Abstract
Specialized microfold (M) cells of the follicle-associated epithelium (FAE) of the mucosal-associated lymphoid tissue (MALT) in gut and the respiratory system play an important role in the genesis of both mucosal and systemic immune responses by delivering antigenic substrate to the underlying lymphoid tissue where immune responses start. Although it has been shown that dendritic cells (DC) also have the ability to sample antigens directly from the gut lumen, M cells certainly remain the most important antigen-sampling cell to be investigated in order to devise novel methods to improve mucosal delivery of biologically active compounds. Recently, novel information on the interactions between bacteria and FAE have come to light that unveil further the complex cross-talk taking place at mucosal interfaces between bacteria, epithelial cells and the immune system and which are central to the formation and function of M cells. In particular, it has been shown that M cell mediated transport of antigen across the FAE is improved rapidly by exposure to certain bacteria, thus opening the way to identify new means to achieve a more effective mucosal delivery. Here, these novel findings and their potential in mucosal immunity are analysed and discussed, and new approaches to improve antigen delivery to the mucosal immune system are also proposed.
Keywords: antigen delivery, M cells, mucosal-associated lymphoid tissue (MALT), mucosal immunity
Introduction
The epithelia overlying the mucosal surfaces of the respiratory and gastrointestinal tract are exposed throughout their life to a limitless variety of antigens; their main task is to provide an efficient barrier against pathogens and macromolecules.1,2 This is achieved by several means. First, the epithelium consists of columnar cells joined by tight junctions that allow passage of water and ions but provide a mechanical barrier to macromolecules. Secondly, mucosal surfaces are covered by local secretions of mucus, secretory IgA antibodies and by a thick glycocalx.3–6 The latter represents a highly degradative environment due to the presence of membrane-bound and layer-entrapped hydrolytic enzymes.7 These features, along with the closely packed carpet of microvilli on absorptive cells, prevent contact and binding of macromolecules and potential pathogens to the epithelium. However, the mucosal epithelium also has to provide channels through which antigens and microorganisms are delivered to the intestinal immune system in order to induce immune responses. Indeed, antigenic penetration of epithelial barriers is the first step required to mount effective mucosal and systemic immune responses and M cells play a key role in this by regulating access of microorganisms and antigens to areas of the MALT equipped to generate protective responses.8,9 The importance of finding the best way to induce robust mucosal responses is highlighted by the accepted view that the systemic immune system is not adequate to fight the vast majority of pathogens to which we are continuously exposed. It is believed that over 95% of human pathogenic microorganisms target host cells after crossing epithelial barriers and in many cases the main protective effector function against these mucosal infections is the production of pathogen-specific local secretory IgA antibody response that can be achieved solely via activation of the mucosal immune system.10 This notion, along with the fact that in adult individuals the area of mucosal surfaces reaches the impressive size of 400 m,2,11 makes it imperative that we acquire a better understanding of the mechanism involved in transepithelial transport of antigens in order to design new strategies to improve oral delivery of vaccines and therapeutics.
Although villous-M cells located outside the follicle-associated epithelium (FAE) have been observed recently,12 the transport of antigens and microorganisms across the intestinal mucosa is carried out mainly by the FAE13,14 that overlies the gut associated lymphoid tissue (GALT)15(Fig. 1). A number of features distinguish the FAE from the absorptive epithelium. There are no receptors for polymeric immunoglobulin, which suggests that these epithelia do not secrete IgA.16,17 Few mucus-producing, defensin- and lysosyme-producing cells are seen in the follicle-associated crypts18 and the production of membrane-associated digestive hydrolases is reduced significantly.19 However, the most remarkable feature of the FAE is the presence of highly specialized antigen-sampling membranous or microfold (M) cells.20 M cells are not restricted to the gut but are also present within the upper respiratory tract, and particular attention is being given to M cells located within the nasal-associated lymphoid tissue (NALT).21 The importance of the NALT as a delivery route of great potential to induce strong mucosal immune responses is becoming increasingly evident and various groups have attempted to produce appropriate vaccine preparations to target specifically the local M cell population.22,23
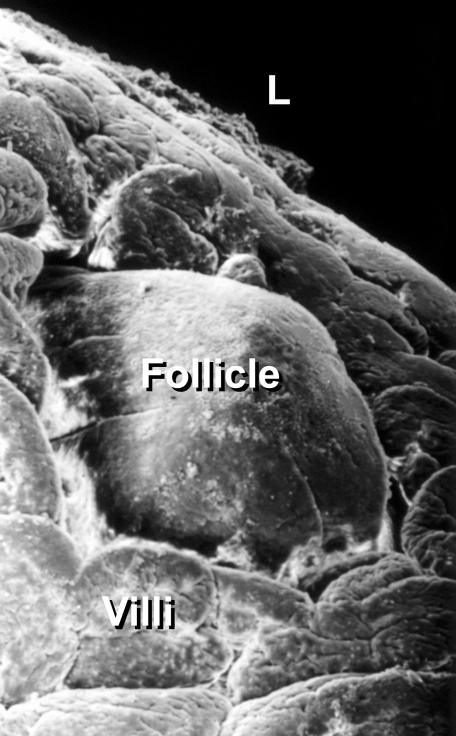
Figure 1.
Scanning electron micrograph of an individual follicle of a mouse Peyer's patch. The follicle is embedded among villi and strategically protrudes into the gut lumen (L) to sample antigens via M cells or dendritic cells.
M cell mediated transport across mucosal barriers
Sampling the gut: M cell versus dendritic cell
It has been shown recently that also dendritic cells (DC) sample epithelial cell antigens24 and bacteria25 from the gut lumen (Fig. 2). DC in the gut are located beneath the FAE of the Peyer's patch26,27 and all along the whole intestinal epithelium within the lamina propria.28In vitro experiments have shown that DC can open the tight junctions between intestinal epithelial cells and send their cellular processes into the lumen where they directly internalize bacteria.25 The expression of tight junction proteins, such as Claudin-1, Occludin and Zonula Occludens-1, enables DC to maintain the integrity of the epithelial barrier while sending their dendrites into the gut lumen. This mechanism has been demonstrated clearly in vitro, although at this time its real relevance in vivo remains to be determined fully. Indeed, in vivo evidence that DC extend their cellular processes between epithelial cells, take-up bacteria and then migrate back within the tissue to present antigens to naive T cells is currently lacking. Experiments carried out in vivo25 using isolated intestinal loops showed an increase in the number of DC recruited in the intestinal tissue briefly after the application of the bacterial stimulus, and subsequently DC dendrites can be seen protruding into the gut lumen between epithelial cells. However, recent in vivo experiments have raised questions indirectly as to the true role of DC as antigen samplers in the gut.29 The authors showed that in mice the transport across the gut barrier of orally delivered green-fluorescence protein (GFP)-labelled Enterobacter cloacae takes place exclusively via FAE-associated M cells in the Peyer's patches and they concluded that the internalization by DC occurred only following M cell mediated transport. In this regard, the discovery of villous-M cells may provide an alternative explanation for the occasional uptake of bacteria in areas of the gut located outside Peyer's patch.12 These data, taken together, suggest strongly that M cells are a major player in the sampling of the gut contents, and as such an appealing target for mucosal delivery of bioactive compounds.30,31
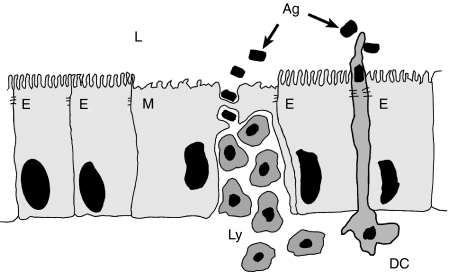
Figure 2.
Sampling the gut. M cells internalize luminal antigens and microorganisms (Ag) and deliver them to the underlying lymphoid tissue. The first contact between immune cells (Ly) and antigen can take place within M cell cytoplasmic pockets that represent a docking site for a variety of lymphocyte subsets. In addition, dendritic cells (DC) also sample antigens directly by extending their dendrites between epithelial cells (E), process them and finally present them to naive T cells in the context of MHC class II molecules.
Features of M cells
M cells display different morphological features compared with the surrounding enterocytes (Fig. 3). The brush border is poorly organized with short irregular microvilli, and the thick glycocalx associated with absorptive cells is absent.32,33 These adaptations allow easy access of luminal material to the apical domain of M cells, where it is internalized and then transported to the underlying lymphoid tissue. The mechanisms by which M cells take up microorganisms and macromolecules vary according to the nature of this material. Large particles and bacteria induce phagocytosis, which is often associated with ruffling of the apical plasma membrane of the M cell and rearrangement of the actin cytoskeleton, which permits active formation of pseudopodia-like structures.34,35 Viruses and other adherent particles are taken up by endocytosis via clathrin-coated vesicles,36 whereas non-adherent material is internalized by fluid phase endocytosis.37,38 In all these cases, internalization is followed quickly by transport of endocytotic vesicles to the endosomal compartment and then by exocytosis to the basolateral membrane. The biochemical events involved in the intracellular transport of endocytotic vesicles in M cells are still largely unknown, but it appears that this is regulated in the same manner as polarized transport observed in other epithelial cells.39,40 A characteristic of M cells is that, unlike other intestinal epithelial cells, they possess deeply invaginated basolateral surfaces that form intraepithelial pockets harbouring a wide variety of lymphocyte subsets that migrate to this unique compartment from lymphoid tissue.41,42 Thus, M cell pockets facilitate the contact between the incoming antigens and the specialized immune system in an environment separated from regulatory elements of the mucosal immune system.42 The use of a large panel of lectins to stain FAE cells has revealed that in some cases M cells display a different glycosylation state compared with neighbouring enterocytes. In mice, for example, small intestine Peyer's patch M cells predominantly express (1–2)-fucose that can be detected by Uleus europeaus (UEA-1) lectin.43,44 The pattern is different in caecal patches, where M cells are stained by the same lectin but also express other terminal saccharides.45,46 In humans, the glycosylation pattern is different from that of other species and M cells preferentially display the sialyl Lewis A antigen.47 Surface glycoconjugates play an important role in microbial–M cell interactions and the wide variability of these molecules on the M cell surface has been interpreted as an effective way to generate a broad repertoire of M cell surface binding molecules to recognize bacteria-borne lectins.48 The presence of M cell-specific glycoconjugates on M cell surface has an immediate relevance in terms of vaccine targeting. Indeed, M cell-specific glycoconjugates have been used with some success as targets for oral and nasal delivery of antigens and particulate carrier.49,50
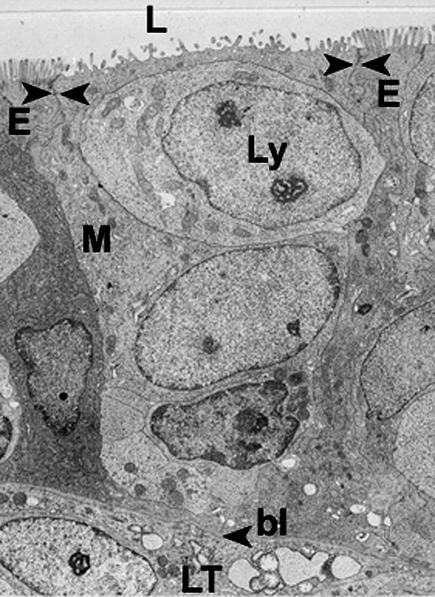
Figure 3.
Electron micrograph showing an M cell (M) enclosed between two adjacent enterocytes (E) in the FAE. The apical region is characterized by the presence of more irregular and scattered microvilli compared to those of enterocytes. This adaptation allows easy access to the M cell apical surface of material in the gut lumen (L). Lymphocytes (Ly) move into M cell pockets from the underlying lymphoid tissue (LT) through openings in the basal lamina (bl). Arrowheads indicate tight junctions.
An important aspect of M cell biology that has been overlooked is its potential in participating in the genesis of mucosal immune responses. Interestingly, although the role of M cells in processing and presenting antigens has not been investigated thoroughly, it was reported that M cells are provided with enzymatic components, including cathepsin E typical of antigen-presenting cells.51 Furthermore, although the presence of major histocompatibilty complex (MHC) Class II molecules remains controversial it, was reported by some authors that M cells expressed Ia molecules on the basolateral plasma membrane and organelles, such as prelysosome, lysosome and endosome and the expression of which was enhanced by pretreatment with interferon (IFN)-γ.52 The notion that M cells are not only simple conduits for antigen transport and may have a more active role in the early phase of mucosal immune responses is also suggested by their ability to produce immunoregulatory cytokines, such as interleukin (IL)-1.53
M cells and bacteria
The capacity of M cells for antigen sampling can also facilitate invasion by potentially harmful intestinal pathogens, a process mediated by bacterial invasin.54 The most dramatic examples of specific targeting of pathogens to M cells are provided by studies performed on Salmonella,55,56Shigella57 and Yersinia.58 In most of these cases the infection of M cells results in the disruption of the cells and the ensuing alteration of the integrity of the epithelial barrier. However, more recent studies have revealed that penetration of M cells by bacteria does not always end in catastrophe for the M cells and gut barrier. We observed that short-term exposure to a non-intestinal bacterium, Streptococcus pneumoniae R36a, induced rapid and significant changes of the morphology35 and function59,60 of the FAE. The most notable was an apparent increase in the number of fully operational M cells that led to an up-regulation of microsphere transport across the FAE59(Fig. 4) and to the systemic circulation.60 More recently the ability of S. pneumoniae to up-regulate rapidly M cell mediated transport of microparticles has been confirmed by others.61 In this case, the authors reported that the up-regulation of antigen transport was not accompanied by a real increase in the number of M cells but rather by the acquisition, by predetermined M cells already inhabiting the FAE of both morphological and functional features of fully mature and differentiated M cells. Furthermore, it is worth highlighting the fact that both groups observed that these events were not accompanied by any detectable alteration of the integrity of the epithelial barrier. These data demonstrate that this experimental model is an excellent tool to address basic but still unsolved issues of M cell biology and function. First, it will help to shed light on the still controversial issue of origin of this cell type within the FAE. Secondly, and more important from an immunological point of view, it provides the first experimental evidence that M cell mediated antigen transport to the mucosal immune system can be improved in vivo; a finding that has a direct bearing on mucosal delivery of vaccines and therapeutics.
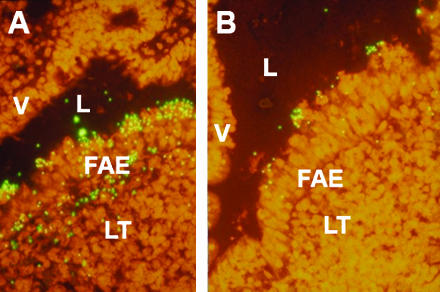
Figure 4.
Confocal laser scanning micrograph of the FAE of Peyer's patch. A significant increase in the number of microparticles bound, internalized and translocated across the FAE is observed following short-term exposure to S. pneumoniae (a) compared to control tissue (b). The binding and translocation is highly specific for the FAE as microparticles can not be seen in contact with or internalized by villous epithelial cells (V) (L = gut lumen).
M cell formation and function
The issue of M cell origin within the FAE provides a fascinating puzzle for not only cell biologists; indeed, due to their high efficiency in sampling the gut lumen this is an enticing objective for scientists seeking to design more effective methods of mucosal immunization and drug delivery. As such, the dynamics of M cell formation within specialized gut epithelia has been the subject of debate since their discovery in 1974.20 Intestinal epithelial cell maturation and differentiation is a well-known phenomenon which is completed in a topographically well-organized migration.62–64 The epithelium of each follicle derives from surrounding crypts, each of each is a clonal unit65,66 characterized by two distinct axes of migration and differentiation. Cells located on the villous side of the crypt differentiate into absorptive enterocytes, goblet and enteroendocrine cells. Cells on the FAE side of the crypt move onto the dome, acquiring features of absorptive enterocytes and specialized M cells.13 The final differentiation of intestinal epithelial cells occurs as they migrate in vertical bands to the apical extrusion zone of the villous and FAE. Within this scenario two different theories on M cell genesis in the FAE have been formulated. First, it was postulated that M cells may originate in the crypts as a distinct cell lineage from stem cells via an independent differentiation programme; alternatively, it was thought that they may be formed by the conversion of FAE–enterocytes upon interaction with the local lymphoid microenvironment.
The most convincing experimental evidence supporting the idea that M cells are derived from undifferentiated crypt cells comes from studies on differential expression of both glycoconjugates67,68 and the specific M cell marker, vimentin in rabbit.69,70 These studies showed that a subpopulation of crypt cells is predetermined as M cells before attaining their morphological and functional features. This was supported further by additional study that showed that the random distribution of the sites where lymphocytes invade the FAE did not correlate with the organization of M cells in radial strips that emerged from the dome associated crypts. These studies led the authors to conclude that M cell formation is restricted to the crypts and that FAE associated enterocytes do not have the potential to convert into M cells.
On the other hand, in addition to previous ultrastructural studies that concluded that M cells derived from fully differentiated enterocytes,71 an in vitro coculture system was established in which murine Peyer's patch-derived lymphocytes converted human intestinal Caco2 cells into functional M cells.72 Although it is a little unrealistic to consider these adenocarcinoma cells as mature and fully differentiated enterocytes,73,74 this model provides direct evidence that lympho-epithelial cross-talk plays a central role in controlling the genesis of specialized epithelial cell populations. The role of immune cells in the formation of specialized FAE and M cells was also demonstrated in several experimental models. In one such case75 it was reported that knock-out (KO) mice that lacked B cells did show a reduction in the numbers of PP and negligible numbers of M cell, thus suggesting that B cells play a role in M cell formation. Although the exclusive role of B cells in these events was later questioned,76 the ability of lymphocytes to modulate the expression of genes linked to M cell phenotype has been demonstrated clearly.77,78 In addition, in vivo studies have shown that bone marrow transplantation in SCID syngeneic mice induced the formation of M cells, thus further supporting the notion that M cell genesis is immunoregulated.79 The most compelling evidence for the ability of immune cells to convert enterocytes into M cells has come from in vivo studies that involved the use of bacteria in the gut. First, oral administration of Salmonella in mice induced a rapid increase (12 hr) in the number of both IEL and M cells within the FAE80 and secondly, that short-term exposures (1–3 hr) to a non-intestinal bacterium, S. pneumoniae R36a induced dramatic alterations of the FAE that included an apparent increase in the number of fully operational M cells in the periphery of the FAE.60 Finally, it also appears that that the numbers of the newly discovered villous-associated M cells population increased following in vivo challenge with S. typhimurium.12 In the light of recent findings, however,61 it seems that these apparently conflicting results on M cell genesis within the FAE can now be reconciled. Indeed, this work produced evidence that suggested strongly that the rapid increase in the number of fully operational M cells following certain stimuli such as Salmonella or S. pneumoniae can be explained as short-term differentiation of predetermined M cells already inhabiting the FAE rather than from the conversion of enterocytes into M cells. Although the nature of the stimulus required to induce the differentiation of predetermined M cells into fully operational ones remains unknown, hypotheses include the release of bacterial products and bacteria-induced secretion of cytokines by the host. The presence of cells with the ability to become fully functional antigen-sampling cells very rapidly would explain the changes of cell population in the FAE following bacterial challenge and, more importantly, it confirms that the antigen-sampling capability of the FAE can be manipulated in vivo. With this in mind it is possible to hypothesize that certain bacteria may help us to design novel strategies for oral delivery of vaccines and drugs.
Future scenarios in mucosal delivery
Searching for the Trojan horse for mucosal delivery
One of the major problems in devising strategies to improve M cell mediated delivery of vaccines and therapeutics to the MALT has been represented so far by the lack of knowledge on the molecular and cellular events underlying M cell formation. This complicates further the quest to identify both bacterial and host molecules involved in the bacteria-induced up-regulation of antigen sampling in the gut.
The observations described in the previous section raise a fundamental question. Can we exploit the ability of certain bacteria to design novel and more effective strategies to improve M cell-mediated transport into the MALT? Although the mechanisms underlying the previously described events are still unknown, we can argue reasonably that this will be possible. Indeed, several observations carried out in vitro point to the fact that soluble mediators might be involved. Although it is possible that bacterial products may play an important role in the final differentiation of pre-M cells into competent sampling M cells, it seems likely that factors secreted by the host gut epithelium or immune system are involved. First, it was observed that in vitro conversion of Caco2 cells into M cells by lymphocytes was not restricted to cells in contact with PP-lymphocytes or B cell lymphoma Raji.72 This was confirmed further in a coculture system in which Caco2 cells and Raji cells were separated physically during culture.81 These experimental models did not employ bacteria, thus implying that soluble mediators secreted by B cells had a major role in the M cell conversion. Given the nature of the lymphoma Raji B cells it is conceivable that these cells constitutively secrete a lympho/cytokine which is normally secreted in vivo upon interaction with bacteria by either epithelial or, more probably, immune cells. This prospect opens a fascinating scenario. The advantage of having at our disposal a molecule with the ability to up-regulate mucosal antigen uptake is obvious, and novel methods to improve both oral (via GALT) and nasal (via NALT) delivery of vaccines and drugs might be within our grasp. Such a molecule will probably help to reduce or minimize the dose and consequently the cost of vaccine or drug preparation, and in addition it may improve the efficiency of already existing or experimental antigen delivery system. For instance, recombinant bacteria have been employed successfully as living delivery vectors for heterologous antigens.82,83 The knowledge that some bacteria have an intrinsic ability to up-regulate M cell mediated transport across mucosal barriers may have a great impact in the selection of the bacterial vector. Alternatively, if the enhancer of M cell transport was a cytokine the construction of a more effective bacterial vector would be possible. The vector should have the ability to target specifically M cells (i.e. Salmonella) and coexpress a heterologous antigen along with the enhancer of mucosal uptake, thus allowing the latter to exert its biological activity within the FAE. In addition, the efficiency of other available technologies such as biodegradable microparticles84,85 may also be improved as the enhancer of mucosal antigen uptake could be microencapsulated easily along with the desired vaccine or drug preparation.
Concluding remarks
As regulator of antigen transport across epithelial barriers in the GALT and NALT, M cells play an important role in the genesis of protective immune responses. The importance of finding better ways to induce effective immune responses at the mucosal level is stressed by the notion that the systemic immune response is not well equipped to tackle the vast majority of pathogens to which we are exposed throughout life. In addition, mucosal administration of bioactive compounds can be administrated easily with none of the risks associated usually with parenteral administration, and their easier and cheaper manufacture may increase their availability to developing countries. In light of these considerations, it is highly desirable to have a better understanding of the cellular and molecular events underlying M cell formation and function in specialized mucosal epithelia. The recent discovery that the M cell mediated transport across mucosal barriers can be significantly up-regulated by interaction with bacteria without altering their integrity gives us a real opportunity to design novel strategies, or to improve already existing ones to achieve more effective oral and nasal delivery of biologically active compounds.
Acknowledgments
We wish to thank I. T. Johnson and M. T. Garcia-Conesa for their suggestions and critics; E. Bertelli, M. Regoli and H. M. Meynell for transmission, scanning and confocal microscopy and P. Pople for his help in computer work. Work in our laboratory is sponsored by research grants from the Biotechnology and Biological Sciences Research Council, UK.
References
- 1.Madara JL, Nash S, Moore R, Atisook K. Structure and function of the intestinal epithelial barrier in health and disease. Monogr Pathol. 1990;31:306–24. [PubMed] [Google Scholar]
- 2.Bjarnason I, MacPherson Hollander D. Intestinal permeability. Gastroenterology. 1995;108:1566–81. doi: 10.1016/0016-5085(95)90708-4. [DOI] [PubMed] [Google Scholar]
- 3.McGhee JR, Kiyono H. New perspective in vaccine development: mucosal immunity to infections. Infect Agents Dis. 1993;2:55–73. [PubMed] [Google Scholar]
- 4.Frey A, Giannasca KT, Weltzin R, et al. Role of glycocalix in regulating access to plasma membranes of intestinal epithelial cell: implications for microbial attachment and oral vaccine targeting. J Exp Med. 1996;1996:1045–59. doi: 10.1084/jem.184.3.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kett K, Baklien K, Bakken A, Kral JG, Fausa O, Brandtzaeg P. Intestinal B cell isotype response in relation to local bacteria load: evidence for IgA subclass adaptation. Gastroenterology. 1995;109:819–25. doi: 10.1016/0016-5085(95)90389-5. [DOI] [PubMed] [Google Scholar]
- 6.Maury J, Nicoletti C, Guzzo-Chambraud F, Maroux S. The filamentous brush border glycocalix, a mucine-like marker of enterocytes hyper polarization. Eur J Biochem. 1995;228:323–31. [PubMed] [Google Scholar]
- 7.Semenza G. Anchoring and biosynthesis of stalked brush border membrane proteins: glycosidases and peptidases of enterocytes and renal tubuli. Annu Rev Cell Biol. 1990;2:255–313. doi: 10.1146/annurev.cb.02.110186.001351. [DOI] [PubMed] [Google Scholar]
- 8.Neutra MR, Frey A, Kraehenbuhl JP, Epithelial M. cells. Gateways for mucosal infection and immunization. Cell. 1996;86:345–8. doi: 10.1016/s0092-8674(00)80106-3. [DOI] [PubMed] [Google Scholar]
- 9.Neutra MR, Pringault E, Kraehenbuhl JP. Antigen sampling across epithelial barriers and induction of mucosal immune responses. Annu Rev Immunol. 1996;14:275–300. doi: 10.1146/annurev.immunol.14.1.275. [DOI] [PubMed] [Google Scholar]
- 10.Holmgren J, Czerkinsky C, Eriksson K, Mharandi A. Mucosal immunization and adjuvants: a brief overview of recent advances and challenges. Vaccine. 2003;21(Suppl. 2):89–95. doi: 10.1016/s0264-410x(03)00206-8. [DOI] [PubMed] [Google Scholar]
- 11.Brandtzaeg P, Baekkevold ES, Farstad IN, et al. Regional specialization in the mucosal immune system: what happens in the microcompartments? Immunol Today. 1999;20:141–51. doi: 10.1016/s0167-5699(98)01413-3. [DOI] [PubMed] [Google Scholar]
- 12.Jang MH, Kweon MN, Iwatani K, et al. Intestinal villous M cells: an antigen entry site in the mucosal epithelium. Proc Nat Acad Sci USA. 2004;101:6110–5. doi: 10.1073/pnas.0400969101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Neutra MR, Mantis NJ, Kraehenbuhl JP. Collaboration of epithelial cells with organized mucosal lymphoid tissues. Nature Immunol. 2001;2:1004–9. doi: 10.1038/ni1101-1004. [DOI] [PubMed] [Google Scholar]
- 14.Allan CH, Trier JS. Structure and permeability differ in subepithelial villus and Peyer's patches follicles capillaries. Gastroenterology. 1991;100:1172–9. [PubMed] [Google Scholar]
- 15.Hein WR. Organization of mucosal lymphoid tissue. Curr Top Microbiol Immunol. 1999;236:1–15. doi: 10.1007/978-3-642-59951-4_1. [DOI] [PubMed] [Google Scholar]
- 16.Pappo J, Owen RL. Absence of secretory component expression by epithelial cells overlying rabbit gut-associated lymphoid tissue. Gastroenterology. 1988;95:1173–7. doi: 10.1016/0016-5085(88)90347-2. [DOI] [PubMed] [Google Scholar]
- 17.Gehrke I, Pabst R. The epithelium overlying rabbit bronchus-associated lymphoid tissue does not express the secretory component of immunoglobulin. Cell Tissue Res. 1990;259:397–9. doi: 10.1007/BF00318464. [DOI] [PubMed] [Google Scholar]
- 18.Giannnasca PJ, Giannasca KT, Falk P, Gordon JI, Neutra MR. Regional differences in glycoconjugates of intestinal M cells in mice: potential targets for mucosal vaccines. Am J Physiol. 1994;227:1108–21. doi: 10.1152/ajpgi.1994.267.6.G1108. [DOI] [PubMed] [Google Scholar]
- 19.Owen RL, Bhalla DK. Cytochemical analysis of alkaline phosphatase and esterase activities and of lectin-binding and anionic sites in rat and mouse Peyer's patch M cells. Am J Anal. 1983;168:199–212. doi: 10.1002/aja.1001680207. [DOI] [PubMed] [Google Scholar]
- 20.Owen RL, Jones AL. Epithelial cell specialization within human Peyer's patch: an ultrastructural study of intestinal lymphoid follicle. Gastroenterology. 1974;66:189–203. [PubMed] [Google Scholar]
- 21.Fujimura Y. Evidence of M cells as portals of entry for antigens in the nasopharyngeal lymphoid tissue of humans. Virchows Arch. 2000;436:560–6. doi: 10.1007/s004289900177. [DOI] [PubMed] [Google Scholar]
- 22.Zuercher AW, Coffin SE, Thurnheer MC, Fundova P, Cebra JJ. Nasal-associated lymphoid tissue is a mucosal inductive site for virus-specific humoral and cellular immune responses. J Immunol. 2002;168:1796–803. doi: 10.4049/jimmunol.168.4.1796. [DOI] [PubMed] [Google Scholar]
- 23.Hou Y, Hu WG, Hirano T, Gu XX. A new intra-NALT route elicits mucosal and systemic immunity against Moraxella catarrhalis in a mouse challenge model. Vaccine. 2002;20:2375–81. doi: 10.1016/s0264-410x(02)00097-x. [DOI] [PubMed] [Google Scholar]
- 24.Huang FP, Platt N, Wykes M, et al. A discrete subpopulation of dentritic cells transports apoptotic intestinal epithelial cells to T cell areas of mesenteric lymph nodes. J Exp Med. 2000;191:435–43. doi: 10.1084/jem.191.3.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rescigno M, Urbano M, Valzasina B, et al. Dentritic cells express tight junction proteins and penetrate gut epithelial monolayers to sample bacteria. Nat Immunol. 2001;2:361–8. doi: 10.1038/86373. [DOI] [PubMed] [Google Scholar]
- 26.Ruedl C, Hubele S. Maturation of Peyer's patches dentritic cells in vitro upon stimulation via cytokines or CD40 triggering. Eur J Immunol. 1997;27:1325–30. doi: 10.1002/eji.1830270605. [DOI] [PubMed] [Google Scholar]
- 27.Kelsall BL, Strober W. Distinct populations of dentritic cells are present in subepithelial dome and T cell regions of the murine Peyer's patch. J Exp Med. 1996;183:237–47. doi: 10.1084/jem.183.1.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iwasaki A, Kelsall BL. Localization of distinct Peyer's patch dentritic cell subsets and their recruitment by chemokines macrophage inflammatory protein (MIP)-3α, MIP-3β, and secondary lymphoid organ chemokine. J Exp Med. 2000;191:1381–94. doi: 10.1084/jem.191.8.1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macpherson AJ, Uhr T. Induction of protective IgA by intestinal dentritic cells carrying commensal bacteria. Science. 2004;303:1662–5. doi: 10.1126/science.1091334. [DOI] [PubMed] [Google Scholar]
- 30.Wang X, Hone DM, Haddad A, Shata MT, Pascual DW. M cell DNA vaccination for CTL immunity to HIV. J Immunol. 2003;171:4717–25. doi: 10.4049/jimmunol.171.9.4717. [DOI] [PubMed] [Google Scholar]
- 31.Clark MA, Jepson MA, Hirst BH. Exploiting M cells for drug and vaccine delivery. Adv Drug Del Rev. 2001;50:81–106. doi: 10.1016/s0169-409x(01)00149-1. [DOI] [PubMed] [Google Scholar]
- 32.Bockman DE. Functional histology of appendix. Arch Histol Cytol. 1983;46:271–92. doi: 10.1679/aohc.46.271. [DOI] [PubMed] [Google Scholar]
- 33.Bye WA, Allan CH, Trier JS. Structure, organization and distribution of M cells in Peyer's patches. Gastroenterology. 1984;86:789–801. [PubMed] [Google Scholar]
- 34.Fujimura Y. Functional morphology of microfold cells (M) in Peyer's patches. Phagocytosis and transport of BCG by M cells into rabbit Peyer's patches. Gastroenterol Jpn. 1986;21:325–30. [PubMed] [Google Scholar]
- 35.Borghesi C, Bertelli E, Regoli M, Nicoletti C. Modifications of the FAE by short term exposure to a non-intestinal bacterium. J Pathol. 1996;180:326–32. doi: 10.1002/(SICI)1096-9896(199611)180:3<326::AID-PATH656>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 36.Neutra MR, Phillips TL, Mayer EL, Fishkind DJ. Transport of membrane-bound macromolecules by M cells in the FAE of rabbit Peyer's patches. Cell Tissue Res. 1987;247:536–46. doi: 10.1007/BF00215747. [DOI] [PubMed] [Google Scholar]
- 37.Owen RL. Sequential uptake of horseradish peroxidase by lymphoid follicle epithelium of Peyer's patches in normal unobstructed mouse intestine: an ultrastructural study. Gastroenterology. 1977;72:440–51. [PubMed] [Google Scholar]
- 38.Gebert A. The role of M cells in the protection of mucosal membrane. Histochem Cell Biol. 1997;108:455–70. doi: 10.1007/s004180050186. [DOI] [PubMed] [Google Scholar]
- 39.Druben DG, Nelson WJ. Origin of cells polarity. Cell. 1996;84:335–44. doi: 10.1016/s0092-8674(00)81278-7. [DOI] [PubMed] [Google Scholar]
- 40.Wolf JL, Bye WA. The membranous (M) epithelial cells and the mucosal immune system. Annu Rev Med. 1984;35:95–112. doi: 10.1146/annurev.me.35.020184.000523. [DOI] [PubMed] [Google Scholar]
- 41.Regoli M, Bertelli E, Borghesi C, Nicoleti C. Three (3D)-reconstruction of M cells in rabbit Peyer's patches: definition of intraepithelial compartment of the follicle-associated epithelium. Anat Rec. 1995;243:19–26. doi: 10.1002/ar.1092430104. [DOI] [PubMed] [Google Scholar]
- 42.Neutra MR. Current concepts in mucosal immunity. V. Role of M cells in transepithelial transport of antigens and pathogens to the intestinal immune system. Am J Physiol. 1998;274:G785–91. doi: 10.1152/ajpgi.1998.274.5.G785. [DOI] [PubMed] [Google Scholar]
- 43.Clark MA, Jepson MA, Simmons NL, Booth TA, Hirst BH. Differential expression of lectin binding sites defines mouse intestinal M cells. J Histochem Cytochem. 1993;41:1679–87. doi: 10.1177/41.11.7691933. [DOI] [PubMed] [Google Scholar]
- 44.Falk P, Roth KA, Gordon JI. Lecins are sensitive tools for defining the differentiation programs of epithelial cell lineages in the developing and adult mouse gastrointestinal tract. Am J Physiol. 1994;266:G987–G1003. doi: 10.1152/ajpgi.1994.266.6.G987. [DOI] [PubMed] [Google Scholar]
- 45.Gebert A, Hach G. Differential binding of lectins to M cells and enterocytes in the rabbit caecum. Gastroenterology. 1993;105:1350–61. doi: 10.1016/0016-5085(93)90139-4. [DOI] [PubMed] [Google Scholar]
- 46.Clark MA, Jepson MA, Simmons NL, Hirst BH. Differential surface characteristics of M cells from mouse intestinal Peyer's patch and caecal patches. Histochem J. 1994;26:271–80. [PubMed] [Google Scholar]
- 47.Giannasca PJ, Giannasca KT, Leichtner AM, Neutra MR. Human intestinal M cells display the sialyl Lewis A antigen. Infect Immun. 1999;67:946–53. doi: 10.1128/iai.67.2.946-953.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Neutra MR, Giannasca PJ, Giannasca KT. M cells and microbial pathogens. In: Blaser M, Smith PD, Ravodin JI, editors. Infections of the GI Tract. New York: Raven Press; 1995. pp. 163–78. [Google Scholar]
- 49.Clark MA, Blair H, Liang L, Brey RN, Brayden D, Hirst BH. Targeting polymerised liposomoe vaccine carriers to intestinal M cells. Vaccine. 2002;20:208–17. doi: 10.1016/s0264-410x(01)00258-4. [DOI] [PubMed] [Google Scholar]
- 50.Jepson MA, Clark MA, Hirst BH. M cell targeting by lectins: a strategy from mucosal vaccination and drug delivery. Adv Drug Del Rev. 2004;56:511–25. doi: 10.1016/j.addr.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 51.Finzi G, Cornaggia M, Capella C, et al. Cathepsin E in follicle-associated epithelium of intestine and tonsils: localization to M cells and possible role in antigen processing. Histochemistry. 1993;99:201–11. doi: 10.1007/BF00269138. [DOI] [PubMed] [Google Scholar]
- 52.Allan CH, Mendrick DL, Trier JS. Rat intestinal M cells contain acidic endosomal–lysosomal compartments and express class II major histocompatibility complex determinants. Gastroenterology. 1993;104:698–08. doi: 10.1016/0016-5085(93)91004-2. [DOI] [PubMed] [Google Scholar]
- 53.Pappo J, Mahlman RT. Follicle epithelial M cells are a source of IL-1 in Peyer's patches. Immunology. 1993;78:505–7. [PMC free article] [PubMed] [Google Scholar]
- 54.Granucci F, Ricciardi–Castagnoli P. Interactions of bacterial pathogens with dentritic cells during invasion of mucosal surfaces. Curr Options Microbiol. 2003;6:72–6. doi: 10.1016/s1369-5274(03)00007-9. [DOI] [PubMed] [Google Scholar]
- 55.Kohobata S, Yokobata H, Yabuuchi E. Cytopathogenic effect of Salmonella typhi GIFU 10 007 on cells of murine ileal Peyer's patches in ligated ileal loops: an ultrastructural study. Microbiol Immunol. 1986;30:1225–37. doi: 10.1111/j.1348-0421.1986.tb03055.x. [DOI] [PubMed] [Google Scholar]
- 56.Jones BD, Ghori N, Falkow S. Salmonella typhimurium initiates murine infection by penetrating and destroying the specialized epithelial M cells of the Peyer's patches. J Exp Med. 1994;180:15–23. doi: 10.1084/jem.180.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Perdomo JL, Cavaillon JM, Huerre M, Ohayon H, Gounon P, Sansonetti PJ. Acute inflammation causes epithelial invasion and mucosal destruction in experimental shigellosis. J Exp Med. 1994;180:1307–19. doi: 10.1084/jem.180.4.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grutzkau A, Hanski C, Hahn H, Riecken EO. Involvement of M cells in the bacterial invation of Peyer's patch: a common mechanism shared by Yersinia enterocolitica and other enteroinvasive bacteria. Gut. 1990;3:1011–5. doi: 10.1136/gut.31.9.1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Meynell HM, Thomas NW, James PS, Holland J, Taussig MJ, Nicoletti C. Up-regulation of microsphere transport across the follicle-associated epithelium of Peyer's patch by exposure to S. pneumoniae R36a. FASEB J. 1999;13:611–9. doi: 10.1096/fasebj.13.6.611. [DOI] [PubMed] [Google Scholar]
- 60.Borghesi C, Taussig MJ, Nicoletti C. Rapid appearance of M cells after microbial challenge is restricted at the periphery of the follicle-associated epithelium of Peyer's patch. Lab Invest. 1999;79:1391–01. [PubMed] [Google Scholar]
- 61.Gebert A, Steinmetz I, Fassbender S, Wendlandt KH. Antigen transport in Peyer's patches: increased uptake by constant numbers of M cells. Am J Pathol. 2004;64:65–72. doi: 10.1016/S0002-9440(10)63097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hermiston M, Green RP, Gordon JI. Chimeric-transgenic mice represent a powerful tool for studying how the proliferation and differentiation programs of intestinal epithelial cells lineages are regulated. Proc Natl Acad Sci USA. 1993;90:8866–70. doi: 10.1073/pnas.90.19.8866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Heath JP. Epithelial cell migration in the intestine. Cell Biol Int. 1996;20:139–40. doi: 10.1006/cbir.1996.0018. [DOI] [PubMed] [Google Scholar]
- 64.Louvard D, Kedinger M, Hauri HP. The differentiating intestinal epithelial cells: establishment and maintenance of functions thought interactions between cellular structures. Annu Rev Cell Biol. 1992;8:157–95. doi: 10.1146/annurev.cb.08.110192.001105. [DOI] [PubMed] [Google Scholar]
- 65.Ponder BA, Schmidt GH, Wilkinson MM, Wood MJ, Monk M, Reid A. Derivation of mouse intestinal crypts from single progenitor cells. Nature. 1985;313:689–91. doi: 10.1038/313689a0. [DOI] [PubMed] [Google Scholar]
- 66.Rubin DC, Ong D, Gordon JI. Cellular differentiation in the emerging fetal rat small intestinal epithelium: mosaic pattern of gene expression. Proc Natl Acad Sci USA. 1989;86:1278–82. doi: 10.1073/pnas.86.4.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Giannasca PJ, Giannasca KT, Falk P, Gordon JI, Neutra MR. Regional differences in glycoconjugates of intestinal M cells in mice: potential targets for mucosal vaccine. Am J Physiol. 1994;267:G1108–21. doi: 10.1152/ajpgi.1994.267.6.G1108. [DOI] [PubMed] [Google Scholar]
- 68.Gebert A, Posselt W. Glyconjugate expression defines the origin and differentiation pathway of intestinal M cells. J Histochem Cytochem. 1997;45:1341–50. doi: 10.1177/002215549704501003. [DOI] [PubMed] [Google Scholar]
- 69.Lelouard H, Sahuquet A, Reggio H, Montcourrier P. Rabbit M cells and dome enterocytes are distinct cell lineages. J Cell Sci. 2001;114:2077–83. doi: 10.1242/jcs.114.11.2077. [DOI] [PubMed] [Google Scholar]
- 70.Gebert A, Fassbender S, Werner K, Weissferdt A. The development of M cells in Peyer's patches is restricted to specialized dome-associated crypts. Am J Pathol. 1999;154:1573–82. doi: 10.1016/S0002-9440(10)65410-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Smith MW, Peacock MA. Lymphocyte induced formation of antigen transporting M cells from fully differentiated mouse enterocytes. In: Robinson JWL, editor. Mechanisms of Intestinal Adaptation. Lancaster: MTP; 1982. pp. 573–83. [Google Scholar]
- 72.Kerneis S, Bogdanova A, Kraehenbulh JP, Pringault E. Conversion by Peyer's patch lymphocytes of human enterocytes into M cells that transport bacteria. Science. 1997;277:949–52. doi: 10.1126/science.277.5328.949. [DOI] [PubMed] [Google Scholar]
- 73.Delie F, Rubas W. A human colonic cell line sharing similarities with enterocytes as a model to examine oral absorption: advantages and limitations of the caco-2 model. Crit Rev Ther Drug Carrier Syst. 1997;14:221–86. [PubMed] [Google Scholar]
- 74.Owen RL. Mid-life crisis for M cells. Gut. 1998;42:11–2. doi: 10.1136/gut.42.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Golovkina TV, Shlomchik M, Hannum L, Chervonsky A. Organogenic role of B lymphocytes in mucosal immunity. Science. 1999;286:1965–8. doi: 10.1126/science.286.5446.1965. [DOI] [PubMed] [Google Scholar]
- 76.Debard N, Sierro F, Browning J, Kraehenbuhl JP. Effect of mature lymphocytes and lymphotoxin on the development of the follicle-associated epithelium and M cells in the Peyer's patches. Gastroenterology. 2001;120:1173–82. doi: 10.1053/gast.2001.22476. [DOI] [PubMed] [Google Scholar]
- 77.El Bahi S, Caliot E, Bens M, et al. Lymphoepithelial interations trigger specific regulation of gene expression in the M cell-containing follicle-associated epithelium of Peyer's patches. J Immunol. 2002;168:3713–20. doi: 10.4049/jimmunol.168.8.3713. [DOI] [PubMed] [Google Scholar]
- 78.Lo D, Tynan W, Dickerson J, et al. Cell culture modeling of specialized tissue: identification of genes expressed specifically by follicle-associated epithelium of Peyer's patch by expression profiling of Caco-2/Raji co-cultures. Int Immunol. 2004;16:91–9. doi: 10.1093/intimm/dxh011. [DOI] [PubMed] [Google Scholar]
- 79.Sharma R, Schumacher U, Adam E. Lectin histochemistry revealed the appearance of M cell in Peyer's patches of SCID mice after syngeneic normal bone marrow transplantation. J Histochem Cytochem. 1998;46:143–8. doi: 10.1177/002215549804600202. [DOI] [PubMed] [Google Scholar]
- 80.Savidge TC, Smith MW, James PS, Aldred P. Salmonella-induced M-cell formation in germ-free mouse peyer's patch tissue. Am J Pathol. 1991;139:177–84. [PMC free article] [PubMed] [Google Scholar]
- 81.Gullberg E, Leonard M, Karlsson J, et al. Expression of specific markers and particle transport in a new human intestinal M-cell model. Biochem Biophys Res Commun. 2000;279:808–13. doi: 10.1006/bbrc.2000.4038. [DOI] [PubMed] [Google Scholar]
- 82.Robinson K, Chamberlain LM, Lopez MC, et al. Mucosal and cellular immune responses elicited by recombinant Lactococcus lactis strains expressing tetanus tocxin fragment C. Infect Immun. 2004;72:2753–61. doi: 10.1128/IAI.72.5.2753-2761.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bowe F, Pickard DJ, Anderson RJ, Londono-Arcila P, Dougan G. Development of attenuated Salmonella starins that express heterologous antigens. Meth Mol Med. 2003;87:83–100. doi: 10.1385/1-59259-399-2:83. [DOI] [PubMed] [Google Scholar]
- 84.Mathiowitz E, Jacob JS, Jong YS, et al. Biologically erodable microspheres as potential oral drug delivery systems. Nature. 1997;386:410–4. doi: 10.1038/386410a0. [DOI] [PubMed] [Google Scholar]
- 85.Brayden DJ. Oral vaccination in man using antigens in particles: current status. Eur J Pharm Sci. 2001;14:183–9. doi: 10.1016/s0928-0987(01)00175-0. [DOI] [PubMed] [Google Scholar]