SYNOPSIS
Objective
This study's objective is to determine if there is an association between rates of violence and rates of childhood asthma in Los Angeles County communities.
Methods
Rates of hospitalization for assault and for asthma were calculated for each ZIP Code and city in Los Angeles County. Linear regression was used to determine the effect of assault rates on asthma rates while controlling for potential confounders such as poverty and racial/ethnic distribution. At the city level, crime rates were included in the model as additional measures of community violence.
Results.
Hospitalization rates for childhood asthma and assaults were significantly correlated at both the city (r=0.80) and the ZIP Code (r=0.54) levels. The association remained significant when controlling for poverty and racial/ethnic distribution with linear regression (p,0.0001). At the city level, the variables measuring the crime rate were not significant predictors of asthma hospitalizations.
Conclusions
Community violence as measured by the rate of assault hospitalizations is associated with childhood asthma in Los Angeles County. Health care providers should consider their asthmatic patients' social environments when devising treatment plans.
Asthma is a leading cause of morbidity in children,1 and if left untreated can result in death.2 Over the last thirty years, the prevalence of asthma in children has risen steadily.3 Based on responses to the National Health Interview Survey, asthma prevalence increased sharply from 1980 to 1996.4 Despite advances in pharmacologic treatments, hospitalizations for childhood asthma also have increased.5 Traditional risk factors for childhood asthma, such as allergens, respiratory tract infections, air pollutants, and tobacco smoke, cannot account fully for this increase.3,6–9
Non-whites and individuals of lower socioeconomic status (SES) are disproportionately represented in the trend of increasing childhood asthma.10–12 Minorities and low SES populations may have greater exposure to the traditional risk factors for asthma mentioned above, which could account for the greater prevalence.5,12–15 In addition, they are often treated at facilities that do not follow the most up-to-date guidelines for asthma care16,17 and may also have limited access to health care. Lower quality and limited access to health care place asthmatic children at greater risk of hospitalization for asthma.
Interestingly, differences in racial/ethnic status and SES may not fully explain why these individuals are more likely to have, and to be hospitalized for, childhood asthma,18 suggesting that other factors may contribute to asthma morbidity.19 Recently, researchers have begun to examine social factors that may affect asthma. Low SES neighborhoods are often characterized by high rates of crime and violence.20 Studies of young inner city children in two large East coast cities found that a large percentage had seen or heard acts of violence.21,22 Community violence is a chronic and pervasive stressor that taxes all members of a community, regardless of each member's individual-level risk.23 There are many potential mechanisms through which community violence-related stress may affect asthmatic children.
Stress may affect children directly, causing biological changes that lead to asthma exacerbations. Research has shown that children exposed to violence experience significantly more negative psychological symptoms, including stress, than unexposed children.21,24–27 General stress has been shown to increase respiratory tract resistance in asthmatic individuals.28,29 Wright has reported a temporal association between violence and self-reported asthma exacerbations.20 Using data from the Inner-City Asthma Study, Wright and Steinbach evaluated the relationship between violence and children's asthma symptoms as reported by caretakers.18 The study found that violent incidents were common in the participating neighborhoods and that the frequency of asthma symptoms increased with increased community violence.18
Exposure to violence may also lead to increased asthma morbidity in children indirectly. Individuals living in violent communities may experience barriers to following their prescribed asthma treatment regimen. Funding may be diverted from primary care and specialty clinics towards programs to address violence.30 Pharmacies may be reluctant to operate 24 hours per day due to fears for safety.20 Even when services are available, individuals may be reluctant to travel outside to obtain asthma medication or to visit their doctors for fear of victimization. One study of hypertensive African Americans from Los Angeles observed that fear of violence was a barrier to keeping medical appointments and following a prescribed exercise regimen.31
Community violence also may decrease individual resources needed to manage childhood asthma. In extreme cases, parents may develop psychological conditions that reduce their ability to care for their asthmatic children.20 Furthermore, violence decreases social cohesion, a factor which may alleviate stress.32 Under stress from violence, parents may be unable to cope with their child's disease, and research has demonstrated that children may adopt their parents' coping mechanisms.33 A child's ability to manage his/her asthma also may be diminished as the result of attitudes that develop when living in a violent environment.34
Finally, behavioral changes in response to community violence may increase children's exposure to risk factors associated with childhood asthma. Parents of children living in violent communities may keep their children indoors for fear of their safety, increasing their exposure to indoor allergens and air pollutants.20 Also, children who play indoors often do so alone, a situation that can result in decreased social networks. This may decrease their ability to cope with general stress and stress due to asthma.32
Previous studies have demonstrated an association between exposure to violence and asthma morbidity in children. Existing studies that ask asthmatic children or their caretakers if they have ever witnessed or been aware of violent incidents measure an individual's experience with violence. However, in a community characterized by high rates of violence, even incidents that individuals did not witness or were personally aware of may increase neighborhood levels of stress. We do not know of any studies that have evaluated overall levels of community violence and its relationship to asthma morbidity. We used assault hospitalization rates and reported crime rates as measures of community violence and examined their association with childhood asthma hospitalization rates in neighborhoods throughout Los Angeles County.
METHODS
This study utilized an ecological design to investigate the association between community violence and asthma hospitalization rates among children. The assault hospitalization rate among all ages for specific geographic areas (ZIP Code and city) was the primary measure of community violence. Additionally, crime rates at the city level were used as measures of community violence. Measures of SES and racial/ethnic diversity were used as potential confounders.
The California Office of Statewide Health Planning and Development (OSHPD) collects patient discharge information from all 128 hospitals in Los Angeles County. For each ZIP Code in Los Angeles County, the number of assault and asthma hospitalizations during 2000 were obtained. A hospitalization was classified as an assault if an International Classification of Disease, 9th Revision (ICD-9) e-code between E960.0 and E969.9 was present in at least one of the e-code variables.35 If a record had at least one ICD-9 diagnosis code between 493.0 and 493.9, it was classified as an asthma hospitalization. The number of assault and asthma hospitalizations in each ZIP Code was further stratified by age (≤20 years, 21–64 years, ≥65 years) and gender.
Counts of assault and asthma hospitalizations by ZIP Code were then converted to counts by city. To do this, a list of all ZIP Codes in Los Angeles County was obtained from the Los Angeles County Department of Health Services. Next, the United States Postal Service website was used to create a list of all cities within each ZIP Code.36 If a ZIP Code had only one city associated with it, all asthma and assault hospitalizations from that ZIP Code were assigned to the city. However, if a ZIP Code contained parts of two or more cities, asthma and assault hospitalizations from that ZIP Code were assigned to each city based on the proportion that city's population contributed to the sum of the total population of all cities associated with that ZIP Code. This was done within each of the age groups and gender strata, using census population data.37
Crime statistics by city were obtained from the California Department of Justice (2000). The California Department of Justice collects information on the number of calls law enforcement officials receive to respond to domestic violence,38 reports of nonviolent crime,39 and reports of violent crime.39 Nonviolent crime includes reports of motor vehicle theft, arson, burglary, and larceny. Violent crime includes willful homicide, forcible rape, robbery, and aggravated assault.
Los Angeles County population data obtained from the 2000 U.S. Census37 were used to calculate hospitalization rates per 10,000 for both children (0–20 years old) and for all ages and to calculate crime rates for each geographic area. U.S. Census data also were used to obtain racial/ethnic diversity and SES measures for each ZIP Code and city. These include the percent non-white,40 percent Hispanic,41 percent African American,40 percent families living in poverty,37 and median before-tax family income.37 Family median income was centered around zero by subtracting the median of the median incomes from each geographic area's median income. Maps of children's asthma hospitalization rates and assault hospitalization rates for all ages for Los Angeles County were created using Arcview version 3.2A.42
Los Angeles County contains 506 ZIP Codes. Of these, 228 P.O. Box ZIP Codes were excluded from analysis, since population data were not available. Of the 278 ZIP Codes remaining, five were excluded; one had no hospitalization data and four had a population of less than twenty. Two additional ZIP Codes were determined to be outliers and were not included in the final analyses. Removal of these ZIP Codes did not change the inferences from the data analyses. The final dataset consisted of 271 Los Angeles County ZIP Codes. There are a total of 88 cities in Los Angeles County. The two cities with the smallest populations (91 and 777) were excluded from analysis. The remaining 86 cities were included in the final dataset for analysis.
Statistical analysis
Statistical analyses were conducted with SAS statistical software.43 The mean, standard deviation, and range were calculated by city, and where applicable, ZIP Code, for the following variables: assault hospitalization rate for all ages, children's assault hospitalization rate, children's asthma hospitalization rate, percent any non-white, percent Hispanic, percent African American, percent of families living in poverty, median family income, rate of calls for service for domestic violence, reported nonviolent crime rate, and reported violent crime rate.
Spearman rank correlation coefficients35,44 were computed by ZIP Code and city to assess the relationships between children's asthma hospitalization rate and assault hospitalization rates, the crime variables, and the sociodemographic variables.
Several univariate linear regression analyses were developed with children's asthma hospitalization rate as the dependent variable. The independent variable was either children's assault hospitalization rate or assault hospitalization rate for all ages or one of the race/ethnicity (either percent non-white or both percent Hispanic and percent African American) or SES (percent of families living in poverty or centered family median income) variables. For city data, models also were fit with each of the three crime variables. Where variables were skewed, we used natural log or square root transformations, if the transformations improved the model fit as judged by adjusted R2.
Multiple regression models were created for both the ZIP Code and city data. In each model, the children's asthma hospitalization rate was the dependent variable and assault hospitalization rate for all ages was the independent variable. To control for potential confounders, each model also contained one of the race/ethnicity and one of the SES variables. At the city level, the three crime rate variables also were included in the model. Based on backwards selection, different models were developed and assessed for statistical significance (p≤0.05), homogenous variance, normality of residuals, and predictive power (R2). Colinearity was assessed in the multivariate linear regression models by examination of the tolerance and variance inflation factor. Based upon examination of the kurtosis, our data were not in a Poisson distribution; therefore, Poisson regression was not used.
RESULTS
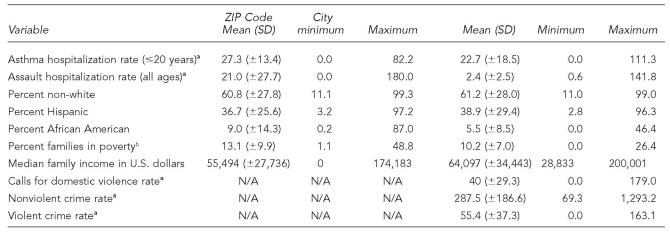
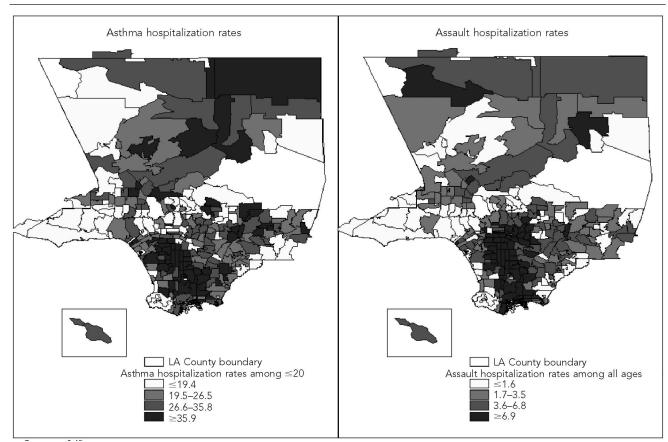
Table 1 shows the mean and standard deviation of the hospitalization, SES, race/ethnicity, and crime variables by ZIP Code and city. Figure 1 depicts children's asthma hospitalization rates and assault hospitalization rates for all ages by ZIP Code in Los Angeles County. These maps show that high rates of both asthma and assault hospitalizations tend to cluster in the same ZIP Codes.
Table 1.
Descriptive statistics—hospitalization rates, sociodemographic characteristics, and reported crime, Los Angeles County ZIP Codes and cities, 2000
All rates are per 10,000 population.
The poverty threshold is defined as $16,895 for a family of four according to the U.S. Census Bureau Population Survey (1999).
CI = confidence interval
N/A: These variables are not available at the ZIP Code level.
Figure.
Hospitalization rates for asthma among ≥20-year-olds and assaults among all ages by ZIP Code, Los Angeles County, 2000
SOURCE: Office of Statewide Health Planning and Development Hospital Discharge Data
NOTE: All rates are per 10,000 population.
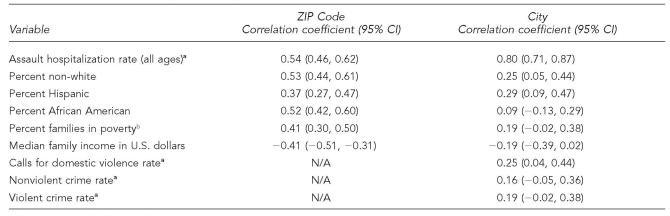
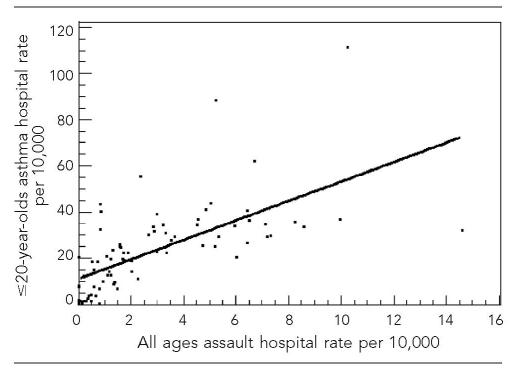
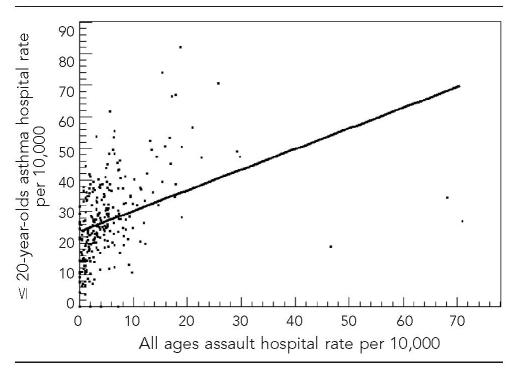
Spearman correlations between children's asthma hospitalization rate and the other variables of interest are shown in Table 2 for Los Angeles County ZIP Codes and cities. At the ZIP Code level, children's asthma hospitalization rate was positively correlated with children's assault hospitalization rate, assault hospitalization rate for all ages, percent non-white, percent Hispanic, percent African American, and percent of families living in poverty. Children's asthma hospitalization rate was also negatively correlated with median family income. At the city level, children's asthma hospitalization rate was positively correlated with children's assault hospitalization rate, assault hospitalization rate for all ages, percent non-white, percent Hispanic, and domestic violence crime rate. The percent African American, both the SES variables, and the remaining two crime rate variables were not significantly correlated with children's asthma hospitalization rate at the city level. The correlations between the asthma and assault hospitalization rates are visualized in Figures 2 and 3. The two variables were more strongly correlated at the city level (Figure 2; r=0.81) than at the ZIP Code level (Figure 3; r=0.54).
Table 2.
Spearman rank correlation coefficients between annual asthma hospitalizations in children and other variables, Los Angeles County ZIP Codes and cities, 2000
All rates are per 10,000 population.
The poverty threshold is defined as $16,895 for a family of four according to the U.S. Census Bureau Population Survey (1999).
CI = confidence interval
N/A: These variables are not available at the ZIP Code level.
Figure.
Correlation between childhood asthma hospitalizations and assault hospitalizations for all ages at the city level
Figure.
Correlation between childhood asthma hospitalizations and assault hospitalizations for all ages at the ZIP Code level
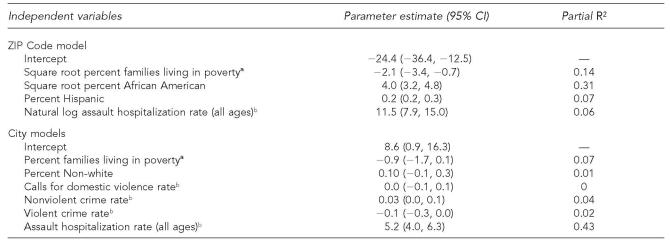
The best-fit variables from the univariate regressions were included in multiple regression analyses. The children's asthma hospitalization rate was the dependent variable in all models. At the ZIP Code level, the best-fit multiple linear regression model (R2=0.58), included as predictors the square root percent families living in poverty, square root percent African American, percent Hispanic, and natural log of assault hospitalization rate. Thirty-one percent of the variance in children's asthma hospitalization rate was accounted for by the square root percent African American variable. The next greatest contributor was square root percent families living in poverty, accounting for 14% of the variance. Percent Hispanic accounted for 7% of the variance in children's asthma hospitalization rate and the natural log of assault hospitalization rate (all ages) accounted for 6%. Colinearity was not a problem in this final model.
The best-fit model at the city level contained percent families living in poverty, percent non-white, domestic violence crime rate, nonviolent crime rate, violent crime rate, and assault hospitalization rate (all ages). Table 3 displays the results from this model. The overall model accounted for 54% of the variance in children's asthma hospitalization rate. The greatest contributor to the variance was assault hospitalization rate (all ages), which accounted for 43% of the variance of children's asthma hospitalization rate. Next, percent of families living in poverty accounted for 7% of the variance in children's asthma hospitalization rate and the nonviolent crime rate accounted for 4% of the variance. Percent non-white, domestic violence crime rate, and the violent crime rate were not significant predictors of children's asthma hospitalization rate in the final model.
Table 3.
Final multiple regression models with childhood asthma hospitalization rate as dependent variable, Los Angeles County ZIP Codes and cities
The poverty threshold is defined as $16,895 for a family of four according to the U.S. Census Bureau Population Survey (1999).
All rates are per 10,000 population.
CI = confidence interval
DISCUSSION
This ecological study showed a consistent association between hospitalization rates for asthma in individuals younger than age 20 and hospitalizations for assaults. In general, our results are consistent with previous findings.5,10,11,18,45,46 Two of the three racial/ethnic variables in the study (percent non-white and percent Hispanic) were correlated with asthma hospitalization rates at both the ZIP Code and the city levels. The third variable, percent African American, was correlated with asthma hospitalization only by ZIP Code. Several small area analyses conducted throughout the country have found correlations between the size of an area's minority population and the rate of asthma hospitalization.5,10,11,17 Both SES variables were significantly correlated with childhood asthma hospitalization rates by ZIP Code, but not by city. Other research has also found associations between these SES measures and asthma hospitalization rates.11,17
While both ZIP Code and city level results are similar to previous research, the data from the two geographic levels are not identical. At the city level, the correlation coefficients for each of these five variables were smaller than at the ZIP Code level, and only two (percent non-white and percent Hispanic) reached significance. The results at the ZIP Code level are more reliable since aggregation of the data into cities creates larger, more heterogeneous areas and results in a smaller sample size. A power analysis also shows that with 271 ZIP Codes there is a power of 99.9% to detect a significant correlation of 0.3 at alpha=0.05; however, with only 86 cities, the power to detect a correlation of 0.3 drops to 81%. Therefore, the Spearman correlations at the ZIP Code level are likely more accurate.
The results of this study indicate that community violence is associated with community-level estimates of children's hospitalization rates for asthma. Our main measure of community violence, the assault hospitalization rate for all ages, was strongly associated with hospitalization rates for childhood asthma after adjustment for racial/ethnic distribution and SES. Assault hospitalization rates accounted for 6% of the variance in childhood asthma hospitalization rates at the ZIP Code and 43% at the city level. The difference in partial R2 may largely be due to the vastly different models that were used for the two geographic levels. The city model contained crime related predictors that were not available at the ZIP Code level and the results were based on a much smaller number of areas. Since violence is one of several factors that may impact asthma morbidity and because the ZIP Code regressions are likely more reliable due to the increased sample size, the 6% partial R2 result from the ZIP Code regression seems more reasonable.
The measures of crime did not have as much effect on asthma hospitalization rates when controlling for race/ethnicity and SES. Nonviolent crime was weakly significant in the final regression model, which suggests nonviolent crime in a community may act as a stressor for individuals living there. We also found that violent crime rates had a significant, but negative, effect on childhood asthma hospitalizations. This was unexpected since violent crime has been identified as a community stressor.47 The third crime measure, domestic violence rate, was not significantly associated with childhood asthma hospitalization rates. This may be because domestic violence is less common than other forms of community violence27 and may be more likely to take place in private locations. From 1993 to 1998, more than 80% of domestic violence incidents occurred in or near the victim's home or in the home of a friend or neighbor,48 while only 36% of all violent crimes were committed in the same locations during 1998.49
The weak relationships between asthma and all crime variables in this study may be partially due to high levels of underreporting. Only around half of all domestic violence victims reported the crime to police from 1993 to 1998.48 Reporting for other types of crimes is also poor. More than 60% of violent, personal, and property crimes are not reported to law enforcement.50 This severe underreporting would tend to bias our results toward the null. In addition, the underreporting of crime potentially explains the unexpected result of a negative association between violent crime and asthma. If communities with high levels of asthma are less likely to report crime, this might lead to the results found here.
This study faces several other limitations. While the ecological approach has been advocated as the most appropriate way to study exposure to community violence,47 the ecological design of our study prohibits drawing any inferences about the effect community violence has on an individual's asthma morbidity.51 The results at the ZIP Code level are likely more reliable than city-level results since the use of smaller, more homogeneous areas may reduce aggregation bias in ecological studies.52
The use of hospital discharge data also introduces some problems. The data do not include each patient's city of residence. The method we used to determine the number of hospitalizations from each city introduces error, since our procedure tends to overrepresent large cities. In addition, the discharge data do not allow for the identification of multiple hospitalizations by the same individual. This is a source of bias, since hospitalized asthma patients are at greater risk for readmission for other reasons (e.g., inability to have access to medications, etc.) in areas with increased hospitalizations for assaults.53 In one study, patients with multiple admissions for asthma made up more than one third of all admissions for asthma.54
Another problem is that hospitalization rates for all conditions can vary geographically, and thus the demonstrated relationship between asthma and assault hospitalizations may be a function of overall geographic variation in hospitalization rates. However, we found that assault hospitalizations were not correlated with hospitalizations for childhood pneumonia and influenza (ZIP Code level Spearman correlation coefficient=−0.08; p=0.21). Thus, while some of the relationship between asthma and assault hospitalizations can, perhaps, be explained by overall geographic variation in the rate of hospitalization, it is likely that a true relationship exists.
The potential for large undercounts in the census data is also a problem since we used the census for race/ethnicity and SES measures as well as the population data. In 1990, the undercount rate for Los Angeles County was 3.3% overall and 5.0% for children; this was much higher for African Americans, with an undercount of 7.8% overall and 12.1% for children.55
Finally, we were unable to find data for several factors which may influence asthma rates. We were not able to locate either air quality or smoking prevalence data at the ZIP Code or city level for Los Angeles County.
Despite these limitations, this study suggests that community violence may act as an additional risk factor for asthma hospitalizations in children. The effects of violence are felt throughout a community, not just by its immediate victims. Los Angeles County is characterized by high rates of community violence. In addition, approximately two thirds of Los Angeles County residents are of non-white decent and almost one in five live below the poverty level.37,40,41 Being non-white and/or of lower SES is associated with greater asthma morbidity, and the additional factor of community violence further adds to the asthma burden experienced by this population.
The failure to address the reasons for health disparities such as those seen in rates of childhood asthma across non-white racial/ethnic groups and levels of SES has significant detrimental public health, social, and economic consequences.56 It is essential that policies and clinical interventions aimed at reducing exposure to violence and/or counseling victims and witnesses of violence be adopted. Policies targeted to improve life opportunities and living conditions may increase social cohesion and decrease violence in high risk communities.20 By addressing the issue of community violence, the disproportionate burden of asthma morbidity of non-white and/or lower SES individuals may be reduced.
REFERENCES
- 1.Neri M, Spanevello A. Chronic bronchial asthma from challenge to treatment: epidemiology and social impact. Thorax. 2000;55(Suppl 2):S57–8. doi: 10.1136/thorax.55.suppl_2.S57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arrighi HM. US asthma mortality: 1941 to 1989. Ann Allergy Asthma Immunol. 1995;74:321–6. [PubMed] [Google Scholar]
- 3.Platts-Mills T, Perzanowski M, Carter MC, Woodfolk JA. The rising prevalence and severity of asthma in western society: are the causes of asthma the causes of the increase? In: Platts-Mills T, editor. Asthma: causes and mechanisms of an epidemic inflammatory disease. Boca Raton (FL): Lewis Publishers; 1999. pp. 1–21. [Google Scholar]
- 4.Surveillance for asthma—United States, 1980–1999. MMWR Surveill Summ. 2002;51(SS-01):1–13. [PubMed] [Google Scholar]
- 5.Ray N, Thamer M, Fadillioglu B, Gergen P. Race, income, urbanicity, and asthma hospitalization in California. Chest. 1998;113:1277–84. doi: 10.1378/chest.113.5.1277. [DOI] [PubMed] [Google Scholar]
- 6.Rosenwasser L. The contribution of genes and environment to asthma. In: Platts-Mills T, editor. Asthma: causes and mechanisms of an epidemic inflammatory disease. Boca Raton (FL): Lewis Publishers; 1999. pp. 225–31. [Google Scholar]
- 7.Rees WL. Etiological factors in asthma. Psychiatr J Univ Ottawa. 1980;5:250–4. [Google Scholar]
- 8.Heyman P, Alarcon AD, Zambrano J, Rakes G. The risk of developing asthma during childhood. Asthma: causes and mechanisms of an epidemic inflammatory disease. In: Platts-Mills T, editor. Boca Raton (FL): Lewis Publishers; 1999. pp. 49–62. [Google Scholar]
- 9.Etzel RA. How environmental exposures influence the development and exacerbation of asthma. Pediatrics. 2003;112(1 Pt 2):233–9. [PubMed] [Google Scholar]
- 10.Wissow L, Gittelsohn A, Szklo M, Starfield B, Mussman M. Poverty, race, and hospitalization for childhood asthma. Am J Public Health. 1988;78:777–82. doi: 10.2105/ajph.78.7.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gottlieb D, Beiser A, O'Connor G. Poverty, race, and medication use are correlates of asthma hospitalization rates. Chest. 1995;108:28–35. doi: 10.1378/chest.108.1.28. [DOI] [PubMed] [Google Scholar]
- 12.Hynes HP, Brugge D, Osgood ND, Snell J, Vallarino J, Spengler J. “Where does the damp come from?” Investigations into the indoor environment and respiratory health in Boston public housing. J Public Health Policy. 2003;24:401–26. [PubMed] [Google Scholar]
- 13.Volmer T. The socio-economics of asthma. Pulm Pharmacol Ther. 2001;14:55–60. doi: 10.1006/pupt.2000.0268. [DOI] [PubMed] [Google Scholar]
- 14.Stevenson LA, Gergen PJ, Hoover DR, Rosenstreich D, Mannino DM, Matte TD. Sociodemographic correlates of indoor allergen sensitivity among United States children. J Allergy Clin Immunol. 2001;108:747–52. doi: 10.1067/mai.2001.119410. [DOI] [PubMed] [Google Scholar]
- 15.Rosenstreich DL, Eggleston P, Kattan M, Baker D, Slavin RG, Gergen P, et al. The role of cockroach allergy and exposure to cockroach allergens in causing morbidity among inner-city children with asthma. New Engl J Med. 1997;336:1356–63. doi: 10.1056/NEJM199705083361904. [DOI] [PubMed] [Google Scholar]
- 16.Evans D, Mellins R, Lobach K, Ramos-Bonoan C, Pinkett-Heller M, Weisemann S, et al. Improving care for minority children with asthma: professional education in public health clinics. Pediatrics. 1997;99:252–4. doi: 10.1542/peds.99.2.157. [DOI] [PubMed] [Google Scholar]
- 17.Carr W, Zeitel L, Weiss K. Variations in asthma hospitalizations and deaths in New York City. Am J Public Health. 1992;82:59–65. doi: 10.2105/ajph.82.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wright R, Mitchell H, Visness C, Cohen S, Stout J, Evans R, Gold DR. Community violence and asthma morbidity: the Inner-City Asthma Study. Am J Public Health. 2004;94:625–32. doi: 10.2105/ajph.94.4.625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiss KB, Gergen PJ, Crain EF. Inner-city asthma: the epidemiology of an emerging US public health concern. Chest. 1992;101(6 Suppl):362S–367S. doi: 10.1378/chest.101.6.362s. [DOI] [PubMed] [Google Scholar]
- 20.Wright RJ, Steinbach SF. Violence: an unrecognized environmental exposure that may contribute to greater asthma morbidity in high risk inner-city populations. Environ Health Perspect. 2001;109:1085–9. doi: 10.1289/ehp.011091085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hurt H, Malmud E, Brodsky NL, Giannetta J. Exposure to violence: psychological and academic correlates in child witnesses. Arch Pediatr Adolesc Med. 2001;155:1351–6. doi: 10.1001/archpedi.155.12.1351. [DOI] [PubMed] [Google Scholar]
- 22.Taylor L, Zuckerman B, Harik V, McAlister-Groves B. Witnessing violence by young children and their mothers. J Dev Behav Pediatr. 1994;15(2):120–3. [PubMed] [Google Scholar]
- 23.Haan M, Kaplan G, Syme S. Socioeconomic status and health: old observations and new thoughts. In: Bunker J, Gomby D, Kehrer B, editors. Pathways in health. Menlo Park (CA): Henry J. Kaiser Family Foundation; 1989. pp. 76–135. [Google Scholar]
- 24.Boney-McCoy S, Finkelhor D. Psychosocial sequelae of violent victimization in a national youth sample. J Consult Clin Psychol. 1995;63:726–36. doi: 10.1037//0022-006x.63.5.726. [DOI] [PubMed] [Google Scholar]
- 25.Cooley-Quille M, Boyd RC, Frantz E, Walsh J. Emotional and behavioral impact of exposure to community violence in inner-city adolescents. J Clin Child Psychol. 2001;30:199–206. doi: 10.1207/S15374424JCCP3002_7. [DOI] [PubMed] [Google Scholar]
- 26.Martinez P, Richters JE. The NIMH Community Violence Project: II. Children's distress symptoms associated with violence exposure. Psychiatry. 1993;56:22–35. doi: 10.1080/00332747.1993.11024618. [DOI] [PubMed] [Google Scholar]
- 27.Wilson WC, Rosenthal BS. The relationship between exposure to community violence and psychological distress among adolescents: a meta-analysis. Violence Vict. 2003;18:335–52. doi: 10.1891/vivi.2003.18.3.335. [DOI] [PubMed] [Google Scholar]
- 28.Rietveld S, Everaerd W, Creer TL. Stress-induced asthma: a review of research and potential mechanisms. Clin Exp Allergy. 2000;30:1058–66. doi: 10.1046/j.1365-2222.2000.00809.x. [DOI] [PubMed] [Google Scholar]
- 29.Ritz T, Steptoe A, DeWilde S, Costa M. Emotions and stress increase respiratory resistance in asthma. Psychosom Med. 2000;62:401–12. doi: 10.1097/00006842-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Fleming AW, Sterling-Scott RP, Carabello G, Imari-Williams I, Allmond B, Foster RS, et al. Injury and violence in Los Angeles: impact on access to health care and surgical education. Arch Surg. 1992;127:671–6. doi: 10.1001/archsurg.1992.01420060037007. [DOI] [PubMed] [Google Scholar]
- 31.Fong RL. Violence as a barrier to compliance for the hypertensive urban African American. J Natl Med Assoc. 1995;87:203–7. [PMC free article] [PubMed] [Google Scholar]
- 32.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277:918–24. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 33.Smith P, Perrin S, Yule W, Rabe-Hesketh S. War exposure and maternal reactions in the psychological adjustment of children from Bosnia-Hercegovina. J Child Psychol Psychiatry. 2001;42:395–404. [PubMed] [Google Scholar]
- 34.Dempsey M. Negative coping as mediator in the relation between violence and outcomes: inner-city African American youth. A J Orthopsychiatry. 2002;72:102–9. [PubMed] [Google Scholar]
- 35.International Classification of Diseases. 5th ed. Los Angeles: Practice Management Information Corporation; 1999. 9th Revision, Clinical Modification. [Google Scholar]
- 36.United States Postal Service. ZIP Code lookup. [cited 2006 Jul 26]. Available from: URL: http://zip4.usps.com/zip4/citytown_zip.jsp.
- 37.Census Bureau (US) Census 2000 summary file 1 (SF-1). DP-3. Profile of general demographic characteristics. [cited 2006 Jul 26]. Available from: URL: http://factfinder.census.gov/home/saff/main.html?_lang=en.
- 38.California Department of Justice. Office of the Attorney General. Criminal Justice Statistics Center. California criminal justice profile. Table 14: domestic violence related calls for assistance. 2000. [cited 2006 Jul 26]. Available from: URL: http://stats.doj.ca.gov/cjsc_stats/prof00/19/14.pdf.
- 39.California Department of Justice. Office of the Attorney General. Criminal Justice Statistics Center. California Criminal Justice Profile. Table 11: California and FBI crime index. 2000. [cited 2006 Jul 26]. Available from: URL: http://stats.doj.ca.gov/cjsc_stats/prof00/19/11.pdf.
- 40.Census Bureau (US) Census 2000 summary file 1 (SF-1). QT-P4. Race, combinations of two races, and not Hispanic or Latino. 2000. [cited 2006 Jul 26]. Available from: URL: http://factfinder.census.gov/home/saff/main.html?_lang=en.
- 41.Census Bureau (US) Census 2000 Summary File 1 (SF-1). QT-P3. Race and Hispanic or Latino. 2000. [cited 2006 Jul 26]. Available from: URL: http://factfinder.census.gov/home/saff/main.html?_lang=en.
- 42.ESRI. Redlands (CA): 1992-2000. Arcview: version 3.2a. [Google Scholar]
- 43.SAS Institute Inc. Cary (NC): SAS Institute Inc; 1999. SAS: version 8.02. [Google Scholar]
- 44.Gujarati DN. New York: McGraw-Hill; 2003. Basic econometrics; pp. 406–7. [Google Scholar]
- 45.Von Behren J, Kreutzer R, Smith D. Asthma hospitalization trends in California, 1983–1996. J Asthma. 1999;36:575–82. doi: 10.3109/02770909909087294. [DOI] [PubMed] [Google Scholar]
- 46.Cesaroni G, Farchi S, Davoli M, Forasteire F, Perucci CA. Individual and area-based indicators of socioeconomic status and childhood asthma. Eur Respir J. 2003;22:619–24. doi: 10.1183/09031936.03.00091202. [DOI] [PubMed] [Google Scholar]
- 47.Rosenthal BS, Wilson WC. The association of ecological variables and psychological distress with exposure to community violence among adolescents. Adolescence. 2003;38:459–79. [PubMed] [Google Scholar]
- 48.Rennison C. Washington:: Bureau of Justice Statistics; 2001. [cited 2006 Jul 7]. Violent victimization and race 1993-1998. Available from: URL: http://www.ojp.usdoj.gov/bjs/pub/pdf/vvr98.pdf. [Google Scholar]
- 49.Department of Justice (US). Bureau of Justice Statistics. Criminal victimization in the United States, 1998 Statistical Tables. Table 61. Selected personal and property crimes. 1998. [cited 2006 Jul 26]. Available from: URL: http://www.ojp.usdoj.gov/bjs/pub/pdf/cvus98.pdf.
- 50.Hart TC, Rennison C. Washington: Dept. of Justice, Bureau of Justice Statistics; 2003. Reporting crime to the police, 1992-2000. [Google Scholar]
- 51.Hennekens CH, Buring JE. Boston: Little, Brown; 1987. Epidemiology in medicine. [Google Scholar]
- 52.Morgenstern H. Ecologic study. In: Armitage P, Colton T, editors. Encyclopedia of biostatistics. Chichester (NY): Wiley; 1998. [Google Scholar]
- 53.Chen E, Bloomberg GR, Fisher EB, Jr, Strunk RC. Predictors of repeat hospitalizations in children with asthma: the role of psychosocial and socioenvironmental factors. Health Psychol. 2003;22:12–8. doi: 10.1037//0278-6133.22.1.12. [DOI] [PubMed] [Google Scholar]
- 54.Morris RD, Naumova EN, Goldring J, Hersch M, Munasinghe RL, Anderson H. Childhood asthma surveillance using computerized billing records: a pilot study. Public Health Rep. 1997;112:506–12. [PMC free article] [PubMed] [Google Scholar]
- 55.Census Bureau (US) 1990 net undercount and undercount rate for counties by state. [cited 2006 Jul 7]. Available from: URL: http://www.census.gov/dmd/www/undercounty.html.
- 56.Respiratory diseases disproportionately affecting minorities. NHLBI Working Group. Chest. 1995;108:1380–92. doi: 10.1378/chest.108.5.1380. [DOI] [PubMed] [Google Scholar]