Abstract
C57Bl/6 mice and mice deficient in the CD40 molecule were infected with three strains of Mycobacterium avium. Two of the M. avium strains proliferated more extensively in CD40-deficient (CD40−/−) mice than in control mice. The increased susceptibility to infection of CD40−/− mice was associated with the generation of poorer interleukin-12 (IL-12) p40 and interferon-γ (IFN-γ) responses as compared to the controls, suggesting a role for CD40 in the development of protective immunity. In contrast, direct triggering of CD40 on infected macrophages failed to induce any anti-mycobacterial activity in infected macrophages.
Introduction
The induction of T-cell responses requires the engagement of costimulatory molecules on antigen-presenting cells (APC) in addition to the specific recognition of the peptide–major histocompatibility complex (MHC) by the T-cell receptor. Among the costimulatory molecules, some belong to the tumour necrosis factor (TNF) and TNF-receptor (TNF-R) superfamilies. CD40, classified as member 5 of the TNF-R superfamily (TNF-RSF5), is expressed on APC and has been shown to be required for the induction of immune responses to infectious agents such as Leishmania,1–4 Toxoplasma gondii,5 Candida albicans6 and Schistosoma mansoni.7 Human patients with mutations in the gene coding for CD40 ligand exhibit the hyper-immunoglobulin M (IgM) syndrome and are prone to infections with opportunistic agents such as T. gondii, Pneumocystis carinii and Cryptosporidium.8,9
The role of CD40 during infection with mycobacteria is less clear. CD40-deficient mice have been shown to be as capable as wild-type mice in controlling Mycobacterium tuberculosis infection,10 although CD154-deficient mice are more susceptible to M. bovis bacille Calmette–Guérin (BCG).11 The clinical evidence of an effect on susceptibility to infection with mycobacteria in CD40-ligand mutations is scarce and anecdotal. Levy et al.8 studied 56 patients with X-linked hyper-IgM syndrome and reported three cases of mycobacterial pneumonia (caused by M. bovis, M. bovis BCG, or atypical mycobacteria), one central nervous system infection caused by M. bovis, and one case of disseminated M. tuberculosis infection leading to the death of the patient. In addition, Ito et al.12 reported the case of a patient with hyper-IgM syndrome who developed a severe tuberculosis infection.
Hayashi et al. have reported that agonists of the CD40 molecule are able to induce anti-M. avium activity in human monocyte-derived macrophages.13 These authors also showed that the administration of an anti-CD40 ligand monoclonal antibody (mAb) to mice reduced their ability to control infection with the same strain of M. avium. These data were, however, limited to one strain of M. avium and no detailed kinetic study of the infection was performed nor was the immune response analysed. In contrast, Larkin et al. failed to observe the induction of anti-M. tuberculosis activity in human monocytes triggered by soluble CD40 ligand.14 Thus, we sought to further dissect the role of CD40/CD154 interactions during M. avium infection using CD40−/− mice and a wider panel of mycobacterial isolates. We present evidence that CD40/CD154 interactions are required for the optimal induction of immune responses to some isolates and in their effective control.
Materials and methods
Animals and infection
Control C57Bl/6 mice (Harlan Iberica, Barcelona, Spain) and C57Bl/6Ncr-TNFRSF5−/− (CD40−/−) mice (bred in our animal facility from breeding pairs obtained from The Jackson Laboratory, Bar Harbor, ME) were intravenously infected with 106 colony-forming units (CFU) of one of three M. avium strains differing in virulence.15 Strains 2447 and 1983, with a smooth transparent (SmT) morphotype, were provided by Dr F. Portaels (Institute of Tropical Medicine, Antwerp, Belgium); strain 25291 (SmT morphotype) was obtained from the American Type Culture Collection (ATCC; Manassas, VA). All bacteria were cultured in Middlebrook 7H9 broth (Difco, Sparks, MO), collected during the exponential growth phase, resuspended in saline containing 0·05% Tween 80, and stored at −80° until used. The infection was followed-up for up to 4 months by performing viable counts on tissue homogenates of groups of five mice. Serial dilutions of these homogenates were plated onto Middlebrook 7H10 agar medium (Difco). Data shown represent the means of the log10 CFU and their standard deviations.
Analysis of the immune response
Spleen cell suspensions were prepared from aseptically collected organs at different time-points of infection, as well as from non-infected control animals. Cells were stimulated in vitro with M. avium envelope proteins (4 µg/ml),16 and interferon-γ (IFN-γ) secretion was evaluated at 72 hr of stimulation by performing an enzyme-linked immunosorbent assay (ELISA) on the supernatants, as described previously.16,17 In vivo TNF secretion was induced by the intraperitoneal injection of 50 µg of lipopolysaccharide (LPS), and the concentration of TNF in the sera was evaluated 2 hr postinduction, as described previously.18 In vivo production of interleukin-12 p40 (IL-12p40) was studied by reverse transcription–polymerase chain reaction (RT–PCR) analysis. Total RNA was extracted from a small portion of liver tissue of individual mice, after lysis in guanidinium isothiocyanate buffer. Reverse transcription was performed using a kit supplied by Invitrogen (Carlsbad, CA). The message for hypoxanthine phosphorybosyltransferase (HPRT) was amplified using specific primers. All samples were standardized for approximately the same HPRT expression level, and this level was verified to be below saturation point, by comparison with a curve generated by serial dilutions of one of the cDNAs. The same amounts of cDNA were then used to PCR amplify the IL-12p40 message, using primers with the following sequences: sense: CGTGCTCATGGCTGGTGCAAA; antisense: CTTCATCTGCAAGTTCTTGGG. The PCR products of both messages were run in an agarose gel containing ethidium bromide. The gel was photographed and the image analysed to evaluate band intensity, using imagequant software. The histological appearance of granulomas was studied in haematoxylin & eosin-stained paraffin sections of formalin-fixed samples.
Macrophage cultures
Bone marrow-derived macrophages were prepared from C57Bl/6 and CD40−/− mice, as described previously.19 Briefly, the marrows from the femurs of the mice were flushed with Hanks' balanced salt solution (HBSS; Life Technologies, Paisley, UK), washed and seeded into the wells of 24-well tissue-culture plates. Cells were cultured in Dulbecco's modified Eagle's minimal essential medium (DMEM; Life Technologies) for 10 days in the presence of 10% L-cell-conditioned medium, as a source of growth factors. Mature macrophages were then used to assess their response to anti-CD40 agonistic antibodies. Thus, macrophages (3·4 × 105 cells per well) were incubated for 72 hr in the presence of 100 U/ml of recombinant IFN-γ (Life Technologies) and/or 1–20 µg/ml of purified CD40 mAb (from hybridoma 1C10). Supernatants were analysed for the concentration of nitrite, as described previously.19 The expression of CD40 in bone marrow-derived macrophages was studied by specifically staining cells with fluorescein-labeled mAb to CD40 (BD-Pharmingen, San Diego, CA) and performing flow cytometry on stained and unstained (control) cells. Macrophages were infected with M. avium 1983 at an infection ratio of 10 : 1 (mycobacteria : macrophages) for 4 hr followed by thorough washing with warmed HBSS to remove extracellular mycobacteria. IFN-γ (100 U/ml) + TNF-α (100 U/ml) and/or anti-CD40 1C10 mAb (10 µg/ml) were then added and the proliferation of mycobacteria was studied by performing viable counts at different time-points of infection. Cytokines were added, daily for the first 4 days, at the indicated doses.
Results
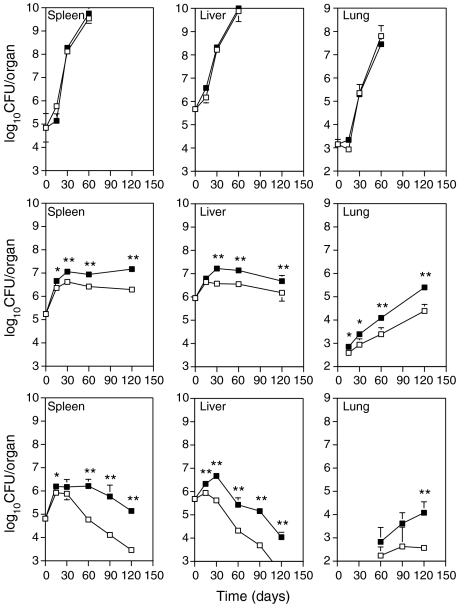
As shown in Fig. 1, strain ATCC 25291 proliferated extensively in the organs of infected mice, with no evidence of any control of the infection. No significant differences were found between wild-type and CD40−/− mice in terms of bacterial loads. In contrast, the growth of strains 2447 and 1983 was arrested following an initial period of uncontrolled proliferation and was followed, in the liver and spleen, by bacteriostasis or bacterial killing, respectively, in strains 2447 and 1983. Such control of infection was significantly delayed in the CD40−/− mice as compared to the controls. Likewise, proliferation of the mycobacterial strains in the lungs was enhanced in the CD40-deficient animals as compared to C57Bl/6 mice. Histological analysis of haematoxylin & eosin-stained sections of infected tissues did not reveal any differences in the development of granulomas in wild-type or CD40−/− mice (data not shown).
Figure 1.
Course of infection of Mycobacterim avium strains 25291 (top panels), 2447 (middle panels), and 1983 (bottom panels) in the organs of C57Bl/6 mice (open symbols) and C57Bl/6Ncr-TNFRSF5−/− (CD40−/−) mice (closed symbols). Statistically significant differences between the two strains of mice were determined using the Student's t-test and are indicated as *(P < 0·05) or **(P < 0·01).
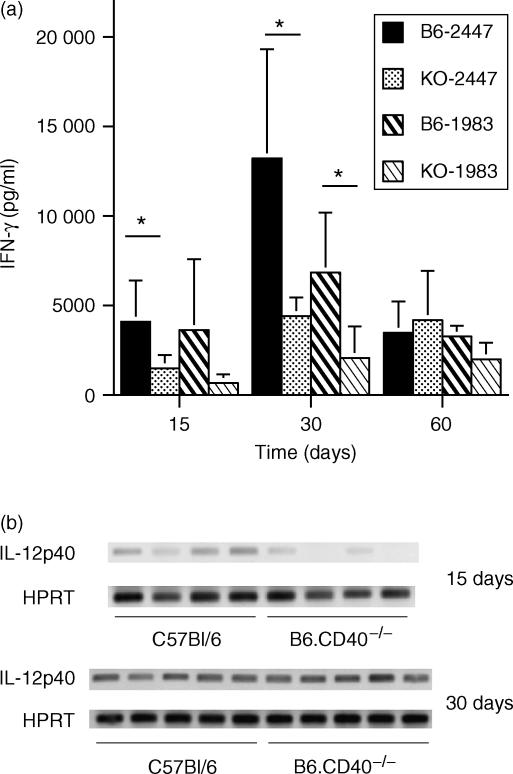
To understand the basis of the increased susceptibility of CD40-deficient animals to infection with the M. avium strains 2447 and 1983, we first analysed the immune response to infection. Spleen cells from mice infected with strains 2447 and 1983 were collected and cultured in the presence of homologous antigen prepared from the envelope proteins of these strains, and the secretion of IFN-γ was analysed in the cultures. As shown in Fig. 2(a), a significant decrease in the antigen-specific production of IFN-γ was observed at the peak of the response in CD40−/− mice, as compared to the controls, during infection with either of the two M. avium strains. Additionally, when we studied the in vivo priming of macrophages for TNF secretion by inducing TNF secretion in infected mice following a 2-hr challenge with LPS, no significant differences in the amount of TNF in the sera were found between C57Bl/6 and CD40−/− mice (143 ± 48 U/ml in the former versus 104 ± 68 U/ml in the latter). As IFN-γ production is, to a great extent, dependent on the action of IL-12, and because IL-12 production is triggered by CD40/CD154 interactions,20–23 we analysed, by RT–PCR, the expression of the p40 chain of this cytokine in infected livers. On day 15 of infection with strain 2447, no message was detected in samples from two CD40−/− mice and the other two animals had very little PCR product detectable (Fig. 2b). In contrast, the message was already abundant in C57Bl/6 mice. By day 30 of infection these differences were no longer evident, with similar, high levels of expression, in both mouse strains (Fig. 2b).
Figure 2.
(a) Secretion of interferon-γ (IFN-γ) by cultures of spleen cells from mice infected with Mycobacterium avium strain 2447 or strain 1983 upon stimulation with homologous M. avium envelope proteins (4 µg/ml). Levels of IFN-γ in non-stimulated cultures, or in stimulated cultures of spleen cells from non-infected animals, were ≈500 pg/ml. (b) Measurement, by semiquantitative reverse transcription–polymerase chain reaction (RT–PCR), of interleukin-12 p40 (IL-12p40) expression in liver samples of mice infected for 15 or 30 days with M. avium 2447. Each band represents the digital image of the amplification product for the material obtained for one mouse and for either IL-12p40 or hypoxanthine phosphorybosyltransferase (HPRT).
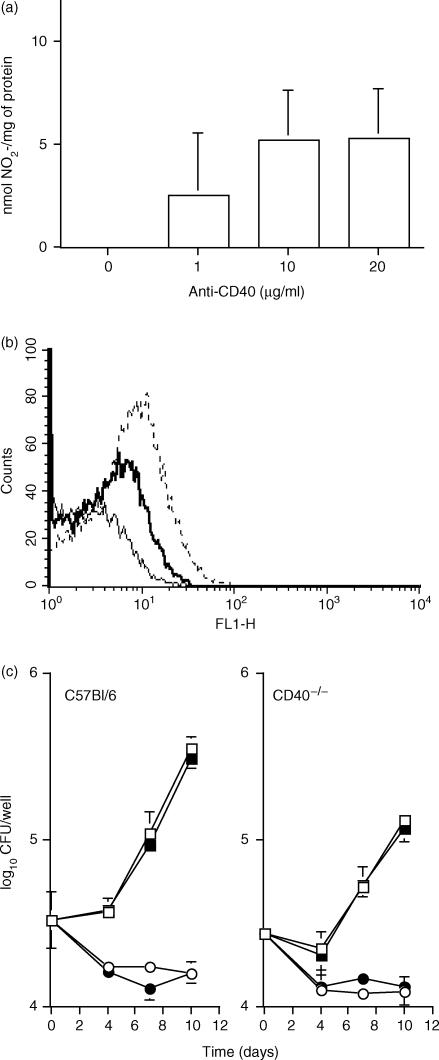
To investigate whether the engagement of CD40 at the surface of infected macrophages led to the induction of anti-mycobacterial activity, we stimulated cultured macrophages with agonistic CD40 mAbs in the presence or absence of activating cytokines. Initially, we assessed the activity of the antibody by studying its ability to trigger nitric oxide in activated macrophages. The antibody was shown to be an effective agonist in vitro by specifically stimulating reactive nitrogen species in IFN-γ-activated macrophages (Fig. 3a). No nitrite was detected in the absence of IFN-γ stimulation (data not shown). Similar data were obtained with resident peritoneal macrophages and, additionally, no response was seen when peritoneal macrophages from CD40−/− mice were used instead of those from C57Bl/6 animals (data not shown). As shown in Fig. 3(b), CD40 was present in resting macrophages and its expression was increased by activation with IFN-γ. Having shown that CD40 was both expressed in macrophages and that the 1C10 mAb was an effective agonist, we assessed whether triggering of CD40 led to the induction of mycobacterial growth inhibition. Bone marrow-derived macrophages were infected with strain 1983 and the growth of mycobacteria was studied in untreated macrophages or in macrophages treated with IFN-γ and/or anti-CD40 (Fig. 3c). Stimulation of macrophages, infected with strain 1983, with the antibody at concentrations tenfold higher than those which acted as agonists of nitric oxide synthesis (10 µg/ml), failed to reduce the mycobacterial proliferation. Increasing the concentration of the antibody a further fourfold still had no effect on mycobacteriostasis (data not shown). In parallel cultures, a combination of recombinant IFN-γ (100 U/ml) and recombinant TNF (100 U/ml), administered daily to the cultures during the first 4 days of infection, caused a marked restriction in the growth of M. avium 1983 inside macrophages. The effect of the cytokines was not affected by the addition of anti-CD40. Similar, negative results were obtained when anti-CD40 were used on macrophages infected with strain 2447 (data not shown). The proliferation of M. avium was slightly reduced in resting macrophages from CD40−/− mice as compared to those from C57Bl/6 animals. This was found in three independent experiments.
Figure 3.
(a) Secretion of nitrite by C57Bl/6 bone marrow-derived macrophages (BMMφ) activated with 100 U/ml of interferon-γ (IFN-γ), in the presence of increasing concentrations of agonist CD40 monoclonal antibodies (mAbs). (b) Expression of CD40 by non-activated (thick line) or IFN-γ-activated (broken line) BMMφ from C57Bl/6 mice, and unstained cells (thin line), as evaluated by fluorescence-activated cell sorter (FACS) analysis. (c) Effect of anti-CD40 treatment on M. avium proliferation: growth of M. avium strain 1983 was studied in BMMφ from C57Bl/6 or CD40−/− mice treated with IFN-γ plus tumour necrosis factor-α (TNF-α) (100 U/ml added daily for the first 4 days, circles) or not added (squares), in the presence (closed symbols) or absence (open symbols) of CD40 mAb (10 µg/ml).
Discussion
The present data show that CD40–CD154 interactions are necessary for the optimal induction of protective immunity to M. avium, involving the development of IFN-γ-secreting T cells. These data are consistent with previous observations on the contribution of CD154 to IFN-γ responses in human tuberculosis24,25 and, in general, with the role of CD40–CD154 interactions in the up-regulation of the T helper 1 (Th1)-promoting functions of APC.26 One possible explanation for the reduced priming of Th1 responses in CD40-deficient animals is a delayed production of IL-12p40. However, the deficiency in the IL-12 response was only transient and recovered later during infection, suggesting that other triggers for the production of this cytokine exist. These data are similar to those obtained in other models of infection where the CD40-deficient hosts showed reduced production of IL-12, impacting on the final IFN-γ responses.1,2 The importance of the interaction between CD40 and CD154 for the generation of IL-12, and the subsequent emergence of a protective immune response, has also been highlighted in human leprosy lesions.27 In contrast to the work of Hayashi et al.,13 we failed to observe a direct anti-mycobacterial triggering effect on macrophages, as previously documented for human monocytes. This may be a result of species differences, of differences in the mycobacterial strains used, or of the use of macrophages differentiated under different conditions. On the other hand, CD40 triggering was able to promote nitric oxide production and, in leishmania infections, such increased nitric oxide secretion has been shown to induce leishmanicidal activity.3 However, L. major is susceptible to nitric oxide-mediated killing by macrophages, whereas M. avium is not susceptible to the amounts of nitric oxide produced by activated macrophages.28 This suggests that protective T cells do not activate M. avium-infected macrophages to restrict mycobacterial proliferation through the use of CD154, as shown in other models.29 The mycobacterial growth appeared to be somewhat reduced in the mutant macrophages as compared to control cells, in the absence of any immunological activation. The reason of this is currently unknown, but could be related to the co-segregation of genes influencing macrophage activity present in the parent 129 strain from which the embryonic stem cells used to contruct the mutant mice are derived. Also unclear is the in vivo significance of this in vitro phenomenon. As macrophages are not expected to express the ligand for CD40, homotypic interactions triggering this molecule are unlikely to explain the data obtained.
We failed to identify any differences in the development of granulomas, in contrast to the results reported for a BCG infection model in CD154-deficient mice.11 It is probable that the levels of IFN-γ, still produced in the deficient animals, were sufficient for the organization of the granulomas, although insufficient for the early induction of mycobacteriostasis or killing. Additionally, the levels of TNF, also involved in granuloma organization, appeared not to be affected.
In summary, CD40 and CD154 should be considered accessory molecules in the induction of protective immunity to M. avium infections. Thus, our data strengthen the view that engagement of CD40 on APCs by CD154 present on the surface of T cells leads to the initiation of the immune response, resulting in the priming of protective IFN-γ-producing T cells.26 These initial steps probably involve the induction of the secretion of cytokines, such as IL-12, but could also include the participation of other costimulatory molecules that would become up-regulated on the APCs, such as members of the B7 family.26 In our system, however, redundant mechanisms surely exist which ensure that, even in the absence of CD40/CD154 signalling, the protective immune response still develops, albeit with a delayed kinetics. The nature of these additional systems is yet unclear but may include the activity of innate receptors such as the Toll-like receptors that may sense the pathogen and trigger the costimulatory pathways required for the generation of protective responses.
Acknowledgments
This work was supported by contracts POCTI/32629 from the Fundação para a Ciência e a Tecnologia (Portugal) and SDH.IC.I.01.15 from the Fundação Calouste Gulbenkian (Portugal). M.F. and A.S.G. are in receipt of postdoctoral fellowships from the ‘Fundação para a Ciência e a Tecnologia’.
References
- 1.Campbell KA, Ovendale PJ, Kennedy MK, Fanslow WC, Reed SG, Maliszewski CR. CD40 ligand is required for protective cell-mediated immunity to Leishmania major. Immunity. 1996;4:283–9. doi: 10.1016/s1074-7613(00)80436-7. [DOI] [PubMed] [Google Scholar]
- 2.Kamanaka M, Yu P, Yasui T, Yoshida K, Kawabe T, Horii T, Kishimoto T, Kikutani H. Protective role of CD40 in Leishmania major infection at two distinct phases of cell-mediated immunity. Immunity. 1996;4:275–81. doi: 10.1016/s1074-7613(00)80435-5. [DOI] [PubMed] [Google Scholar]
- 3.Nashleanas M, Scott P. Activated T cells induce macrophages to produce NO and control Leishmania major in the absence of tumor necrosis factor receptor p55. Infect Immun. 2000;68:1428–34. doi: 10.1128/iai.68.3.1428-1434.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soong L, Xu J-C, Grewal I, et al. Disruption of CD40–CD40 ligand interactions results in an enhanced susceptibility to Leishmania amazonensis infection. Immunity. 1996;4:263–73. doi: 10.1016/s1074-7613(00)80434-3. [DOI] [PubMed] [Google Scholar]
- 5.Reichmann G, Walker W, Villegas EN, Craig L, Cai G, Alexander J, Hunter CA. The CD40/CD40 ligand interaction is required for resistance to toxoplasmic encephalitis. Infect Immun. 2000;68:1312–8. doi: 10.1128/iai.68.3.1312-1318.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Netea MG, van der Meer JWM, Verschueren I, Kullberg BJ. CD40/CD40 ligand interactions in the host defense against disseminated Candida albicans infection: the role of macrophage-derived nitric oxide. Eur J Immunol. 2002;32:1455–63. doi: 10.1002/1521-4141(200205)32:5<1455::AID-IMMU1455>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 7.MacDonald AS, Patton EA, la Flamme AC, Araujo MI, Huxtable CR, Bauman B, Pearce EJ. Impaired Th2 development and increased mortality during Schistosoma mansoni infection in the absence of CD40/CD154 interaction. J Immunol. 2002;168:4643–9. doi: 10.4049/jimmunol.168.9.4643. [DOI] [PubMed] [Google Scholar]
- 8.Levy J, Espanol-Boren T, Thomas C, et al. Clinical spectrum of X-linked hyper–IgM syndrome. Pediatrics. 1997;131:47–54. doi: 10.1016/s0022-3476(97)70123-9. [DOI] [PubMed] [Google Scholar]
- 9.Subauste CS, Wessendarp M, Sorensen RU, Leiva LE. CD40–CD40 ligand interaction is central to cell-mediated immunity against Toxoplasma gondii: patients with hyper IgM syndrome have a defective type 1 immune response that can be restored by soluble CD40 ligand trimer. J Immunol. 1999;162:6690–700. [PubMed] [Google Scholar]
- 10.Campos-Neto A, Ovendale P, Bement T, Koppii TA, Fanslow WC, Rossi MA, Alderson MR. CD40 ligand is not essential for the development of cell-mediated immunity and resistance to Mycobacterium tuberculosis. J Immunol. 1998;160:2037–41. [PubMed] [Google Scholar]
- 11.Hogan LH, Markofski W, Bock A, Barger B, Morrissey JD, Sandor M. Mycobacterium bovis BCG-induced granuloma formation depends on gamma interferon and CD40 ligand, but does not require CD28. Infect Immun. 2001;69:2596–603. doi: 10.1128/IAI.69.4.2596-2603.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ito I, Ishida T, Hashimoto T, Arita M, Osawa M, Mishima M, Nonoyama S. Hyper–IgM syndrome with systemic tuberculosis. Scand J Infect Dis. 2002;34:305–7. doi: 10.1080/00365540110080151. [DOI] [PubMed] [Google Scholar]
- 13.Hayashi T, Rao SP, Meylan PR, Kornbluth RS, Catanzaro A. Role of CD40 ligand in Mycobacterium avium infection. Infect Immun. 1999;67:3558–65. doi: 10.1128/iai.67.7.3558-3565.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larkin R, Benjamin CD, Hsu Y-M, Li Q, Zukowski L, Silver RF. CD40 ligand (CD154) does not contribute to lymphocyte-mediated inhibition of virulent Mycobacterium tuberculosis within human monocytes. Infect Immun. 2002;70:4716–20. doi: 10.1128/IAI.70.8.4716-4720.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pedrosa J, Flórido M, Kunze ZM, Castro AG, Portaels F, McFadden JJ, Silva MT, Appelberg R. Characterization of the virulence of Mycobacterium avium complex isolates in mice. Clin Exp Immunol. 1994;98:210–6. doi: 10.1111/j.1365-2249.1994.tb06127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pais TF, Cunha JF, Appelberg R. Antigen specificity of the T cell response to Mycobacterium avium infection in mice. Infect Immun. 2000;68:4805–10. doi: 10.1128/iai.68.8.4805-4810.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Flórido M, Cooper AM, Appelberg R. Immunological basis of the development of necrotic lesions following Mycobacterium avium infection. Immunology. 2002;106:590–601. doi: 10.1046/j.1365-2567.2002.01459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Appelberg R, Castro AG, Pedrosa J, Silva RA, Orme IM, Minóprio P. The role of gamma interferon and tumor necrosis factor-alpha during the T cell independent and dependent phases of Mycobacterium avium infection. Infect Immun. 1994;62:3962–71. doi: 10.1128/iai.62.9.3962-3971.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Appelberg R, Orme IM, Sousa MIP, Silva MT. In vitro effects of interleukin-4 on interferon-γ-induced macrophage activation. Immunology. 1992;76:553–9. [PMC free article] [PubMed] [Google Scholar]
- 20.de Kruyff RH, Gieni RS, Umetsu DT. Antigen-driven but not lipopolysaccharide-driven IL-12 production in macrophages requires triggering of CD40. J Immunol. 1997;158:359–66. [PubMed] [Google Scholar]
- 21.Kennedy MK, Picha KS, Fanslow WC, Grabstein KH, Alderson MR, Clifford KN, Chin WA, Mohler KM. CD40/CD40 ligand interactions are required for T cell-dependent production of interleukin-12 by mouse macrophages. Eur J Immunol. 1996;26:370–8. doi: 10.1002/eji.1830260216. [DOI] [PubMed] [Google Scholar]
- 22.Shu U, Kiniwa M, Wu CY, Maliszewski C, Vezzio N, Hakimi J, Gately M, Delespesse G. Activated T cells induce interleukin-12 production by monocytes via CD40–CD40 ligand interaction. Eur J Immunol. 1995;25:1125–8. doi: 10.1002/eji.1830250442. [DOI] [PubMed] [Google Scholar]
- 23.Stüber E, Strober W, Neurath M. Blocking the CD40L–CD40 interaction in vivo specifically prevents the priming of T helper 1 cells through the inhibition of interleukin 12 secretion. J Exp Med. 1996;183:693–8. doi: 10.1084/jem.183.2.693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Samten B, Thomas EK, Gong J, Barnes PF. Depressed CD40 ligand expression contributes to reduced gamma interferon production in human tuberculosis. Infect Immun. 2000;68:3002–6. doi: 10.1128/iai.68.5.3002-3006.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Samten B, Wizel B, Shams H, et al. CD40 ligand trimer enhances the response of CD8+ T cells to Mycobacterium tuberculosis. J Immunol. 2003;170:3180–6. doi: 10.4049/jimmunol.170.6.3180. [DOI] [PubMed] [Google Scholar]
- 26.Grewal IS, Flavell RA. CD40 and CD154 in cell-mediated immunity. Annu Rev Immunol. 1998;16:111–35. doi: 10.1146/annurev.immunol.16.1.111. [DOI] [PubMed] [Google Scholar]
- 27.Yamauchi PS, Bleharski JR, Uyemura K, et al. A role for CD40–CD40 ligand interactions in the generation of type 1 cytokine responses in human leprosy. J Immunol. 2000;165:1506–12. doi: 10.4049/jimmunol.165.3.1506. [DOI] [PubMed] [Google Scholar]
- 28.Gomes MS, Flórido M, Pais TF, Appelberg R. Improved clearance of Mycobacterium avium upon disruption of the iNOS gene. J Immunol. 1999;162:6734–9. [PubMed] [Google Scholar]
- 29.Stout RD, Suttles J, Xu J, Grewal IS, Flavell RA. Impaired T cell-mediated macrophage activation in CD40 ligand-deficient mice. J Immunol. 1996;156:8–11. [PubMed] [Google Scholar]