SYNOPSIS
Objective
The purpose of this ecological study was to relate West Nile virus (WNV) human case fatality rates to county-level demographic and surveillance variables, thereby characterizing the populations to which WNV poses the greatest threat.
Methods
The authors acquired data on human, avian, and mosquito WNV infections for the 13 states in which there were 100 or more human cases during 2003. The data on avian and mosquito infections were converted into surveillance variables using empirical Bayes methodology. A preliminary logistic regression model was formulated to relate these surveillance variables and demographic variables to case fatality rates. The statistical technique of backward elimination was applied to obtain a final model in terms of the variables most useful for predicting case outcomes.
Results
The probability of a fatal outcome depends on the poverty rate for the county in which the infected person lives (p=0.0283), the average temperature (p<0.0001), and surveillance variables reflecting the fractions of Culex pipiens and Culex restuans mosquitoes among infected mosquitoes (p=0.0079; p=0.0076).
Conclusions
Effective WNV educational programs and control measures are vital, especially in poverty-stricken areas. A uniform protocol for disseminating county-level data could facilitate timely responses to WNV outbreaks and to emerging infectious diseases more generally.
The emerging infectious disease caused by West Nile virus (WNV) has been a source of concern for public health practitioners since the 1999 outbreak in New York City1,2 and subsequent spread of the virus across the continental United States and parts of Canada.3–5 WNV, a member of the genus Flavivirus first detected in 1937,6 infects both vertebrates and invertebrates, initiating sufficient viremia in a vertebrate host to permit acquisition of the virus by a vector and transmission to another host.7,8 The predominant route of transmission to humans is through mosquitoes that acquire the virus from infected birds; infections in humans are incidental, taking place when the transmission cycle between mosquitoes and birds amplifies.9
Common virus reservoirs include members of the corvid family, especially crows and blue jays, for which infection is often fatal.10 However, infection has been documented in more than 200 species of birds.11 Common WNV vectors include Culex pipiens, Culex restuans, and Culex tarsalis mosquitoes, although mosquitoes from other genera (notably Aedes and Ochlerotatus) are known to transmit WNV.12–14 Culex pipiens mosquitoes were implicated as the primary vectors in a 1996 outbreak of WNV in Bucharest, Romania; some researchers have speculated that urban areas provide favorable environments for mosquito proliferation and virus amplification.15,16 Culex tarsalis mosquitoes have been identified as particularly efficient vectors in the western United States.17
While numerous studies have addressed risk factors and mechanisms for acquiring WNV,9,18–20 comparatively little progress has been made toward understanding which populations are most vulnerable to poor and fatal outcomes. Such an understanding would complement existing knowledge about the social and economic burdens imposed by WNV;21 more importantly, it could guide strategies for allocating resources and organizing prevention efforts.
The goal of this ecological study is to relate WNV case fatality rates from the peak year of 2003 to county-level surveillance and demographic variables for the states in which WNV was most prevalent. We will consider variables reflecting: the fraction of corvids among infected birds; the fractions of Culex pipiens, Culex restuans, and Culex tarsalis mosquitoes among infected mosquitoes; human population density; the fraction of individuals older than age 65; the poverty rate; geographical location; temperature; and precipitation. Modeling the probability of a fatal outcome in terms of these surveillance and demographic variables will characterize the populations to which WNV poses the greatest threat.
METHODS
Data acquisition
We contacted state health departments and visited their web sites to compile data for the 13 states with 100 or more human WNV cases during 2003 (CO, IA, LA, MN, MT, NM, ND, NE, OH, PA, SD, TX, WY).22 Of the 9,862 cases reported nationwide that year, 8,835 took place in these 13 states; moreover, 199 of the 264 deaths reported nationwide occurred in these states.23 The data we sought included: numbers of human cases and deaths in each county; numbers of positive birds and positive corvids in each county; and numbers of positive mosquito pools, positive mosquito pools containing Culex pipiens, positive mosquito pools containing Culex restuans, and positive mosquito pools containing Culex tarsalis in each county.
We were able to obtain the numbers of human cases and deaths in each county for nine of the states (CO, MN, MT, NM, OH, PA, SD, TX, WY); there were 432 counties with cases in these nine states. For the other four states, we acquired the statewide numbers of cases and deaths from the Centers for Disease Control and Prevention (CDC) web page.23 We were also able to obtain much of the desired data about avian and mosquito infections for most of these 436 geographical units (432 counties and four states).
The population density from the year 2000, the percentage of individuals older than age 65 for 2000, and the 1999 poverty rate were acquired from the U.S. Census Bureau for 435 of the 436 geographical units.24 Data on average temperature and average annual precipitation were recovered from the National Water and Climate Center.25 We estimated figures for Broomfield County in Colorado, which did not exist in 2000, based on figures for adjacent counties and on the contents of that county's web page.26
Variable definitions
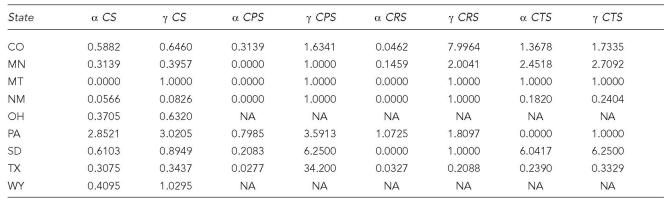
To create a variable reflecting the fraction of corvids among infected birds, we used (parametric) empirical Bayes methodology.27 If many birds tested positive in a particular county, a reasonable proxy for the fraction of corvids among infected birds in that county would be the number of corvids testing positive divided by the total number of birds testing positive. However, if there were very few positive birds in a county, it is unlikely that such a quotient would approximate the fraction of corvids among infected birds; if there were no positive birds, such a quotient would not even be defined. The empirical Bayes methodology allowed us to incorporate information from other counties in the same state when there were very few or no positive birds in a particular county. As a first step, we calculated the aforementioned quotients for all counties with at least one positive bird. For a given state, let m1 and m2 denote the mean and variance of the quotients for that state's counties. Following formula A.3 in Bayesian Data Analysis,27 we set γ= [m1(1 − m1)/m2] − 1 and α = m1γ. We then defined a corvid share (CS) variable for each county in the state by CS=(positive corvids in county+α)/(positive birds in county+γ).
Note that α/γ=m1 is roughly equal to the statewide number of positive corvids divided by the statewide number of positive birds. Values of α and γ for each state are presented in Table 1. For the four states that were themselves geographical units, we defined CS by
| CS=(positive corvids in state)/(positive birds in state). |
Table 1.
Empirical Bayes calculations for CS, CPS, CRS, and CTS
CS = corvid share
CPS = Culex pipiens share
CRS = Culex restuans share
CTS = Culex tarsalis share
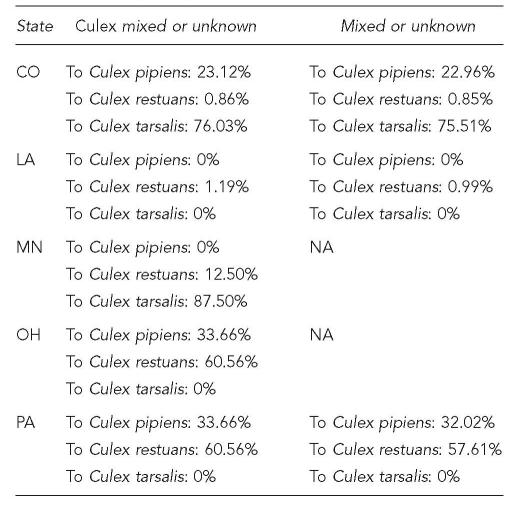
To create variables reflecting the fractions of Culex pipiens, Culex restuans, and Culex tarsalis mosquitoes among infected mosquitoes, we began by allocating ambiguously classified positive pools (i.e., Culex mixed species, Culex unknown species, mixed species, unknown species) to Culex pipiens, Culex restuans, and Culex tarsalis in appropriate percentages based on statewide species breakdowns of positive mosquito pools (Table 2). We defined a Culex pipiens share (CPS) variable for each county, except in Ohio and Wyoming, by CPS=(positive Culex pipiens pools in county+α)/(positive mosquito pools in county+γ), where values for α and γ were again calculated using an empirical Bayes approach (Table 1). Regarding Ohio, for which positive mosquito pools were not classified specifically except at the state level, we calculated the statewide CPS value, CPS=(positive Culex pipiens pools in state)/(positive mosquito pools in state), and assigned it to each county. Regarding Wyoming, for which we had no information about positive mosquito pools, we assigned to each county the average of the statewide CPS values from the adjacent states Montana, South Dakota, and Colorado. Such an assignment is simply nearest-neighbor smoothing, with Wyoming as the region of interest and Montana, South Dakota, and Colorado as the neighbors over which an average is taken. As documented in Waller and Gotway,28 nearest-neighbor smoothing is a viable strategy for data analysis in public health when a proportion or rate cannot be estimated reliably from data in the region of interest.
Table 2.
Allocations of ambiguously classified positive mosquito pools
Statewide CPS values were obtained for Louisiana and North Dakota. We had little information about positive mosquito pools for Iowa and Nebraska; we assigned to Iowa the average of the statewide CPS values from South Dakota and Minnesota, and assigned to Nebraska the average of the statewide CPS values from Colorado and South Dakota.
The Culex restuans share (CRS) and Culex tarsalis share (CTS) variables were defined analogously.
Let LPD denote the natural logarithm of the population density from year 2000, SEN the 2000 fraction of individuals older than age 65, and POV the 1999 poverty rate. We worked with LPD rather than population density itself because the distribution of population densities across counties is highly skewed and we wanted to avoid making heavily populated counties unduly influential.
Let WE denote an indicator variable for western geographical location; that is, WE=1 for any county in a state (or state) principally west of the Mississippi River, and WE=0 for any county in a state principally east of the Mississippi River. Since WNV has spread from the eastern United States to the western United States, we wanted to be able to distinguish eastern locations from western locations should such a distinction be useful in predicting case outcomes.
Finally, let TEMP denote the average temperature (Fahrenheit) and PREC the average annual precipitation (inches). Climate and weather, among other factors not easily quantified, are known to affect vector populations.4 Also, it seems possible that a case outcome may depend on the environment, which is influenced by climate and weather.
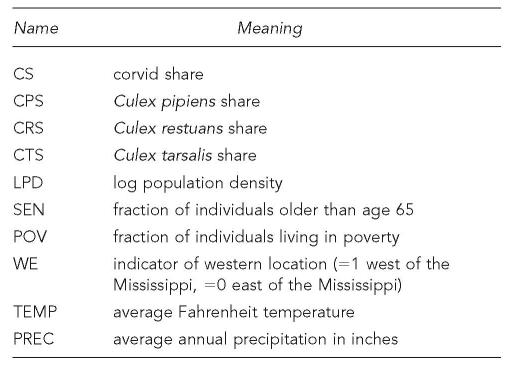
The variables are listed in Figure 1.
Figure 1.
List of variable names and meanings
Statistical modeling
Let f denote the probability of a fatal outcome for a person identified as having acquired WNV, given knowledge of the geographical unit in which the individual resides. The observed case fatality rate in the geographical unit is a crude estimate of f. We employed the logistic regression capabilities of SAS, version 9.1,29 to fit the following preliminary model:
The preliminary model expresses the log odds of a fatal outcome in terms of all ten surveillance and demographic variables. For any number c, exp[cβ1] is the factor by which the odds of a fatal outcome are multiplied if CS is increased by c units while the other variables in the model are fixed. Similar interpretations are available for exp[cβ2], exp[cβ3], and so forth.
We decided a priori to apply backward elimination with a significance threshold of 0.05 to obtain a final model involving only the variables most useful in predicting case outcomes: a model with fewer variables is more amenable to interpretation and typically yields smaller standard errors (i.e., more precise parameter estimates).
We also performed two sensitivity analyses. The first sensitivity analysis excluded data from the states (Wyoming, Iowa, and Nebraska) for which we had to define CPS, CRS, and CTS by borrowing information from other states. The purpose of this sensitivity analysis was to confirm empirically that the nearest-neighbor smoothing did not introduce substantial biases. The second sensitivity analysis entailed fitting a model that related statewide case fatality rates to state-level surveillance and demographic variables for the 13 states with at least 100 WNV cases. The purpose of this sensitivity analysis was to assess how the results could be influenced by the sizes of the geographic units.
RESULTS
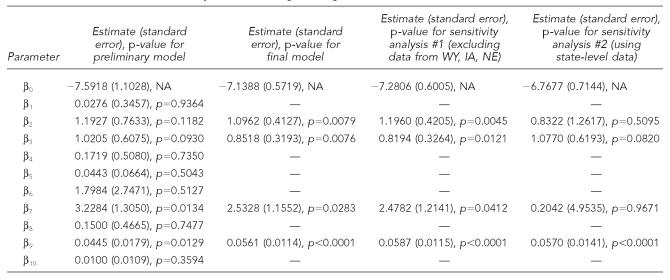
The parameter estimates for the preliminary model are supplied with their standard errors and p-values in Table 3; p-values less than 0.05 identify parameter estimates that are significantly different from zero. Only POV and TEMP had p-values less than 0.05; except for CPS and CRS, all other variables had p-values greater than 0.15.
Table 3.
Parameter estimates and p-values for logistic regression models
Backward elimination with a significance threshold of 0.05 led to the removal of CS, WE, CTS, SEN, LPD, and PREC. Choosing a more liberal significance threshold of 0.10 would not have affected backward elimination for this data set.
The final model is:
The parameter estimates, standard errors, and p-values for the final model are presented in Table 3. The odds of a fatal outcome are estimated to increase by a multiplicative factor of 1.011=exp[0.01×1.0962] for every one percent increase in CPS and by a factor of 1.009 for every one percent increase in CRS, suggesting that fatalities may be more likely in areas where Culex pipiens and Culex restuans mosquitoes are the primary vectors. Moreover, the odds of a fatal outcome are estimated to increase by a factor of 1.026 for every one percent increase in the poverty rate and by a factor of 1.058 for every one degree increase in the average temperature.
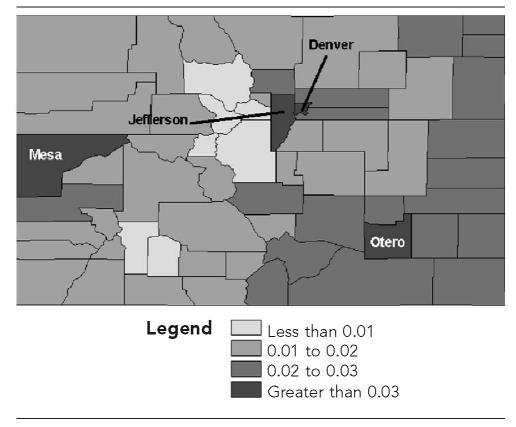
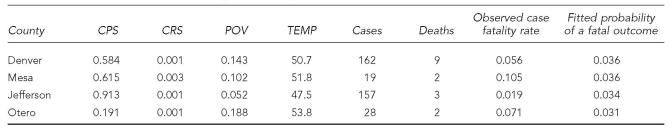
Figure 2 depicts the fitted probabilities of a fatal outcome (i.e., model-based estimates of f) for counties in the state of Colorado. There are four counties (Denver, Mesa, Jefferson, Otero) with fitted probabilities greater than 0.03. Table 4 shows the actual numbers of WNV cases and deaths in these four counties along with the values of CPS, CRS, POV, and TEMP. The fitted probabilities are in reasonable agreement with the observed case fatality rates; for example, there is a 15% chance of having two or more deaths among 19 cases if f= 0.036. Jefferson County had an exceptionally high value of CPS, although it had a low value of POV. Jefferson County was also the only one of the four in which the actual number of deaths was less than what would have been predicted by the model (actual: 3, predicted: 157×0.034≈5). Otero County had a value of POV more than double the statewide poverty rate of 0.093, although it had a rather low value of CPS. Denver and Mesa Counties were moderately high on both POV and CPS. All four counties were rather similar on CRS and TEMP.
Figure 2.
Fitted probabilities of a fatal outcome
Table 4.
Counties in Colorado with highest fitted probabilities of a fatal outcome
CPS = Culex pipiens share
CRS = Culex restuans share
POV = poverty rate
TEMP = average temperature
For the first sensitivity analysis, we refit the final model excluding the data from Wyoming, Iowa, and Nebraska (Table 3). None of the parameter estimates was qualitatively different, and none of the p-values escalated above 0.05. For the second sensitivity analysis, we refit the final model using state-level data instead of (mostly) county-level data (Table 3). The estimates for β0, β2, β3, and β9 did not change dramatically; however, the standard errors were larger, yielding noticeably larger p-values for CPS and CRS. The estimate of β7 decreased substantially, but this is intuitively reasonable: POV is more heterogeneous across counties than across states, so the role of poverty should be more difficult to ascertain with state-level data.
DISCUSSION
The role of poverty
Populations in areas with high poverty rates appear to face a greater threat from WNV. This finding accords with previous research not focused on WNV specifically: people living in low socioeconomic status neighborhoods are more likely to die prematurely than those living in high socioeconomic status neighborhoods.30 An understanding of why certain populations are more vulnerable (in this instance, to fatal outcomes from WNV) may have implications for public health officials and other policy makers regarding efforts at health promotion and the reduction of health disparities.30,31 In particular, community educational programs can encourage residents to take inexpensive protective measures to reduce the risk of WNV infection. The judicious administration of mosquito spraying programs is imperative; reducing the number of infected mosquitoes through adulticiding and larviciding has been shown to decrease the incidence of WNV among humans.32
There are several reasons why people living in poverty-stricken areas may be more vulnerable to fatal outcomes. Poverty may limit both an individual's seeking and receiving medical care; a delay in receiving care, or receiving limited care, may result in a poor or fatal outcome. An individual living in poverty may be more likely to experience a fatal outcome even if medical care is received promptly, especially if the person is afflicted by other co-morbidities linked to a history of insufficient preventive care. Immunosuppressive disorders and other chronic conditions may be more prevalent in poverty-stricken areas.33 Environmental factors must not be overlooked. The homes of the poor may lack air conditioning and window screening, resulting in greater exposure to infected mosquitoes. Environmental factors also suggest why higher temperatures may correspond to elevated case fatality rates. People are more likely to leave windows open and to wear less protective clothing; infected individuals may fare less well since higher temperatures can be difficult to endure for a person whose health has been compromised.
Remarks on study design
In principle, a case-control design with individual-level data would have been ideal. However, acquiring individual-level data for a WNV study of national scope is infeasible. Even county-level summary data are not generally available to researchers; when they are available, they are not necessarily well-organized. Preservation of the national scope was essential for assessing the roles of variables that fluctuate widely across states but not much within states (e.g., TEMP). In sum, an ecological design with (mostly) county-level data provided the only feasible option for investigating all demographic and surveillance variables of interest.
Modeling issues and limitations
Aside from the inferential challenges inherent to ecological studies in general,28 there are a few modeling issues and limitations specific to this study that must be described.
The absence of a variable reflecting the counties' (and states') mosquito control programs must be acknowledged as a limitation. If we had sufficient information to define such a variable, we would certainly want to investigate whether it had a relationship with case fatality rates.
The definitions of CS, CPS, CRS, and CTS warrant comment. We felt that defining these variables as fractions rather than as counts (e.g., the fraction of corvids among birds testing positive rather than the total number of positive corvids) would mitigate the bias due to differing policies on avian and mosquito testing. However, such bias could not be completely avoided. If a county decided to test only certain species of birds, the fraction of corvids among birds testing positive could overstate the fraction of corvids among all infected birds in that county. Even in the absence of differing policies on avian and mosquito testing, there would still be difficulties. For example, the scavenging of small non-corvids could still cause CS to overstate the fraction of corvids among infected birds. Nonetheless, the recent change in neurovirulence11 suggests that the evolution and behavior of WNV may depend on the primary hosts and vectors; as such, some attempt must be made to define variables reflecting the primary hosts and vectors.
Finally, we must comment on the interpretation of f and the observed case fatality rates. Strictly speaking, they do not reflect probabilities of a fatal outcome for any person who has acquired WNV; they reflect probabilities of a fatal outcome for a person identified as having acquired WNV. The distinction is subtle but important—presumably thousands of individuals were infected in 2003 who did not develop strong enough symptoms to be identified as cases.
Remarks on data dissemination
Since treating counties as the units of analysis (where possible) was preferable to treating states as the units of analysis, we invested considerable effort in amassing county-level WNV data. We found that the various state health departments had radically different conventions for recording, organizing, and disseminating county-level WNV data. While these differing conventions may not complicate analyses confined to any one state, they do make analyzing data from multiple states a formidable task. Adoption of a uniform protocol for recording, organizing, and disseminating county-level WNV data (including information about mosquito control programs) might allow trends across states to be perceived more quickly and studied more effectively, providing a stronger basis for decisive action by public health practitioners.
Conclusions
Populations in poverty-stricken areas appear to be more vulnerable to fatal outcomes from WNV. Hence, effective WNV educational programs and control measures are vital for these areas. In addition, a uniform protocol for disseminating county-level data could facilitate timely responses to WNV outbreaks and to emerging infectious diseases more generally.
Acknowledgments
The authors thank the Editorial Board and the anonymous referees for suggestions that greatly improved the paper. They also thank Jeff Jones, PhD, for assistance in preparing Figure 2. Finally, the authors thank the state epidemiologists and other public health staff who provided data for this study.
REFERENCES
- 1.Nash D, Mostashari F, Fine A, Miller J, O'Leary D, Murray K, et al. The outbreak of West Nile virus infection in the New York City area in 1999. N Engl J Med. 2001;344:1858–9. [Google Scholar]
- 2.Mostashari F, Bunning ML, Kitsutani PT, Singer DA, Nash D, Cooper MJ, et al. Epidemic West Nile encephalitis, New York, 1999: results of a household-based seroepidemiological survey. Lancet. 2001;358:261–4. doi: 10.1016/S0140-6736(01)05480-0. [DOI] [PubMed] [Google Scholar]
- 3.Lopez W. West Nile virus in New York City. Am J Public Health. 2002;92:1218–21. doi: 10.2105/ajph.92.8.1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reisen W, Lothrop H, Chiles R, Madon M, Cossen C, Woods L, et al. West Nile virus in California. Emerg Infect Dis. 2004;10:1369–78. doi: 10.3201/eid1008.040077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aquino M, Fyfe M, MacDougall L, Remple V. Protective behavior survey, West Nile virus, British Columbia. Emerg Infect Dis. 2004;10:1499–501. doi: 10.3201/eid1008.031053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smithburn KC, Hughes TP, Burke AW, Paul JH. Neurotropic virus isolated from the blood of a native of Uganda. Am J Trop Med Hyg. 1940;4:471. [Google Scholar]
- 7.Miller BR, Nasci RS, Godsey MS, Savage HM, Lutwama JJ, Lanciotti RS, Peters CJ. First field evidence for natural vertical transmission of West Nile virus in Culex univittatus complex mosquitoes from Rift Valley province, Kenya. Am J Trop Med Hyg. 2000;62:240. doi: 10.4269/ajtmh.2000.62.240. [DOI] [PubMed] [Google Scholar]
- 8.Murray PR, Rosenthal KS, Kobayashi GS, Pfaller MA. Togaviruses and flaviruses. In: Schmitt W, Grigg LL, editors. Medical microbiology. 4th ed. St. Louis: Mosby; 2002. pp. 562–3. [Google Scholar]
- 9.Theophilides CN, Ahearn SC, Grady S, Merlino M. Identifying West Nile virus risk areas: the Dynamic Continuous-Area Space-Time system. Am J Epidemiol. 2003;157:843–54. doi: 10.1093/aje/kwg046. [DOI] [PubMed] [Google Scholar]
- 10.Yaremych SA, Warner RE, Mankin PC, Brawn JD, Raim A, Novak R. West Nile virus and high death rate in American crows. Emerg Infect Dis. 2004;10:709–11. doi: 10.3201/eid1004.030499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gea-Banacloche J, Johnson RT, Bagic A, Butman JA, Murray PR, Agrawal AG. West Nile virus: pathogenesis and therapeutic options. Ann Intern Med. 2004;140:545–53. doi: 10.7326/0003-4819-140-7-200404060-00015. [DOI] [PubMed] [Google Scholar]
- 12.Update: West Nile virus activity—eastern United States, 2000. MMWR Morb Mortal Wkly Rep. 2000;49(46):1044–7. [PubMed] [Google Scholar]
- 13.Turell MJ, O'Guinn M, Oliver J. Potential for New York mosquitoes to transmit West Nile virus. Am J Trop Med Hyg. 2000;62:413–4. doi: 10.4269/ajtmh.2000.62.413. [DOI] [PubMed] [Google Scholar]
- 14.Turell MJ, O'Guinn ML, Dohm DJ, Jones JW. Vector competence of North American mosquitoes (Diptera: Culicidae) for West Nile virus. J Med Entomol. 2001;38:130–4. doi: 10.1603/0022-2585-38.2.130. [DOI] [PubMed] [Google Scholar]
- 15.Tsai TF, Popovici F, Cernescu C, Campbell GL, Nedelcu NI. West Nile encephalitis epidemic in southeastern Romania. Lancet. 1998;352:767–71. doi: 10.1016/s0140-6736(98)03538-7. [DOI] [PubMed] [Google Scholar]
- 16.Han LL, Popovici F, Alexander JP, Jr, Laurentia V, Tengelsen LA, Cernescu C, et al. Risk factors for West Nile virus infection and meningoencephalitis, Romania, 1996. J Infect Dis. 1999;179:230–3. doi: 10.1086/314566. [DOI] [PubMed] [Google Scholar]
- 17.Turell MJ, O'Guinn ML, Dohm DJ, Webb JP, Jr, Sardelis MR. Vector competence of Culex tarsalis from Orange County, California, for West Nile virus. Vector Borne Zoonotic Dis. 2002l;2:193–6. doi: 10.1089/15303660260613756. [DOI] [PubMed] [Google Scholar]
- 18.Ruiz MO, Tedesco C, McTighe TJ, Austin C, Kitron U. Environmental and social determinants of human risk during a West Nile virus outbreak in the greater Chicago area, 2002. Int J Health Geogr. 2004;3:8. doi: 10.1186/1476-072X-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Iwamoto M, Jernigan DB, Guasch A, Trepka MJ, Blackmore CG, Hellinger WC, et al. Transmission of West Nile virus from an organ donor to four transplant recipients. N Engl J Med. 2003;348:2196–203. doi: 10.1056/NEJMoa022987. [DOI] [PubMed] [Google Scholar]
- 20.Pealer LN, Marfin AA, Petersen LR, Lanciotti RS, Page PL, Stramer SL, et al. Transmission of West Nile virus through blood transfusion in the United States in 2002. N Engl J Med. 2003;349:1236–45. doi: 10.1056/NEJMoa030969. [DOI] [PubMed] [Google Scholar]
- 21.Zohrabian A, Meltzer MI, Ratard R, Billah K, Molinari NA, Roy K, et al. West Nile virus economic impact, Louisiana, 2002. Emerg Infect Dis. 2004;10:1736–44. doi: 10.3201/eid1010.030925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Division of Vector-Borne Infectious Diseases. Links to state and local government West Nile virus web sites. [cited 2004 Aug 14]. Available from: URL: http://www.cdc.gov/ncidod/dvbid/westnile/city_states.htm.
- 23.Centers for Disease Control and Prevention; Division of Vector-Borne Infectious Diseases. West Nile virus: statistics, surveillance, and control. [cited 2004 Aug 14]. Available from: URL: http://www.cdc.gov/ncidod/dvbid/westnile/surv&controlCaseCount03_detailed.htm.
- 24.Census Bureau (US) State and county quickfacts. [cited 2004 Aug 14]. Available from: URL: http://quickfacts.census.gov/qfd.
- 25.National Resources Conservation Service: National Water and Climate Center. Climate information retrieval. [cited 2005 Aug 14]. Available from: URL: http://www.wcc.nrcs.usda.gov/climate/climate-map.html/
- 26.The city and county of Broomfield. [cited 2004 Aug 14]. Available from: URL: http://www.ci.broomfield.co.us/
- 27.Gelman A, Carlin J, Stern H, Rubin D. Boca Raton: Chapman & Hall/CRC; 1995. Bayesian data analysis. [Google Scholar]
- 28.Waller LA, Gotway CA. Hoboken: John Wiley & Sons; 2004. Applied spatial statistics for public health data. [Google Scholar]
- 29.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2003. SAS: version 9.1. [Google Scholar]
- 30.Bosma H, van de Mheen HD, Borsboom GJ, Mackenbach JP. Neighborhood socioeconomic status and all-cause mortality. Am J Epidemiol. 2001;153:363–71. doi: 10.1093/aje/153.4.363. [DOI] [PubMed] [Google Scholar]
- 31.Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91:1783–9. doi: 10.2105/ajph.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bowman C, Gumel AB, van den Driessche P, Wue J, Zhu H. A mathematical model for assessing control strategies against West Nile virus. Bull Math Biol. 2005;67:1107–33. doi: 10.1016/j.bulm.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 33.Hayes EB, Gubler DJ. West Nile virus: epidemiology and clinical features of an emerging epidemic in the United States. Annu Rev Med. 2005;57:187–94. doi: 10.1146/annurev.med.57.121304.131418. [DOI] [PubMed] [Google Scholar]