SYNOPSIS
Objectives
Given the national effort to respond to the challenge of terrorism post-9/11, this study examined the organizational structure of state public health preparedness programs across the country, their administration, and the personnel and resources supported through federal cooperative agreements and state funds.
Methods
In Fall 2004, the Association of State and Territorial Health Officials surveyed state public health preparedness directors of all 50 states and territories of the United States regarding the organizational structure, administration, personnel, and resources of the state public health preparedness programs.
Results
Individuals representing 45 states and the District of Columbia responded to the web-based questionnaire for a response rate of 88.2%. States tended to subdivide their organizations into regions for preparedness purposes. More than half the established preparedness regions (53.8%) were created post-9/11. Preparedness program directors frequently reported directly to either the state health official (40.0%) or a deputy state health official (33.3%). Responsibility for both the Centers for Disease Control and Prevention (CDC) and Health Resources and Services Administration (HRSA) cooperative agreements was predominantly vested in one person (73.3%). Federal resources were found to support needed preparedness workforce (CDC mean=117.1 full-time equivalents [FTEs]; HRSA mean=10.6 FTEs). In addition, 36.6% of the states also contributed to the public health preparedness budget.
Conclusions
This study of state public health agency preparedness provides new information about state-level organizational structure, administration, and support of preparedness programs. It offers the first comprehensive insights into the approaches states have adopted to build infrastructure and develop capacity through CDC and HRSA funding streams.
The unprecedented attacks of September 11, 2001, and the subsequent anthrax-related events thrust our nation's often forgotten public health system into the forefront of public attention.1 Congress and the President took immediate action to bolster defense of the nation against the threats posed by terrorism. Steps taken included the allocation of new dedicated funding streams to support homeland security.2,3 Armed with these additional resources and the development of inventive tools, public health, as well as law enforcement, emergency management, hospitals, and others were expected to rise to the challenge of defending the United States against this emerging threat. In response to these recent challenges, public health agencies at the state and local levels have made major strides to advance their preparedness programs4 and lessen the collective potential danger to society from terrorism. Rapid engagement and enthusiastic support of preparedness programs has occurred across the nation.5
The post-9/11 literature is replete with information regarding preparedness and the pivotal role played by the public health workforce.6–14 Likewise, experienced public health practitioners have offered their thoughtful approaches for overall public health agency preparedness, particularly in conjunction with critical system partners.15–21 In addition, innovative assessment tools have been developed to assist state and local health departments in determining the community's overall level of readiness.22–24
However, even with this plethora of preparedness activities and recent published literature, relatively little is known about the organization of state public health preparedness programs around the country, their administration, and the infrastructure supporting preparedness. Moreover, the various approaches state public health preparedness programs have taken to resolve their unique needs with respect to federal funding sources have not been documented. The current study was initiated to address this information gap related to public health preparedness infrastructure at the state level.
METHODS
In the fall of 2004, the Association of State and Territorial Health Officials (ASTHO) surveyed state health departments about the status of current organizational characteristics of state-level preparedness activities under the Centers for Disease Control and Prevention (CDC) and the Health Resources and Services Administration (HRSA) cooperative agreements (CAs). The survey was designed specifically to assess emergency preparedness within state public health agencies since 9/11, and to gather information regarding their activities related to the federal CAs. The questionnaire contained 27 questions divided into four major domains of inquiry: preparedness organizational structure, program administration, program workforce and support, and exercises. Respondents were also asked to identify their organizational typology utilizing defined categories from previous studies.25,26
In November 2004, cover letters and e-mails were sent to the state public health preparedness directors of all fifty states and the District of Columbia, soliciting their participation in the study and directing them to the appropriate electronic address for participation in the survey. Surveys were also sent to the United States territories, but they were excluded from the present study. After thirty days, one of the authors personally contacted nonresponders through e-mail or telephone. State officials who did not complete the instrument were contacted no fewer than three times prior to February 2005.
To better understand trends in the data, we performed analyses utilizing numerous variables of interest. For example, we interpreted responses from a geographic perspective employing the four U.S. Census Bureau regions.27 In addition, we used a categorical measure of population size to allow comparisons between the state responses. State population size was defined as large (the eight largest states), medium (15 states), and small (22 states).27 We also examined per capita preparedness investment. This measure was obtained by dividing preparedness budget information collected from the current study by the estimated 2004 state population.27 This per capita preparedness investment was further classified as low (0–$4.67), medium ($4.68–$6.75), and high (>$6.75). Statistical analyses utilized the chi-square test, Fisher's exact test, independent sample t-tests, or Pearson's correlation as appropriate and significance was considered at the p<0.05 level. All analyses were computed in SPSS version 13.0.28 Approval for this study was obtained from the Florida State University Human Subjects Committee.
RESULTS
Individuals representing 44 states and the District of Columbia responded to the web-based questionnaire for an overall response rate of 88.2%. To facilitate the presentation of the study results, findings were divided into four subsections (depicted in Tables 1–4) corresponding to state public health preparedness organizational structure, state public health preparedness administration, state public health preparedness workforce and support, and state public health preparedness drills and exercises.
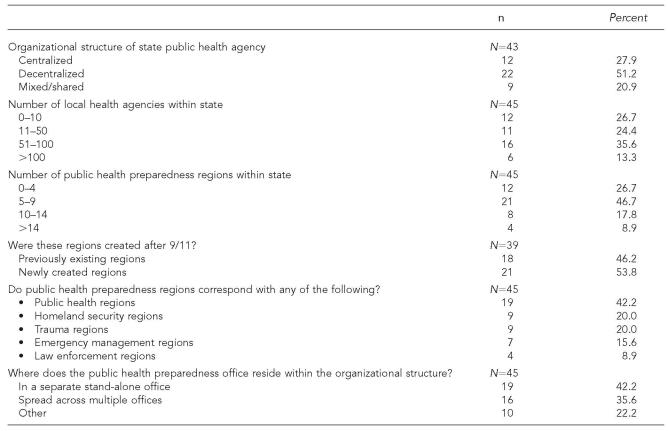
Table 1.
State public health preparedness organizational structure
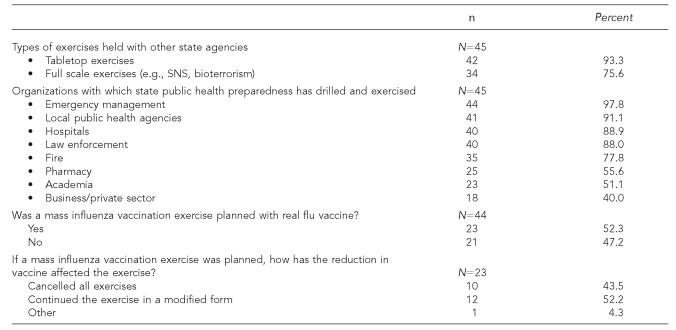
Table 4.
State public health preparedness drills and exercises
SNS = Strategic National Stockpile
State public health preparedness organizational structure
Approximately half of the responding states (51.3%) classified their public health system organizational typology as decentralized, while one-fourth (27.9%) indicated they were centralized (see Table 1). Mixed or shared organizational structure accounted for the remaining 20.9%. Although there was considerable variation nationally, in nearly half the states (48.9%) there were 51 or more local public health agencies (LPHAs). However, this pattern was counterbalanced by more than one-fourth of the states (26.7%), with 10 or fewer LPHAs.
Results suggest that states tended to further subdivide their organizations into regions for preparedness purposes. For example, roughly three-quarters of respondents (73.4%) were arrayed in nine or fewer regions, while four states had more than 14 regions. We also noted a correlation between increasing numbers of LPHAs within the state and the tendency for the state to form more public health regions (r=0.433; p=0.003). More than half the established preparedness regions (53.8%) were created post-9/11. Even with the growing number of mission critical partners, preparedness regions corresponded most frequently with state-defined public health regions (42.2%). Nonetheless, homeland security regions and trauma regions together accounted for 40.0% of the preparedness regional structures, with emergency management regions representing an additional 15.6%. Some states aligned their regions to relate with more than one category of preparedness partner, accounting for 48 responses among the 45 state respondents.
State responses were divided fairly evenly on the topic of preparedness program office structure (stand-alone office: 42.2%; spread or matrix structure: 35.6%; and other: 22.2%). States with newly created preparedness regions revealed a tendency toward stand-alone offices, while pre-existing regions were more likely to select matrix options. However, this trend was not significant (p=0.057). Further analysis showed geographic variations in organizational structure. Newly created regions were significantly more likely to have been formed in the Midwest as compared with other areas of the country (Midwest 90.0% vs. Northeast 57.1% vs. South 28.6% vs. West 50.0%; p=0.03). Moreover, these newly established regions were less likely to correspond with pre-existing public health regions than were previously existing regional structures (p=0.021). There was a greater tendency for decentralized typology states to form new preparedness regions (66.7%), but it was not statistically significant (p=0.055).
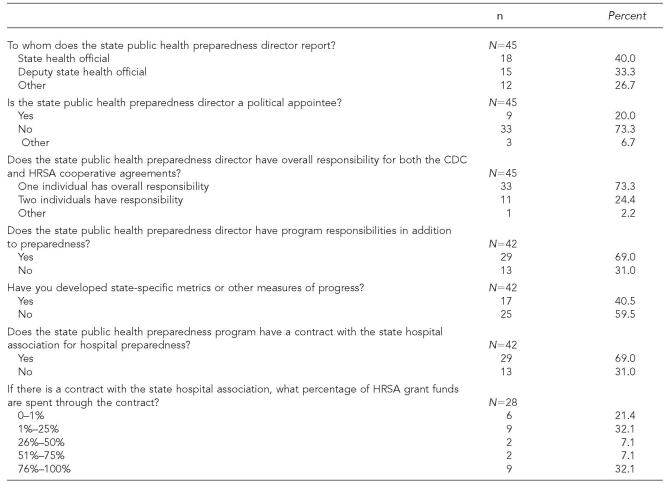
State public health preparedness administration
Analogous to the state agency structure outlined in the previous section, the survey also focused upon preparedness program administration (see Table 2). Nearly three-quarters of the preparedness program directors (73.3%) reported directly to either the state health official (40.0%) or a deputy state health official (33.3%). Most program directors (80.0%) were not political appointees, increasing their potential to make a lasting impact within the agency and state. A clear preference was expressed for vesting responsibility for both the CDC and HRSA cooperative agreements in one person (73.3%). Even with the heavy obligations incumbent under the CA, more than two-thirds of state preparedness directors (69.0%) reported having additional programmatic duties.
Table 2.
State public health preparedness administration
CDC = Centers for Disease Control and Prevention
HRSA = Health Resources and Services Administration
In addition to grant requirements detailed within the respective CDC and HRSA CAs, states have opted to self-impose further performance measures or metrics to demonstrate that important programmatic milestones have been achieved. Overall, 17 of 42 respondents (40.5%) stated that they employ additional indicators for tracking preparedness implementation.
To learn whether state hospital associations have proven to be key system partners in the implementation of the HRSA hospital preparedness grant, states were asked about their level of involvement in preparedness. Over two-thirds of state preparedness programs (69.0%) contracted with the state hospital association to facilitate preparedness.
No variation was noted for preparedness administration by geography, population size, organizational typology, or preparedness regional structure.
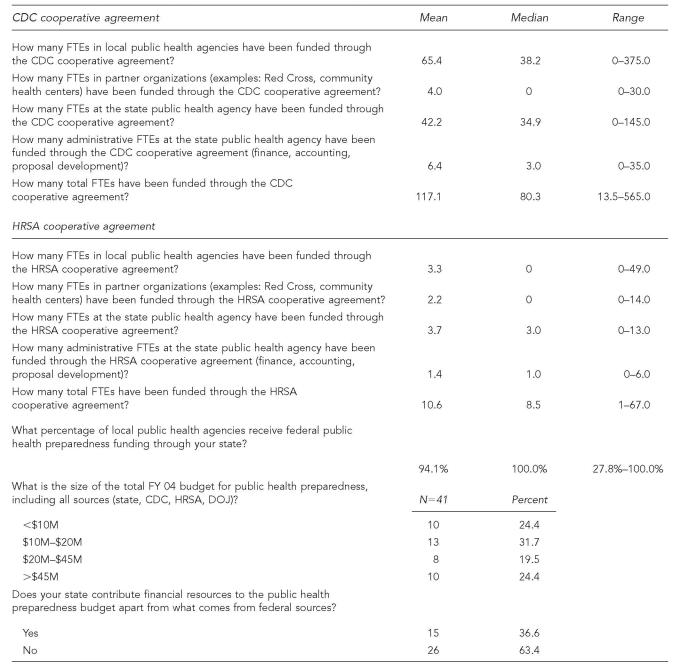
State public health preparedness workforce and support: personnel and fiscal resources
The ASTHO survey also examined how states utilized newly garnered federal resources to strengthen the public health workforce. Results are depicted in Table 3 by grant source. Overall, public health preparedness budgets from all sources for fiscal year 2004 exhibited a wide variability. For example, approximately one-quarter of state budgets were less than $10 million (24.4%) and one-quarter were more than $45 million (24.4%). Nearly one-third (31.7%) had allocated from $10 to $20 million for public health preparedness purposes. Notably, not all preparedness budgets were comprised entirely of federal dollars; 36.6% of responding states contributed to the cost associated with public health preparedness.
Table 3.
State public health preparedness workforce and support
CDC = Centers for Disease Control and Prevention
FTE = full-time equivalent
HRSA = Health Resources and Services Administration
DOJ = Department of Justice
Investments with resources from the CDC CA benefited both local and state public health capacity. On average, 65.4 full time equivalents (FTEs) were added to LPHAs (median=38.2). Overall, 94.4% of LPHAs received some funding from the CDC CA. A typical state public health preparedness program was strengthened by the support of 42 positions (median=35). States selected differing pathways with respect to building capacity within preparedness partner organizations such as the Red Cross, community health centers, and hospital associations. Many public health preparedness system partners had their workforce enhanced, with CDC resources funding a mean of four FTEs (median=0; range=0–30). In total, the CDC CA supported the preparedness workforce statewide by financing a mean of 117.1 positions (median: 80.3).
Far fewer FTEs were supported through the HRSA funding. Overall, the mean for total FTEs funded by the grant was 10.6 (median=8.5). Another difference between the HRSA and CDC CAs was that positions supported were more typically located at the state level in the HRSA grant (HRSA: 3.7 state and 3.3 local; CDC: 42.2 state and 65.4 local; all FTE means). In addition, proportionately, as a percentage of total FTEs, HRSA funding support for partner organizations such as state hospital associations was greater (HRSA 20.8% vs. CDC 3.4%; p<0.001).
States with the largest preparedness budget allocations were found to have a greater likelihood of investing more resources for building workforce capacity. For example, states with public health preparedness budgets above $45 million tended to support more total FTEs through the CDC CA as compared with all other states (>$45M vs. <$10M: p<0.001; >$45M vs. $10–20M: p<0.001; >$45M vs.$20–45M: p=0.024). Similar findings were present for LPHA investment (>$45M vs. <$10M: p<0.001; >$45M vs. $10–20M: p=0.001). However, these relationships were not demonstrated for the HRSA grant, except as pertaining to administrative FTEs (>$45M vs. <$10M: p<0.001; >$45M vs. $10–20M: p=0.003; >$45M vs. $20–45M: p=0.005).
State population size was related to personnel and fiscal resources in a manner similar to the size of the preparedness budget. States with larger populations were more likely to fund greater numbers of LPHA positions (large vs. small: p<0.001; large vs. medium: p=0.011), state public health agency positions (large vs. small: p<0.001; large vs. medium: p=0.009), total positions under the CDC CA (large vs. small: p<0.001; large vs. medium: p=0.012), and administrative FTEs under the HRSA CA (large vs. small: p<0.001; large vs. medium: p=0.004).
Similar findings were obtained with regard to per capita investment in public health preparedness. Higher per capita funding was related to greater workforce support for LPHA positions (p=0.003), total positions (p=0.003), state level program FTEs (p=0.004), as well as HRSA administrative FTEs (p=0.025) when contrasted with the lowest per capita preparedness budget. In addition, per capita investment in public health preparedness was found to be inversely related to the number of LPHAs in the state. States with fewer LPHAs (up to 10) tended to have higher per capita contributions compared with states with more LPHAs (51–100; p=0.003). No difference was noted in per capita support for newly established preparedness regions vs. those predating Sept 11. Organizational structure was also found to be associated with personnel and fiscal resources. States identifying themselves as having mixed or shared organizational control had a significantly greater likelihood of funding more LPHA positions as well as total preparedness positions though the CDC CA compared with centrally organized states (LPHA support mixed/shared vs. centralized: p=0.037; total FTEs mixed/shared vs. centralized: p=0.036). States with previously established regions, when compared with states with newly formed regions, were significantly different only with respect to CDC CA supported administrative positions. Previously established regions funded on average nine FTEs vs. three FTEs for newly created regions (p=0.015). No differences were found when analyzing workforce support and U.S. census geographic regions.
State public health preparedness and exercises
Drills and exercises may be considered the processes by which the level of preparedness attainment can be assessed. At the time of the study, nearly all states reporting having held exercises with other system partners (see Table 4). Tabletop exercises were the most frequent form of joint exercise among respondents (93.3%). Consistent with the mission of the grant, key organizational partners were emergency management (97.8%) and LPHAs (91.1%), closely followed by hospitals (88.9%) and law enforcement (88.0%). Extensive involvement of pharmacies (55.6%) reflected the importance states have assigned to exercises involving the Strategic National Stockpile. Frequent participation by the academic (51.1%) and private sectors (40.0%) indicate the broad perspective taken toward preparedness drilling and system partners.
Flu season offered the opportunity to test the responsiveness of the public health systems' ability in a live drill, and this challenge was accepted by half the states (52.3%). Inadequate vaccine availability nationally resulted in many of these critical exercises being sidelined (43.5%).
Further analyses were conducted utilizing several variables searching for trends. No differences with regard to exercises and drills were noted among respondents based upon geographic basis, population size, organizational typology, or previously existing preparedness regional structure.
DISCUSSION
The threat posed by terrorism and the need for optimal preparedness have not diminished during the intervening years since September 11, 2001.29,30 More recent events may have served to increase the risk to the U.S. of being a target of terrorism. Intense activity across the nation on the part of state and local health departments and their preparedness partners to ensure a robust response to these dangers can now be placed into a better contextual framework as a consequence of having greater insight into the state public health preparedness organizational structure, administration, and infrastructure from the current ASTHO study.
To facilitate closer coordination between public health and mission critical partners, most state public health preparedness programs have strategically moved to establish regional structures. Moreover, the need for regional approaches to improve coordinated responses when confronted by complex threats was often magnified by the large number of LPHAs participating in the response effort. Nearly half the state public health systems in the country were comprised of 51 or more LPHAs, with six states having more than 100 LPHAs. Indeed, a correlation was found between the number of LPHAs within states and the tendency to form more regions. In addition to corresponding with existing public health regions, these newly formed regions tended to align themselves with homeland security, trauma, and emergency management regions, further enhancing the potential for improved interagency communication.
State public health preparedness program administrative structures were also well designed to assure prompt access to critical agency decision-makers in an expedited fashion. Lessons learned from the anthrax events and the need for nimble responsiveness have emphasized the importance of prompt input to leadership.31 This was illustrated by three-fourths of preparedness directors reporting to either the state health official or the deputy state health official. Also of significance, the vast majority of preparedness directors had oversight for both the CDC and HRSA CAs. This approach may well have allowed for closer integration of preparedness activities across the agency and more consistent communication with external partners.
To a large extent, infrastructure and support for state and local public health translate into building organizational capacity through workforce expansion and training. The same can be said for public health preparedness programs; sustainable infrastructure is a necessary prerequisite to successful readiness. The current study confirmed that the CDC and HRSA CAs have greatly expanded statewide public health preparedness workforce and support, with virtually all LPHAs benefiting in some fashion. Conventional wisdom that larger population states and those states with more generous preparedness budgets tended to increase the number of preparedness positions the most was likewise confirmed.
The CDC CA was primarily designed to enhance the ability of state public health systems to respond to terrorism threats through infrastructure development and capacity building. National resources committed to bolstering hospital preparedness under the HRSA CA were more than half as much as the CDC grant program (2005 HRSA $476M; CDC $829M).32 However, given that strengthening hospitals' ability to respond was the intended purpose of this federal support (rather than enhancement of public health infrastructure),33,34 it is not surprising that far fewer FTEs were supported through the HRSA funding. State hospital associations proved to be pivotal partners in fulfilling the HRSA mandate, with more than two-thirds of the states working closely with them. Emphasis, however, varied substantially, with one-third of states (32.1%) committing over three-quarters of the HRSA funding through the hospital association, while half the states contributed less than 25% of the hospital preparedness resources, in a classic bimodal distribution.
One of the most notable findings of the study was that more than one-third of the states contributed to the public health preparedness budget. Given many states' slow recovery from the economic downturn of recent years,35 coupled with the nearly universal state requirement for a balanced budget, this was a substantial commitment that is likely underrecognized at the federal level.
Although the CDC and HRSA grants have focused on building needed capacity within public health and hospitals, impressively, over 40% of states have looked beyond capacity to focus on capability and performance improvements made possible through their infrastructure enhancements.36 Ultimately, improved capability and performance will be the litmus test for success of the federal funding streams.37 Further research will be needed to discern whether those states proposing more sophisticated measures conduct more robust exercises and drills, as well as whether their preparedness program implementation is better suited for addressing the problems posed by disasters and terrorism.
Our work also found that preparedness exercises are becoming increasingly more sophisticated, and now involve a growing number of agency and system partners. Many public health agencies have recognized the looming threat of an influenza pandemic, and have conducted exercises accordingly.38,39 Future research is warranted to determine the relationship between increases in preparedness capacity and overall improvement in readiness as demonstrated through performance in actual events and exercises.
Despite the important contributions we feel this study makes to the literature regarding public health preparedness, it does have limitations. First, although our survey benefited from a high response rate, not all states participated. Second, this was a self-reported survey, and therefore may be subject to recall bias. The data we present is offered from the perspective of the state preparedness director. Although they are well positioned to respond to inquiries related to public health preparedness in their states, a self-reported study, by its nature, introduces the potential for bias.
In conclusion, this study of state public health agency preparedness has provided new information about state-level organizational structure, administration, and support of preparedness programs. Moreover, it offers the first comprehensive insights into the approaches states have adopted to build infrastructure and develop capacity through CDC and HRSA funding streams. Integrating these results with the available knowledge regarding the strengthening of the public health workforce and proven strategies for promoting coordinated interagency collaboration holds great potential for improving state public health system preparedness performance, should terrorism again darken our borders.
REFERENCES
- 1.Spake A, Boyce N, Hawkins D, Schultz S, Sobel R. Confusion in spades: the anthrax scares reveal a public-health system in dissarray. US News World Rep. 2001;131:42–8. [PubMed] [Google Scholar]
- 2.Departments of Labor, Health and Human Services and Education, and Related Agencies Appropriations Act of Fiscal Year 2002. 2001. 115 Stat. 2186, 2198.
- 3.Department of Defense and Emergency Supplemental Appropriations for Recovery from and Response to Terrorist Attacks in the United States Act. 2002;Vol 115 Stat. 2230, 2314. [Google Scholar]
- 4.Terrorism preparedness in state health departments–United States, 2001-2003. MMWR Morb Mortal Wkly Rep. 2003;52(43):1051–53. [PubMed] [Google Scholar]
- 5.Estrada L, Fraser M, Cioffi J, Sesker D, Walkner L, Brand MW, et al. Partnering for preparedness: the project public health ready experience. Public Health Rep. 2005;120(Suppl 1):69–75. doi: 10.1177/00333549051200S114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gebbie K, Merrill J. Public health worker competencies for emergency response. J Public Health Manag Pract. 2002;8(3):73–81. doi: 10.1097/00124784-200205000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Miner K, Childers W, Alperin M, Cioffi J, Hunt N. The MACH Model: from competencies to instruction and performance of the public health workforce. Public Health Rep. 2005;120(Suppl 1):9–15. doi: 10.1177/00333549051200S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turnock BJ. Roadmap for public health workforce preparedness. J Public Health Manag Pract. 2003;9:471–80. doi: 10.1097/00124784-200311000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Calhoun G, Rowney R, Eng E, Hoffman Y. Competency mapping and analysis for public health preparedness training initiatives. Public Health Rep. 2005;120(Suppl 1):91–9. doi: 10.1177/00333549051200S117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Potter MA, Barron G, Cioffi JP. A model for public health workforce development using the National Public Health Performance Standards Program. J Public Health Manag Pract. 2003;9:199–207. doi: 10.1097/00124784-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Shadel BN, Chen JJ, Newkirk RW, Lawrence SJ, Clements B, Evans RG. Bioterrorism risk perceptions and educational needs of public health professionals before and after September 11, 2001: a national needs assessment survey. J Public Health Manag Pract. 2004;10:282–89. doi: 10.1097/00124784-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Kerby DS, Brand MW, Johnson DL, Ghouri FS. Self-assessment in the measurement of public health workforce preparedness for bioterrorism or other public health disasters. Public Health Rep. 2005;120:186–91. doi: 10.1177/003335490512000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kerby DS, Brand MW, Elledge BL, Johnson DL, Magas OK. Are public health workers aware of what they don't know? Biosecur Bioterror. 2005;3:31–8. doi: 10.1089/bsp.2005.3.31. [DOI] [PubMed] [Google Scholar]
- 14.Harrison LM, Davis MV, MacDonald PD, Alexander LK, Cline JS, Alexander JG, et al. Development and implementation of a public health workforce training needs assessment survey in North Carolina. Public Health Rep. 2005;120(Suppl 1):28–34. doi: 10.1177/00333549051200S107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lurie N, Wasserman J, Stoto M, Myers S, Namkung P, Fielding J, Valdez RB. Local variation in public health preparedness: lessons from California. Health Aff (Millwood) 2004. W4-341-53. [DOI] [PubMed]
- 16.Werner D, Wright K, Thomas M, Edgar M. An innovation in partnership among first responders and public health: bridging the gap. Public Health Rep. 2005;120(Suppl 1):64–8. doi: 10.1177/00333549051200S113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lurie N, Wasserman M, Stoto S, Myers R, Namkung P, Fielding J, Valdez R. Santa Monica (CA): Rand; 2004. Gaps in public health preparedness: lessons learned in California. [DOI] [PubMed] [Google Scholar]
- 18.Davis LM, Blanchard JC. Santa Monica (CA): Rand; 2002. Are local health responders ready for biological and chemical terrorism? [Google Scholar]
- 19.Gursky EA. Drafted to fight terror: U.S. public health on the front lines of biological defense. [cited 2006 Jul 24]. Available from: URL: http://www.homelandsecurity.org/bulletin/drafted_gursky.pdf.
- 20.Trust for America's health. Ready or not? Protecting the public's health in the age of bioterrorism. [cited 2006 Jul 24]. Available from: URL: http://healthyamericans.org/state/bioterror/Bioterror.pdf. [DOI] [PubMed]
- 21.Malecki J, Brumback CL. Need for physicians trained in preventive medicine and public health: implications for a bioterrorism response. J Public Health Manag Pract. 2003;9(2):89–90. doi: 10.1097/00124784-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Council of State and Territorial Epidemiologists. National assessment of epidemiologic capacity: findings and recommendations. [cited 2006 Jul 15]. Available from: URL: http://www.cste.org/Assessment/ECA/pdffiles/ECAfinal05.pdf.
- 23.Scharf L, Bradshaw C, Fidler A, Sinnock P. Atlanta: CDC; 2002. State preparedness and response capacity inventory. [Google Scholar]
- 24.Scharf L, Bradshaw C, Fidler A, Sinnock P. Atlanta: CDC; 2002. Local public health preparedness and response capacity inventory. [Google Scholar]
- 25.Beitsch L, Brooks R, Grigg M, Menachemi N. Structure and functions of state public health agencies at the dawn of the new millennium. Am J Pub Health. 2006;96:167–72. doi: 10.2105/AJPH.2004.053439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (US) Public Health Practice Program Office. Profile of state and territorial public health system, 1991. [cited 2004 Aug 17]. Available from: URL: http://wonder.cdc.gov/wonder/sci%5Fdata/misc/type%5Ftxt/stprof91.asp.
- 27. Census Bureau (US). US Census Bureau Regions 2005.
- 28.SPSS, Inc. Chicago: SPSS Inc.; 2004. SPSS: version 13.0. [Google Scholar]
- 29.Gursky E, Inglesby TV, O'Toole T. Anthrax 2001: observations on the medical and public health response. Biosecur Bioterror. 2003;1:97–110. doi: 10.1089/153871303766275763. [DOI] [PubMed] [Google Scholar]
- 30.Mann NC, MacKenzie E, Anderson C. Public health preparedness for mass-casualty events: a 2002 state-by-state assessment. Prehospital Disaster Med. 2004;19:245–55. doi: 10.1017/s1049023x00001849. [DOI] [PubMed] [Google Scholar]
- 31.Potter M, Burns H, Barron G, Grofebert A, Bednarz G. Cross-sector leadership development for preparedness. Public Health Rep. 2005;120(Suppl 1):109–15. doi: 10.1177/00333549051200S119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.FY 2005 Budget in brief. [cited 2005 Sep 19]. Available from: URL: http://www.hhs.gov/budget/05budget/centers.html.
- 33.Washington: U.S. General Accounting Office; 2004. HHS Bioterrorism Preparedness Programs: States reported progress but fell short of program goals for 2002. [Google Scholar]
- 34.Fiscal Year 2004 Continuation Guidance National Bioterrorism Preparedness Program Catalogue of Federal Domestic Assistance No 93.003. [cited 2006 Mar 3]. Available from: URL: http://www.hrsa.gov/bioterrorism/hrsa04biot.htm.
- 35.Osborne D, Hutchinson P. The price of government. [cited 2005 Sep 19]. Available from: URL: http://www.ripolicyanalysis.org/WashStateApproach.pdf.
- 36.Beitsch L. Washington: Association of State and Territorial Health Officials; 2006. Public health preparedness: how do we measure our success? [Google Scholar]
- 37.Burkle FM., Jr Measures of effectiveness in large-scale bioterrorism events. Prehospital Disaster Med. 2003;18:258–62. doi: 10.1017/s1049023x0000114x. [DOI] [PubMed] [Google Scholar]
- 38.Taylor JL, Roup BJ, Blythe D, Reed GK, Tate TA, Moore KA. Pandemic influenza preparedness in Maryland: improving readiness through a tabletop exercise. Biosecur Bioterror. 2005;3:61–69. doi: 10.1089/bsp.2005.3.61. [DOI] [PubMed] [Google Scholar]
- 39.Osterholm MT. Preparing for the next pandemic. N Engl J Med. 2005;352:1839–42. doi: 10.1056/NEJMp058068. [DOI] [PubMed] [Google Scholar]