Abstract
Nutrition intervention is an integral part of type 2 diabetes care. Dietary management entails a series of eating behavior changes regarding meal planning, food selection, food preparation, dinning out, portion control, as well as appropriate responses to eating challenges. Diabetic patients encounter several difficulties in complying with the dietary regime. They exhibit restrictive eating behaviors, they express feelings of dietary deprivation, and rigid dietary control is perceived as the only way to a proper diet and weight management. However, pressure to conform to nutritional recommendations may render diabetics more prone to dietary under-reporting. Binge eating, restraint and body dissatisfaction frequently occur among these patients. Health professionals, therefore, need to take into account these difficulties in their collaboration with the patients in order to improve the effectiveness of nutrition intervention.
Keywords: eating behavior, nutrition, dietary management, adherence, weight control, glycemic control
Introduction
The prevalence of type 2 diabetes mellitus is increasing worldwide [1]. Nutritional intervention is an integral part of diabetes management and self-care education, aiming at the attainment and maintenance of optimal metabolic outcomes, the prevention and treatment of medical complications, and the improvement of general health by addressing individual nutritional needs [2]. Diabetic people are routinely advised to adopt a healthful diet; dietary changes include modifications in food habits and meal patterns on a lifelong basis. However, a significant proportion of patients remain poorly controlled [3-7]. Diet, a lifestyle behavior, has been reported as a management domain with very low compliance among diabetics [8-10]. Results from cross-sectional studies indicate low adherence to the dietary recommendations for macronutrient intake and fruit and vegetable consumption [9, 11-13]. Furthermore, compared to non-diabetics, diabetic patients were less devoted to the Mediterranean diet, which is rich in vegetables, fruits, fish, cereals and olive oil [14]. There is also some evidence indicating that they are less successful in maintaining long-term weight loss than people without diabetes [15], a parameter that predisposes them to poorer metabolic control. On the other hand, Gauthier-Chelle et al. support the hypothesis that, even if their diets are far from the official recommendations, self-declared diabetic patients try to modify their dietary habits [16]. It could be that their efforts are not in the appropriate directions or that they receive confusing and contradictory advice from a variety of sources (health professionals, media, social contacts). In this case, diabetes education requires the standardized training of health professionals and a provision of unequivocal information. Yet is this enough to improve the eating habits of diabetics or should we also take more parameters into account that affect food consumption?
The overall act of eating not only includes nutrient and food intake, but also eating behavior in relation to preference, selection and consumption of food. As Anderson and Funnell interestingly pointed out, unlike the treatment of acute illnesses, the most important choices affecting the health and well-being of people with diabetes are made by themselves, and not by their physician or any other health professional [17]. Every day they need to make a series of choices with regards to eating and physical activity that are very important in regulating their blood glucose levels and overall health. An understanding of their eating behavior, as well as of the factors affecting dietary choices and underlying experiences, would help to increase the effectiveness of lifestyle education by identifying weaknesses in dietary practices and targeting specific areas for improvement. It may also help to diminish the frequently mentioned gap between knowledge of appropriate nutrition in type 2 diabetes and its application in everyday life.
What determines the eating behaviors of type 2 diabetic patients?
Little of human food choice and intake on a daily basis is directly determined by the chemical composition of foods and the physiological characteristics of the individual; it is very much influenced by events occurring around and between these factors, perceptions, beliefs and responses to cues. There are global rules that operate on human eating behavior; food choice and intake reflect food availability, existing eating habits but also learning mechanisms, and individual beliefs and expectations, i.e. cognitive influences and meanings [18]. Context largely influences food intake and diet content; it would, thus, be interesting to identify eating behaviors related to food choice in diabetic patients or to glycemic control and explore their importance and contribution. Still, data in this area are very scarce.
Savoca and Miller identified personal dimensions, behavioral patterns and environmental characteristics affecting the food consumption and eating patterns of people with type 2 diabetes [19]. Eating history, including food selection, weight control efforts, emotional eating and overeating, along with nutrition-related knowledge, influence daily diabetes management with regards to meal planning, food selection and preparation, but also behavioral responses to diet challenges, such as eating favorite foods, weight management, portion control and dinning out. Mediating variables that impede or facilitate self-dietary care of diabetes may include the level of social support, the degree of self-efficacy and the individual's time management skills.
Eating behaviors were also evaluated in relation to glycemic control [20]. A healthful eating lifestyle resulted in low HbA1c levels and was positively related to specific food habits, i.e. limiting the amount of high-sugar foods and portion sizes, eating only an occasional dessert, reducing high-fat foods, eating low-fat foods, eating regularly, planning meals, eating large amounts of vegetables, limiting specific carbohydrate. In contrast, it was negatively related to eating at buffets, fast-food and large-chain restaurants, choosing high-fat menu selections and eating high-fat sources of protein. Deviations in prescribed eating patterns, particularly breakfast skipping and snack additions and deletions, were also associated with poor metabolic control [21].
The adoption of new food habits is not an easily achieved goal. Diabetic patients encounter several educational, environmental, psychological and lifestyle difficulties in modifying their lives to accommodate disease management [22]. Barriers to dietary adherence include complications with daily life (eating out, social events) and temptations, need for food planning, need for constant self-care, denial of the severity of the disease, poor understanding of diet-disease associations, misinformation, lack of appropriate social support and time constraints (Figure 1) [23-26]. Patients also encounter troubles following food exchange systems and express their need for revised dietary strategies that would incorporate appropriate education on how to make healthy food choices [26].
Figure 1. Possible outcomes of dietary management regimes.
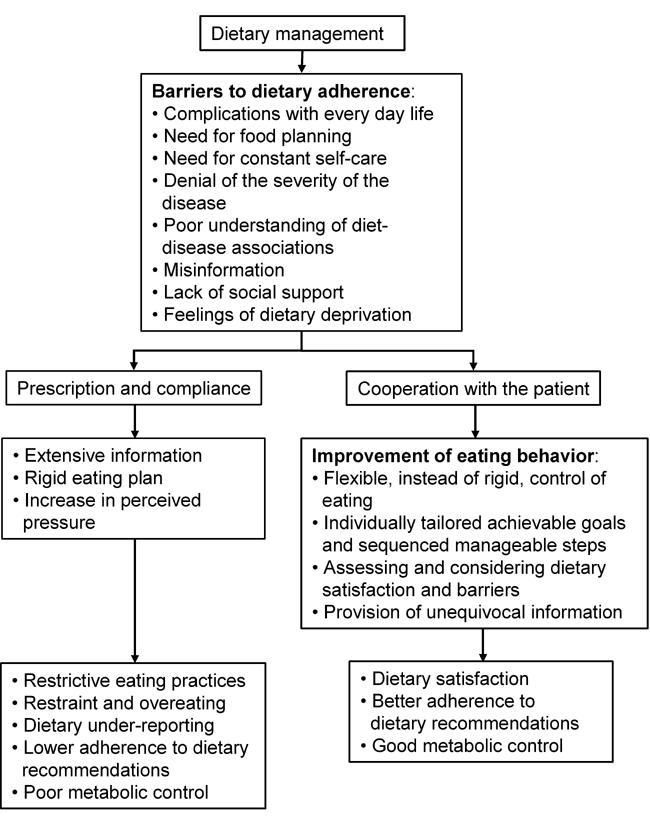
Patients face several barriers opposing a successful introduction of a nutrition-related management of diabetes. They tend towards under-reporting and low adherence to nutritional recommendations as a re-action on these barriers if diet regimes are too rigid and inflexible. A cooperation-based approach may be able to induce desirable changes in eating behavior and, with it, to metabolic control.
Moreover, diabetic patients report difficulties in complying with the dietary regime due to several associated meanings and negative emotions, such as the loss of pleasure in eating, autonomy and freedom [27]. Food ingestion is frequently accompanied by feelings of fear, guilt and anger, whereas diet compliance elicits aversive and restrictive attitudes. Thoughts of dietary deprivation have also been reported [25, 28]. Patients perceive dietary recommendations as restraining and not adapted to individual needs. Interestingly, the more "restrictive" or rigid eating practices, such as eliminating sugar, limiting carbohydrate-containing foods and decreasing total dietary fat, were far more frequently described by diabetics as an important part of diabetes dietary management compared with the more flexible eating patterns of portion control and regular eating [19]. No research so far has addressed the issue as to whether patients themselves selectively "prefer" restrictive eating practices, or whether in fact it is the health professionals who fail to promote a flexible control of eating habits, particularly during the first stages of dietary management. However, a rigid control of eating behavior contributes to a higher susceptibility to eating problems, while flexible control may be a less vulnerable method of weight management [29]. One could further hypothesize that the latter may also promote a more long-term glycemic control in diabetic patients (Figure 1). These aspects of eating behavior related to disordered eating symptoms are also discussed below.
Under-reporting as a consequence of poor dietary adherence and eating behavior
Evaluating a patient's food intake is a labor-intensive and time-consuming task, which may also be compromised and biased by the presence of under-reporting. Relevant literature reveals a variable degree of under-reporting in total energy and individual food and nutrient intakes, ranging from 10% to 88%, depending on the population studied and the method used [30]. It can be explained by under-recording (omission of recording some of the food consumed) and/or under-eating (reduction of food intake during the study period). Whatever its origin, dietary under-reporting prevails among women, older persons, and overweight individuals; there is much inconsistency regarding the effect of several other socioeconomic, demographic, lifestyle and behavioural parameters [31].
Interestingly, high under-reporting rates have been found among patients with type 2 diabetes [32, 33]. In particular, Samuel-Hodge et al. concluded that, because diabetic under-reporters actually reported diets closely matching the currently recommended diet for diabetes, it seems plausible that they were more likely to report what they should be eating rather than what they were eating [33]. Diabetic patients usually receive extensive information on food; they become more familiar with portion sizes and try to monitor their dietary intake in order to achieve glycemic control. In spite of an apparently increased awareness about their dietary intake, the opposite is observed in practice. One could hypothesize that the perceived pressure to change eating patterns and adopt a healthy diet may prompt them to intentionally omit reporting some food or food groups that do not conform to the nutrition recommendations (Figure 1). In support of this theory we found that diabetic patients are also more likely than healthy ones to under-report their obesity status [34]. Individuals encountering health problems where increased body weight is a significant risk factor may tend to under-record their BMI as a defensive mechanism. Pressure to lose weight and lack of appropriate medical guidance to do so could result in an indifference to, or concealment of, the weight problem.
Disordered eating behavior of type 2 diabetic patients
Numerous studies have found an increased prevalence of eating disorders and eating disorder symptoms in type 1 diabetic patients [35-38]; however, few reports exist regarding type 2 diabetic patients. Most of them have focused on binge eating disorder (BED), due to its association with obesity, a condition that predisposes to type 2 diabetes. The results of these studies indicate that, in general, the prevalence of BED in diabetic patients is higher than in the general community but similar to, or even lower than, in weight control samples, ranging from 2.5% to 25.6% [39-43]. The diversity in prevalence rates found in different studies may be attributed to the variety of assessment methods and the diagnostic criteria used, as well as to differences in prevalence rates across countries. Higher rates, though, are observed for binge eating, if one moves from the typical BED to a subclinical condition or an eating disorder symptom [40, 41].
Is binge eating related to the development of type 2 diabetes or is it diabetes that predisposes patients to develop binge eating symptomatology? Despite the fact that the studies having addressed this issue were cross-sectional in their design, most findings support the idea that the likely sequence is that of binge eating increasing body weight and, hence, becoming a risk factor for the development of type 2 diabetes [40, 41, 43]. The typical age of diabetes onset is much higher than that of eating disorders; therefore, it is unlikely that diabetes constitutes a risk factor for eating disorders; the opposite is more probable. Nonetheless, binge eating is not simply a covariate of overweight. Kenardy et al. found that both bingeing and obesity contribute conjointly to diabetes onset and represent independent risk factors [41]. Weight and dieting history may also affect the age of diagnosis of type 2 diabetes in susceptible individuals [44].
Little evidence holds for an association between bingeing and diabetic control, as this was assessed in most studies by HbA1c levels. After accounting for the recognized risk factors of weight, exercise, alcohol consumption and smoking, bingeing was only moderately [41] or not associated with glycemic control [39, 43, 45]. This finding may be unexpected and contradictory to similar studies in insulin-dependent diabetic patients, where the relationship between clinically disordered eating and worsened glycemic control is clear [38, 39]. Crow et al. suggested that binge eating behavior might exert little effect on weight control compared with purging behaviors like insulin omission [39].
With regards to other eating disturbances, diabetic patients showed higher scores on the Restraint Scale than obese non-diabetic patients, a difference that remained significant even after adjusting for age and BMI [40]. Furthermore, the higher the weight of diabetic patients the higher the level of eating and body awareness on psychological distress [41, 42]. In a follow-up study that examined eating disorder-related symptoms in type 2 diabetic patients after a 2-year period, the "drive for thinness" and the "body dissatisfaction" were significantly increased [45]. The authors suggested that the dieting-bingeing sequence proposed by Herman and Polivy [46] may also be applied to diabetic, especially obese diabetic, patients. Besides the social pressure on obese people to lose weight and, thus, conform to the Western norms of beauty and wellness, diabetics are expected to lose weight for alleviating the symptoms of their disease. As weight control expectations increase, body satisfaction, a keystone of self-esteem, decreases, enhancing the vicious cycle of restraint eating and bingeing.
Conclusion: is there anything to be changed?
Diabetes management is primarily behavioral, involving daily medication taking, glucose testing, exercise and nutrition-related actions [47]. The adoption of a healthy and balanced diet requires a series of behavioral changes in eating patterns with regards to meal planning, food selection, food preparation, dinning out, portion control, as well as appropriate responses to eating challenges. Dietary changes need to be consistent and applied to all lifestyle aspects. Diabetic patients receive a great amount of information and become very much concerned about their food intake, as one of the important means for managing their disease state. Guidance to conform to dietary recommendations is not often accompanied by the respective attention to behavioral factors in helping diabetics to adhere to multifaceted and demanding dietary regimes. Therefore, they exhibit restrictive behaviors with regards to food intake, express feelings of dietary deprivation and are convinced that rigid dietary control is the only way to diet and weight management. Dietary intervention needs to take into account these issues in order to improve its effectiveness. Patients are expected to discover and explore their personal responsibilities, while health professionals should shift from the concepts of compliance and adherence to the concept of collaboration (Figure 1) [17].
Brief measures of eating behaviors, dietary satisfaction and obstacles to following a dietary plan should be incorporated into the routine nutritional assessment of diabetic patients [48, 49], next to the traditional dietary assessment methods. They could be used to tailor intervention and assess outcomes apart from the nutrient or food intake changes. With regards to the nutritional approaches, research evidence has shown that nutrition advice given in the form of a simple meal plan emphasizing guidelines for healthy food choices is equally effective in producing changes in glycemic control as the traditional exchange-based dietary regime [50]. Success in nutrition therapy lies in the food choices that are made.
Nutrition education strategies should, therefore, be re-organized around individually tailored achievable goals in eating behavior and sequenced manageable steps regarding every day food choices and responses to problematic eating circumstances. A non-dieting approach or guidance for a flexible control of eating could induce the desirable changes in eating behavior and, consequently, glycemic control, without the "side effects" of dietary rigid restriction. The latter might be one of the causes of low adherence to the diet among diabetic patients (Figure 1).
References
- 1.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.Franz MJ, Bantle JP, Beebe CA, Brunzell JD, Chiasson JL, Garg A, Holzmeister LA, Hoogwerf B, Mayer-Davis E, Mooradian AD et al. Evidence-based nutrition principles and recommendations for the treatment and prevention of diabetes and related complications. Diabetes Care. 2002;25(1):148–198. doi: 10.2337/diacare.25.1.148. [DOI] [PubMed] [Google Scholar]
- 3.Monnier L, Grimaldi A, Charbonnel B, Iannascoli F, Lery T, Garofano A, Childs M. Management of French patients with type 2 diabetes mellitus in medical general practice: report of the Mediab observatory. Diabetes Metab. 2004;30(1):35–42. doi: 10.1016/s1262-3636(07)70087-3. [DOI] [PubMed] [Google Scholar]
- 4.Harris MI. Frequency of blood glucose monitoring in relation to glycemic control in patients with type 2 diabetes. Diabetes Care. 2001;24(6):979–982. doi: 10.2337/diacare.24.6.979. [DOI] [PubMed] [Google Scholar]
- 5.Saaddine JB, Cadwell B, Gregg EW, Engelgau MM, Vinicor F, Imperatore G, Narayan KM. Improvements in diabetes processes of care and intermediate outcomes: United States, 1988-2002. Ann Intern Med. 2006;144(7):465–474. doi: 10.7326/0003-4819-144-7-200604040-00005. [DOI] [PubMed] [Google Scholar]
- 6.Maizlish NA, Shaw B, Hendry K. Glycemic control in diabetic patients served by community health centers. Am J Med Qual. 2004;19(4):172–179. doi: 10.1177/106286060401900406. [DOI] [PubMed] [Google Scholar]
- 7.Azab AS. Glycemic control among diabetic patients. Saudi Med J. 2001;22(5):407–409. [PubMed] [Google Scholar]
- 8.Peyrot M, Rubin RR, Lauritzen T, Snoek FJ, Matthews DR, Skovlund SE. Psychosocial problems and barriers to improved diabetes management: results of the Cross-National Diabetes Attitudes, Wishes and Needs (DAWN) Study. Diabet Med. 2005;22(10):1379–1385. doi: 10.1111/j.1464-5491.2005.01644.x. [DOI] [PubMed] [Google Scholar]
- 9.Thanopoulou A, Karamanos B, Angelico F, Assaad-Khalil S, Barbato A, Del Ben M, Djordjevic P, Dimitrijevic-Sreckovic V, Gallotti C, Katsilambros N et al. Nutritional habits of subjects with Type 2 diabetes mellitus in the Mediterranean Basin: comparison with the non-diabetic population and the dietary recommendations. Multi-Centre Study of the Mediterranean Group for the Study of Diabetes (MGSD) Diabetologia. 2004;47(3):367–376. doi: 10.1007/s00125-003-1316-0. [DOI] [PubMed] [Google Scholar]
- 10.Glasgow RE, Hampson SE, Strycker LA, Ruggiero L. Personal-model beliefs and social-environmental barriers related to diabetes self-management. Diabetes Care. 1997;20(4):556–561. doi: 10.2337/diacare.20.4.556. [DOI] [PubMed] [Google Scholar]
- 11.Nelson KM, Reiber G, Boyko EJ. Diet and exercise among adults with type 2 diabetes: findings from the third national health and nutrition examination survey (NHANES III) Diabetes Care. 2002;25(10):1722–1728. doi: 10.2337/diacare.25.10.1722. [DOI] [PubMed] [Google Scholar]
- 12.Shimakawa T, Herrera-Acena MG, Colditz GA, Manson JE, Stampfer MJ, Willett WC, Stamper MJ. Comparison of diets of diabetic and nondiabetic women. Diabetes Care. 1993;16(10):1356–1362. doi: 10.2337/diacare.16.10.1356. [DOI] [PubMed] [Google Scholar]
- 13.Virtanen SM, Feskens EJ, Rasanen L, Fidanza F, Tuomilehto J, Giampaoli S, Nissinen A, Kromhout D. Comparison of diets of diabetic and non-diabetic elderly men in Finland, The Netherlands and Italy. Eur J Clin Nutr. 2000;54(3):181–186. doi: 10.1038/sj.ejcn.1600916. [DOI] [PubMed] [Google Scholar]
- 14.Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanadis C. The epidemiology of Type 2 diabetes mellitus in Greek adults: the ATTICA study. Diabet Med. 2005;22(11):1581–1588. doi: 10.1111/j.1464-5491.2005.01731.x. [DOI] [PubMed] [Google Scholar]
- 15.Guare JC, Wing RR, Grant A. Comparison of obese NIDDM and nondiabetic women: short- and long-term weight loss. Obes Res. 1995;3(4):329–335. doi: 10.1002/j.1550-8528.1995.tb00158.x. [DOI] [PubMed] [Google Scholar]
- 16.Gauthier-Chelle K, Mennen L, Arnault N, Rigalleau V, Hercberg S, Gin H. Comparison of the diet of self-declared diabetics with non-diabetic patients in the SU.VI.MAX study: did the diabetics modify their nutritional behavior? Diabetes Metab. 2004;30(6):535–542. doi: 10.1016/s1262-3636(07)70152-0. [DOI] [PubMed] [Google Scholar]
- 17.Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26(4):597–604. doi: 10.1177/014572170002600405. [DOI] [PubMed] [Google Scholar]
- 18.Mela DJ. Food choice and intake: the human factor. Proc Nutr Soc. 1999;58(3):513–521. doi: 10.1017/s0029665199000683. [DOI] [PubMed] [Google Scholar]
- 19.Savoca M, Miller C. Food selection and eating patterns: themes found among people with type 2 diabetes mellitus. J Nutr Educ. 2001;33(4):224–233. doi: 10.1016/s1499-4046(06)60035-3. [DOI] [PubMed] [Google Scholar]
- 20.Savoca MR, Miller CK, Ludwig DA. Food habits are related to glycemic control among people with type 2 diabetes mellitus. J Am Diet Assoc. 2004;104(4):560–566. doi: 10.1016/j.jada.2004.01.013. [DOI] [PubMed] [Google Scholar]
- 21.Schmidt LE, Rost KM, McGill JB, Santiago JV. The relationship between eating patterns and metabolic control in patients with non-insulin-dependent diabetes mellitus (NIDDM) Diabetes Educ. 1994;20(4):317–321. doi: 10.1177/014572179402000410. [DOI] [PubMed] [Google Scholar]
- 22.Snoek FJ. Barriers to good glycaemic control: the patient's perspective. Int J Obes Relat Metab Disord. 2000;24(Suppl 3):S12–S20. doi: 10.1038/sj.ijo.0801421. [DOI] [PubMed] [Google Scholar]
- 23.Brown SL, Pope JF, Hunt AE, Tolman NM. Motivational strategies used by dietitians to counsel individuals with diabetes. Diabetes Educ. 1998;24(3):313–318. doi: 10.1177/014572179802400305. [DOI] [PubMed] [Google Scholar]
- 24.Travis T. Patient perceptions of factors that affect adherence to dietary regimens for diabetes mellitus. Diabetes Educ. 1997;23(2):152–156. doi: 10.1177/014572179702300205. [DOI] [PubMed] [Google Scholar]
- 25.Schlundt DG, Rea MR, Kline SS, Pichert JW. Situational obstacles to dietary adherence for adults with diabetes. J Am Diet Assoc. 1994;94(8):874–876. doi: 10.1016/0002-8223(94)92367-1. [DOI] [PubMed] [Google Scholar]
- 26.El-Kebbi IM, Bacha GA, Ziemer DC, Musey VC, Gallina DL, Dunbar V, Phillips LS. Diabetes in urban African Americans. V. Use of discussion groups to identify barriers to dietary therapy among low-income individuals with non-insulin-dependent diabetes mellitus. Diabetes Educ. 1996;22(5):488–492. doi: 10.1177/014572179602200508. [DOI] [PubMed] [Google Scholar]
- 27.Peres DS, Franco LJ, Santos MA. Eating behavior among type 2 diabetes women. Rev Saude Publica. 2006;40(2):310–317. doi: 10.1590/s0034-89102006000200018. [DOI] [PubMed] [Google Scholar]
- 28.Samuel-Hodge CD, Headen SW, Skelly AH, Ingram AF, Keyserling TC, Jackson EJ, Ammerman AS, Elasy TA. Influences on day-to-day self-management of type 2 diabetes among African-American women: spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23(7):928–933. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 29.Westenhoefer J, Broeckmann P, Munch AK, Pudel V. Cognitive control of eating behaviour and the disinhibition effect. Appetite. 1994;23(1):27–41. doi: 10.1006/appe.1994.1032. [DOI] [PubMed] [Google Scholar]
- 30.Black AE, Coward WA, Cole TJ, Prentice AM. Human energy expenditure in affluent societies: an analysis of 574 doubly-labelled water measurements. Eur J Clin Nutr. 1996;50(2):72–92. [PubMed] [Google Scholar]
- 31.Livingstone MB, Black AE. Markers of the validity of reported energy intake. J Nutr. 2003;133(Suppl 3):895S–920S. doi: 10.1093/jn/133.3.895S. [DOI] [PubMed] [Google Scholar]
- 32.Martin GS, Tapsell LC, Denmeade S, Batterham MJ. Relative validity of a diet history interview in an intervention trial manipulating dietary fat in the management of Type II diabetes mellitus. Prev Med. 2003;36(4):420–428. doi: 10.1016/s0091-7435(02)00054-3. [DOI] [PubMed] [Google Scholar]
- 33.Samuel-Hodge CD, Fernandez LM, Henriquez-Roldan CF, Johnston LF, Keyserling TC. A comparison of self-reported energy intake with total energy expenditure estimated by accelerometer and basal metabolic rate in African-American women with type 2 diabetes. Diabetes Care. 2004;27(3):663–669. doi: 10.2337/diacare.27.3.663. [DOI] [PubMed] [Google Scholar]
- 34.Yannakoulia M, Panagiotakos DB, Pitsavos C, Stefanadis C. Correlates of BMI misreporting among apparently healthy individuals: the ATTICA study. Obes. Res doi: 10.1038/oby.2006.103. [DOI] [PubMed] [Google Scholar]
- 35.Mannucci E, Rotella F, Ricca V, Moretti S, Placidi GF, Rotella CM. Eating disorders in patients with type 1 diabetes: a meta-analysis. J Endocrinol Invest. 2005;28(5):417–419. doi: 10.1007/BF03347221. [DOI] [PubMed] [Google Scholar]
- 36.Colton P, Olmsted M, Daneman D, Rydall A, Rodin G. Disturbed eating behavior and eating disorders in preteen and early teenage girls with type 1 diabetes: a case-controlled study. Diabetes Care. 2004;27(7):1654–1659. doi: 10.2337/diacare.27.7.1654. [DOI] [PubMed] [Google Scholar]
- 37.Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: cross sectional study. BMJ. 2000;320(7249):1563–1566. [PMC free article] [PubMed] [Google Scholar]
- 38.Rydall AC, Rodin GM, Olmsted MP, Devenyi RG, Daneman D. Disordered eating behavior and microvascular complications in young women with insulin-dependent diabetes mellitus. N Engl J Med. 1997;336(26):1849–1854. doi: 10.1056/NEJM199706263362601. [DOI] [PubMed] [Google Scholar]
- 39.Crow S, Kendall D, Praus B, Thuras P. Binge eating and other psychopathology in patients with type II diabetes mellitus. Int J Eat Disord. 2001;30(2):222–226. doi: 10.1002/eat.1077. [DOI] [PubMed] [Google Scholar]
- 40.Mannucci E, Tesi F, Ricca V, Pierazzuoli E, Barciulli E, Moretti S, Di Bernardo M, Travaglini R, Carrara S, Zucchi T et al. Eating behavior in obese patients with and without type 2 diabetes mellitus. Int J Obes Relat Metab Disord. 2002;26(6):848–853. doi: 10.1038/sj.ijo.0801976. [DOI] [PubMed] [Google Scholar]
- 41.Kenardy J, Mensch M, Bowen K, Green B, Walton J, Dalton M. Disordered eating behaviours in women with Type 2 diabetes mellitus. Eat Behav. 2001;2(2):183–192. doi: 10.1016/s1471-0153(01)00028-9. [DOI] [PubMed] [Google Scholar]
- 42.Herpertz S, Albus C, Lichtblau K, Kohle K, Mann K, Senf W. Relationship of weight and eating disorders in type 2 diabetic patients: a multicenter study. Int J Eat Disord. 2000;28(1):68–77. doi: 10.1002/(sici)1098-108x(200007)28:1<68::aid-eat8>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 43.Herpertz S, Albus C, Wagener R, Kocnar M, Wagner R, Henning A, Best F, Foerster H, Schulze Schleppinghoff B, Thomas W et al. Comorbidity of diabetes and eating disorders. Does diabetes control reflect disturbed eating behavior? Diabetes Care. 1998;21(7):1110–1116. doi: 10.2337/diacare.21.7.1110. [DOI] [PubMed] [Google Scholar]
- 44.Kenardy J, Mensch M, Bowen K. Self-reported dieting and weight histories of newly diagnosed NIDDM patients. Int J Obes Relat Metab Disord. 1996;20(1):88–90. [PubMed] [Google Scholar]
- 45.Herpertz S, Albus C, Kielmann R, Hagemann-Patt H, Lichtblau K, Kohle K, Mann K, Senf W. Comorbidity of diabetes mellitus and eating disorders: a follow-up study. J Psychosom Res. 2001;51(5):673–678. doi: 10.1016/s0022-3999(01)00246-x. [DOI] [PubMed] [Google Scholar]
- 46.Polivy J, Herman CP. Dieting and binging. A causal analysis. Am Psychol. 1985;40(2):193–201. doi: 10.1037//0003-066x.40.2.193. [DOI] [PubMed] [Google Scholar]
- 47.Glasgow RE, Fisher EB, Anderson BJ, LaGreca A, Marrero D, Johnson SB, Rubin RR, Cox DJ. Behavioral science in diabetes. Contributions and opportunities. Diabetes Care. 1999;22(5):832–843. doi: 10.2337/diacare.22.5.832. [DOI] [PubMed] [Google Scholar]
- 48.Glasgow RE, Perry JD, Toobert DJ, Hollis JF. Brief assessments of dietary behavior in field settings. Addict Behav. 1996;21(2):239–247. doi: 10.1016/0306-4603(95)00056-9. [DOI] [PubMed] [Google Scholar]
- 49.Ahlgren SS, Shultz JA, Massey LK, Hicks BC, Wysham C. Development of a preliminary diabetes dietary satisfaction and outcomes measure for patients with type 2 diabetes. Qual Life Res. 2004;13(4):819–832. doi: 10.1023/B:QURE.0000021694.59992.a1. [DOI] [PubMed] [Google Scholar]
- 50.Ziemer DC, Berkowitz KJ, Panayioto RM, El-Kebbi IM, Musey VC, Anderson LA, Wanko NS, Fowke ML, Brazier CW, Dunbar VG et al. A simple meal plan emphasizing healthy food choices is as effective as an exchange-based meal plan for urban African Americans with type 2 diabetes. Diabetes Care. 2003;26(6):1719–1724. doi: 10.2337/diacare.26.6.1719. [DOI] [PubMed] [Google Scholar]


