women.5 The prevalence of obesity increased in Canada from 5.6% to 14.8% between 1985 and 1998,6 however, and is expected to have increased even more during the last couple of years, so the prevalence of metabolic syndrome might have risen also.
To complement existing information about the prevalence of metabolic syndrome, this study was designed to determine the prevalence and clinical aspects of it in a family practice population.
METHODS
Definition of metabolic syndrome
In this study, NCEP ATPIII criteria were used to define metabolic syndrome.1 If 3 or more of the following criteria were found, metabolic syndrome was determined to exist: fasting plasma glucose level of >6.1 mmol/L, triglyceride level of ≥1.69 mmol/L, HDL cholesterol level for men of <1.04 mmol/L and for women of <1.29 mmol/L, blood pressure of ≥130/85 mm Hg, and waist circumference for men of >102 cm and for women of >88 cm. Subjects using antihypertensive or diabetic medications were considered to have an associated abnormal risk factor.
Patient population
The Family Medicine Centre (FMC) at Queen’s University has a patient population of approximately 6000. The FMC is an academic teaching practice in Kingston, Ont, a small city of approximately 130 000 population. Practice patients have a range of demographic characteristics, but are mostly affluent. Patients 40 to 60 years old, who had been seen at least once in the FMC since January 1, 2004, were identified in the registration database (n = 1972). A random sample of 760 patients (nearly 40%) were selected; 259 of these were excluded due to either missing charts or incomplete data. Data on the remaining 501 (about 25% of the eligible population of 1972 patients) were used in the analysis. We determined that this 25% sample provided 99% confidence of obtaining a correct estimate of the prevalence of metabolic syndrome in this population with a 5% margin of error.
Data collection
Charts of the 501 patients were reviewed, and 4 of the 5 criteria for metabolic syndrome were abstracted (most recent triglyceride level, HDL level, blood pressure and use of antihypertensive medication, and fasting blood glucose level and use of diabetic medication within the past 5 years). Only a few patients had the fifth criteria, waist circumference, recorded on the chart (6.2%). Demographic characteristics and most recent weight and height were also abstracted from the chart. Patients were categorized into 3 groups based on the number of criteria they met (0-1, 2, or ≥3); 297 patients (59.3%) were stratified into group 1 (patients without metabolic syndrome), 118 (23.6%) into group 2 (might have metabolic syndrome), and 86 (17.2%) into group 3 (patients with metabolic syndrome) (Figure 11). Whether or not patients in group 2 had metabolic syndrome depended on the fifth criteria, waist circumference.
Figure 1.
Study design
The 118 patients from group 2 were invited by letters from their physicians to attend the clinic to have their height, weight, and waist circumference measured. Height was measured without shoes to the nearest 0.5 cm; weight was measured without shoes in light clothing to the nearest 0.5 kg; and waist circumference was measured between the iliac crest and the lowest rib to the nearest 0.5 cm while subjects were at minimal respiration.
Of the 118 patients in group 2, 52 (44.1%) agreed to come in to be measured and weighed. The study protocol was approved by the Research Ethics Board of Queen’s University. Written consent was obtained from group 2 participants when they came for assessment.
Statistical analysis
Differences in characteristics between participants with and without metabolic syndrome were tested with independent sample t tests for normal distributed variables, with the Wilcoxon rank sum test for skewed variables, and with the chi-square test for categorical variables.
Prevalence of metabolic syndrome in the original population was calculated by using a formula that took into account all patients in group 3 who were already diagnosed with metabolic syndrome and the proportion of patients in group 2 who met waist circumference criteria (Figure 11). Best estimate of waist circumference of patients in group 2 who did not come in to be measured was determined in 3 ways: waist circumference recorded on the chart, body mass index (BMI) recorded on the chart (if ≥30 we assumed waist circumference met the criteria because a BMI of 30 correlates well with the metabolic syndrome waist circumference cutoff of 102 cm for men and 88 cm for women), and a random imputation process (if no weight, BMI, or waist circumference was recorded).
All tests of statistical significance were two-sided. The significance level was set at 5%. All statistical analyses were carried out using SPSS 11.0 software.
RESULTS
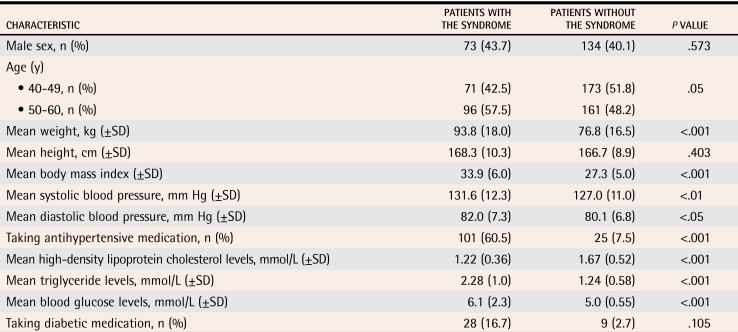
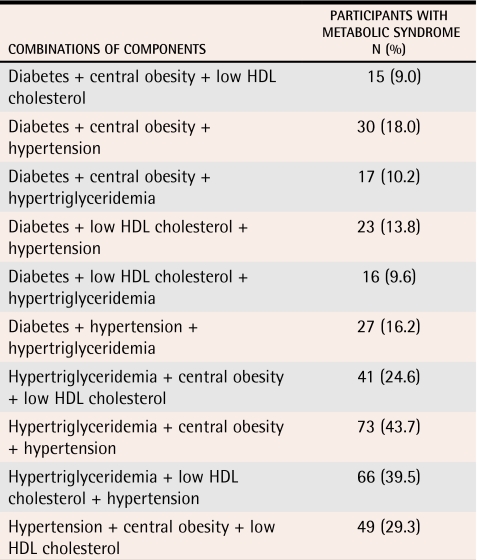
Of the 501 patients, 167 met the criteria for metabolic syndrome, so our best estimate of its prevalence in this population was 33% (35% among men and 32% among women). Patients aged 50 to 60 were more likely to have metabolic syndrome than those aged 40 to 49 (Table 1). They were also more likely to weigh more, have higher blood pressure, and have worse lipid profiles, all of which are not surprising because these are the features that define metabolic syndrome. The most common combination of 3 components of the syndrome was central obesity, hypertriglyceridemia, and hypertension (43.7%, Table 2).
Table 1.
Characteristics of participants with and without metabolic syndrome
SD—standard deviation.
Table 2.
Prevalence of combinations of 3 components of metabolic syndrome
HDL—high-density lipoprotein.
DISCUSSION
We estimated that 33% of the patients 40 to 60 years old registered at the FMC had metabolic syndrome. The prevalence of metabolic syndrome varies among studies, mostly because of different definitions of the syndrome. The prevalence we found was higher than that reported by Ardern et al (17% among men and 13.2% among women).5 Ardern et al defined metabolic syndrome without taking into account use of antihypertensive drugs and actual blood-glucose levels. They used self-report of physician-diagnosed diabetes instead. In addition, they used a broad age category (20 to 74 years), and their data are old. Our findings were in agreement with those of Ford et al, who reported a prevalence of 33.0% among American men and 30.6% among American women 40 to 59 years old.7
Recently, the International Diabetes Federation published a new definition of metabolic syndrome in an attempt to establish one worldwide definition.8 The main differences from the NCEP ATPIII definition are that a large waist circumference has become a prerequisite for the syndrome, the cutoff points for waist circumference have been lowered (94 cm for men and 80 cm for women), the cutoff point for glucose level has been lowered, and patients using lipid-lowering medication are considered to have the associated abnormal factor. With this new definition, our prevalence would probably increase, although we were unable to verify this because of missing information about use of lipid-lowering medications.
Most literature on prevalence relies on population-based studies. To determine whether the prevalence of metabolic syndrome in a family practice population in Canada had been studied previously, we conducted a MEDLINE search using the terms “Metabolic syndrome” AND “Canada” AND (“primary care” OR “general practice” OR “family practice”). We found no articles. We then deleted the last part of the search phrase and searched using “Metabolic syndrome” AND “Canada”; this produced 139 hits.
We reviewed the titles and found studies that were relevant but that had not set out specifically to measure the prevalence of metabolic syndrome in a family practice population. Pollex et al9 reported on the prevalence of metabolic syndrome among Ontario Oji-Cree and found that 43.4% of adults older than 35 had the syndrome. Monsalve et al10 conducted a study of all adults in primary care in Bella Coola, BC, and assessed cardiovascular disease and cardiovascular risks. They determined that 70% of aboriginals and 53% of nonaboriginals had metabolic syndrome based on their having at least 3 of the 5 risk factors for it. We used the same definition of the syndrome and found a prevalence of 33%. We think it likely that family physicians, wherever they practise in Canada, have a substantial proportion of patients with metabolic syndrome.
Limitations
Our reported prevalence of metabolic syndrome might overestimate the real prevalence because we excluded patients who did not have blood pressure measurements or blood-glucose levels recorded on their charts (242 patients), and they might have been the healthier people. As well, we had to impute a small amount of data, which might have had an effect. On the other hand, our estimate might be low because our patient population likely had a higher socioeconomic status than the population in general. Despite these limitations, our estimate is probably acceptable for a family practice population in a southern Ontario community.
Conclusion
Our study suggests that metabolic syndrome has a high prevalence in family practice populations. Some argue that combining risk factors and calling the combination a syndrome is of limited use. Regardless of this criticism, it appears that every third patient aged 40 to 60 who walks into a family doctor’s office is at risk of cardiovascular disease because of these factors, whether they are combined into a syndrome or simply looked at separately. Our goal was to measure the degree to which metabolic syndrome or its individual components were evident in a family practice and to raise awareness of the syndrome.
Biography
Ms van den Hooven and Ms Ploemacher are Masters students from the Netherlands doing research internships at the Centre for Studies in Primary Care at Queen’s University in Kingston, Ont. Dr Godwin was Director of the Centre for Studies in Primary Care when the study was conducted and is now Director of the Primary Healthcare Research Unit at Memorial University of Newfoundland in St John’s.
Footnotes
Competing interests: None declared
References
- 1.National Institutes of Health. Third report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in adults (Adult Treatment Panel III). NIH Publication 02-5215. Washington, DC: National Institutes of Health; 2002. [Google Scholar]
- 2.Miranda PJ, Defronzo RA, Califf RM, Guyton JR. Metabolic syndrome: definition, pathophysiology, and mechanisms. Am Heart J. 2005;149:33–45. doi: 10.1016/j.ahj.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 3.McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the Atherosclerosis Risk in Communities Study. Diabetes Care. 2005;28:385–390. doi: 10.2337/diacare.28.2.385. [DOI] [PubMed] [Google Scholar]
- 4.Malik S, Wong ND, Franklin S, Pio J, Fairchild C, Chen R. Cardiovascular disease in U. S. patients with metabolic syndrome, diabetes, and elevated C-reactive protein. Diabetes Care. 2005;28:690–693. doi: 10.2337/diacare.28.3.690. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CI, Katzmarzyk PT, Janssen I, Ross R. Discrimination of health risk by combined body mass index and waist circumference. Obes Res. 2003;11:135–142. doi: 10.1038/oby.2003.22. [DOI] [PubMed] [Google Scholar]
- 6.Katzmarzyk PT. The Canadian obesity epidemic, 1985–1998. CMAJ. 2002;166:1039–1040. [PMC free article] [PubMed] [Google Scholar]
- 7.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U. S. adults. Diabetes Care. 2004;27:2444–2449. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 8.International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome. Brussels, Belg: International Diabetes Federation; 2003. [cited 2005 July 25]. Available at: http://www.idf.org/webdata/docs/IDF_Metasyndrome_definition.pdf. [Google Scholar]
- 9.Pollex RL, Hanley AJ, Zinman B, Harris SB, Khan HM, Hegele RA. Metabolic syndrome in aboriginal Canadians: prevalence and genetic associations. Atherosclerosis. 2006;184(1):121–129. doi: 10.1016/j.atherosclerosis.2005.03.024. [DOI] [PubMed] [Google Scholar]
- 10.Monsalve MV, Thommasen HV, Pachev G, Frohlich J. Differences in cardiovascular risks in the aboriginal and non-aboriginal people living in Bella Coola, British Columbia. Med Sci Monit. 2005. CR21-8. [PubMed]